Abstract
Aims: The present study aimed to compare the long-term (five-year) safety and efficacy between the one-stent, two-stent and double-kissing (DK) crush strategies, utilising drug-eluting stents, for unprotected left main coronary artery (ULMCA) bifurcation lesions.
Methods and results: Between March 2004 and April 2007, 633 consecutive patients with ULMCA bifurcation lesions (232 in the one-stent group and 401 in the two-stent group) were prospectively enrolled. The primary endpoint was the occurrence of major adverse cardiac events (MACE), a composite of cardiac death, myocardial infarction (MI), and target vessel revascularisation (TVR), at five-year follow-up. Patients in the the two-stent group were classified as DK crush (n=155) and other two-stent techniques (culotte, T-stenting, kissing stenting and classical crush, n=246). Forty-seven (16.8%) patients in the one-stent group crossed over to the two-stent group. The one-stent group was associated with an increased incidence of MI compared to the two-stent approach (10.5% vs. 5.5%, p=0.025). The crude rate of MACE at five years was 28.0% in the one-stent group and 28.4% in the two-stent group (p=0.927). DK crush was associated with a significantly decreased five-year MACE compared to the other two-stent approaches or the one-stent approach (DK crush: 14.8% vs. other two-stent approaches: 37.0%, one-stent approach: 28.0%, p<0.001). The main benefit of DK crush primarily appeared to be secondary to a reduction in TVR (7.7% vs. 30.5% vs. 18.1%, p<0.001). By Cox regression analyses, the non-DK crush two-stent technique, a high SYNTAX Score (≥33) or New Risk Stratification (NERS) score (>20), and incomplete revascularisation were shown to be independent predictors of MACE at five-year follow-up.
Conclusions: With distal left main true bifurcations, the two-stent technique (excluding DK crush) is an independent predictor of long-term MACE. DK crush is associated with more favourable long-term clinical outcomes. Confirmation of these findings is required from randomised controlled trials.
Introduction
With the extensive off-label use of drug-eluting stents (DES) for obstructive coronary artery disease, the interest in stenting unprotected left main coronary artery disease (ULMCA) has increased rapidly1,2. The ACC/AHA guidelines recently updated recommendations for percutaneous coronary intervention (PCI) of ULMCA disease from class III to II(b), and class I(b) for coronary artery bypass graft (CABG), compared to I(a) in previous guidelines1,3. ULMCA bifurcation lesions nevertheless represent a technical challenge for the interventional cardiologist, with ULMCA bifurcation lesions being previously shown to be an independent predictor of major adverse cardiac events (MACE) during one to three-year clinical follow-up, predominantly secondary to repeat revascularisation1,2,4-6. In addition, several studies have suggested that the two-stent techniques for distal ULMCA bifurcation lesions do not provide any additional advantages compared to the one-stent technique, and may even be detrimental4-7. None of these studies has, however, included a three-year clinical follow-up to assess potential long-term differences in two-stent techniques. Furthermore, the DK crush technique, as a novel two-stent strategy in the setting of ULMCA disease, has not currently been reported directly. The DK crush technique has been shown to lead to increased procedural success8-10, with clinical results at least comparable to the one-stent approach, and a reduced incidence of repeat revascularisation, compared to the one-stent (provisional T-stenting) technique, for unselected non-left main bifurcation lesions11. The aim of the present study was to compare the five-year safety and efficacy between the one-stent, two-stent and DK crush strategies, with the hypothesis that DK crush may offer superior clinical outcomes compared to other two-stent strategies (including culotte, T-stenting, kissing stenting and classical crush), and possibly to a one-stent strategy for ULMCA bifurcation lesions.
Methods
STUDY POPULATION
Between March 2004 and April 2007, a total of 1,156 patients with ULMCA in eight Chinese medical centres were screened (Figure 1). Of these, 767 (66.3%) patients had distal lesions, and 650 had true bifurcation or trifurcation lesions classified by Medina classification (1,1,1; 1,0,1; 0,1,1)12. Among the 650 bifurcation or trifurcation lesions, 10 patients received medical therapy alone and seven underwent CABG. Of the remaining 633 patients, the one-stent technique was scheduled in 279 patients, 47 (16.9%) of whom crossed over to the two-stent group because of suboptimal results in the left circumflex after crossover left main (left anterior descending - LAD) stenting. In total, 232 patients were included in the one-stent group and 401 patients in the two-stent group.
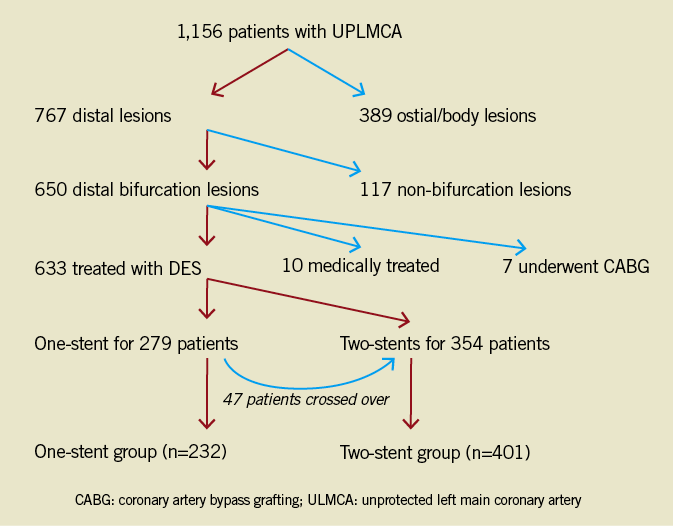
Figure 1. Study flow chart. CABG: coronary artery bypass grafting; ULMCA: unprotected left main coronary artery
INCLUSION/EXCLUSION CRITERIA
The clinical inclusion criteria were the presence of angina, documented ischaemia and/or acute myocardial infarction (AMI). The exclusion criteria were the presence of any graft to a native coronary artery and a life expectancy less than three months. Bare metal stents for any lesions were prohibited.
All candidates, or their legally authorised representatives, were invited to participate in the discussion with the whole clinical team (including the cardiologist, cardiac surgeons and the hospital accountant) and were informed that: 1) CABG was the gold-standard treatment for ULMCA, and that the implantation of DES was an option under investigation for ULMCA; 2) a lack of blood supply to the left myocardium during left main stenting was associated with the possibility of cardiac death; 3) complete revascularisation by PCI is only achieved in some patients, and incomplete revascularisation would potentially place patients at high risk; and 4) the patient would pay a portion of the estimated intraprocedural costs for either PCI (according to complete or incomplete revascularisation and either a one-stent or two-stent strategy) or CABG (according to complete revascularisation). After agreement between the medical team and the patient had been achieved, written informed consent was obtained. All patients who would undergo PCI were enrolled in this study. Patients undergoing CABG or medical treatment alone were prospectively included in another database. The current study was approved by all participating centres’ local ethics committees. In addition, the institutional review board approved the use of clinical data for this study.
INTERVENTIONAL PROCEDURE AND PERIPROCEDURAL MEDICATIONS
The stenting technique was chosen at the operator’s discretion. A one-stent technique was defined as a stent crossover technique (from LAD to left main) with a safety coronary wire jailed in the left circumflex coronary artery (LCX), followed by kissing balloon dilatation if there was >50% diameter stenosis, by visual estimation, at the ostial LCX. An additional stent was required for the LCX ostium if any of the following issues was observed after kissing balloon inflation: residual diameter stenosis >70%, >type B dissection or thrombolysis in myocardial infarction (TIMI) flow <3. Two-stent techniques used in this study included DK crush, culotte, T-stenting, kissing stenting, and classical crush.10-17 Two non-compliant balloons inflated at ≥16 atm were used for all final kissing balloon inflations. Pre-procedural intravascular ultrasound (IVUS) assessment and the use of platelet glycoprotein IIb/IIIa inhibitors was left to the physician’s discretion.
Sirolimus-eluting stents (Firebird™, MicroPort Co., Shanghai, China18; Excel™, Jiwei Medical, Shandong, China19,20; CYPHER™, Cordis, Johnson & Johnson, Miami, FL, USA) and a paclitaxel-eluting stent (TAXUS™, Boston Scientific, Natick, MA, USA) were used. DES selection and staged procedures were left to the operator’s discretion.
Before the data analysis was performed, all patients were classified into two prespecified groups according to the final stenting technique: one-stent group and two-stent (DK crush and other two-stent techniques) group.
All patients were pretreated with aspirin and clopidogrel. A 300 mg loading dose of clopidogrel was administered before the index procedure if the patient was not pretreated. Intravenous unfractionated heparin was used to maintain an activated clotting time between 250 and 300 seconds throughout the procedure. After the intervention, all patients received 300 mg/day aspirin for one month. Thereafter, they received 100 mg/day indefinitely for life. Clopidogrel (75 mg/d) was continued for at least 12 months, along with other medications according to the judgement of the patient’s physician.
QUANTITATIVE CORONARY ANGIOGRAPHY (QCA) ANALYSIS AND RISK SCORING
Matched orthogonal views after intracoronary injection of nitroglycerine (100-200 µg) were used for QCA pre-procedurally, post-procedurally and at follow-up. Coronary angiograms were analysed offline with a validated, automated edge-detection, 2-D coronary bifurcation system (CAAS version 5.9.2; Pie Medical Imaging, Maastricht, The Netherlands), by two independent experienced operators in an angiographic core laboratory (CCRF [China Cardiovascular Research Foundation], Beijing, China) unaware of the treatment allocation. Vessel segments involving bifurcation lesions were divided into proximal main vessel (MV), distal MV, and side branch (SB). QCA variables included reference vessel diameter (RVD), minimal lumen diameter (MLD), late lumen loss (LLL), and distal bifurcation angle (defined as the angle between distal MV and SB). Downstream lesions in the LAD or LCX were defined as lesions at least 5 mm distal to the left main bifurcation lesions. ULMCA was defined as the absence of any vessel anastomosed with a bypass graft. The ULMCA lesions were classified as ostial (lesions located within 3 mm of the LMCA ostium), midshaft (lesions located in the middle portion of the LMCA, with at least 3 mm of apparently lesion-free artery before the take-off of LAD and LCX), and distal bifurcation lesions (lesions involving the ostial LAD and LCX). Distal ULMCA trifurcation (lesions involving the ostial LAD, LCX and ramus intermedius if the latter diameter was >2.0 mm) were also included in the enrolment. The SYNTAX Score (http://www.syntaxscore.com) was retrospectively calculated by two independent experienced operators, blinded to treatment assignment and clinical outcomes as previously described21,22. In addition, the New Risk Stratification (NERS) score was calculated, as previously described (http://www.nersscore.com)23.
STUDY ENDPOINTS AND DEFINITIONS
The primary outcome of interest was the occurrence of MACE, a composite of cardiac death, myocardial infarction (MI), and target vessel revascularisation (TVR). Secondary angiographic endpoints were binary in-stent restenosis (ISR) and LLL in the MV or SB at eight months. The rate of definite stent thrombosis (ST) served as a safety endpoint. MI was diagnosed if the plasma level of creatine kinase (CK)-MB/troponin increased to ≥3 times the upper normal limit in no fewer than two blood samples.24 All deaths were considered as cardiac in origin unless non-cardiac reasons were indicated. Target lesion revascularisation (TLR) and TVR were defined as any repeat revascularisation (PCI or coronary artery bypass grafting [CABG]) for target lesions and target vessels, respectively, in the presence of symptoms or objective signs of ischaemia. ST was defined according to the Academic Research Consortium (ARC) definition25,26. Angiographic binary ISR was defined as diameter stenosis >50% measured by QCA. The LLL was defined as the difference between post-procedural and follow-up MLD. Angiographic success in ULMCA bifurcation lesions was defined as the achievement of TIMI grade 3 and residual stenosis of <20% in both the MV and SB. Angiographic complete revascularisation was defined as any attempt to revascularise all diseased segments (≥2.5 mm in diameter) during the index hospitalisation or within 30 days after the index procedure, but before a new MI or urgent TLR.
FOLLOW-UP PROTOCOL
Total creatine kinase (CK), creatine kinase and myoglobin (CK-MB), and cardiac troponin I were measured every eight hours for the first 24 hours after the procedure and daily thereafter before discharge from hospital. Clinical follow-up was performed with office visits or telephone contact at one, six, and 12 months, and once yearly thereafter. Adverse events were monitored throughout the entire study period. A follow-up coronary angiography was scheduled at eight months after the index procedure unless it was performed earlier for clinical reasons. All data were collected and entered into a dedicated computer database by specialised personnel of the Clinical Data Management Centre. Event committees in each medical centre, blinded to treatment allocation, adjudicated all adverse clinical events.
STATISTICAL ANALYSIS
The treatment group differences of continuous variables were expressed as mean ± standard deviation and compared with the Student’s t-test or Wilcoxon rank-sum test scores where appropriate. Categorical variables are reported as percentages and compared with the χ2 test or Fisher’s exact test. Event-free survival rates were generated by Kaplan-Meier analysis and compared using a log-rank test. To determine predictors of MACE at five-year follow-up, clinical, angiographic and procedural variables were analysed using multivariable Cox proportional hazards forward stepwise regression analyses. The following variables considered as possible predictors were included for analyses: age, gender, diabetes, current smoker, hypertension and hyperlipidaemia, prior history of MI or PCI, unstable angina, acute MI, ejection fraction (EF) <30%, peripheral arterial disease, SYNTAX Score or NERS score (there was significant interaction between these two scores for five-year follow-up MACE, interaction p-value <0.05), stent type (SES/PES), diseased vessel number, downstream lesions, lesion sites in left main coronary artery, bifurcation angle, chronic total occlusion, transfemoral or transradial approach, stent strategies for LM bifurcation, total stent number, total stent length, incomplete revascularisation, IVUS guidance, final kissing inflation. Statistical significance was defined with a two-sided p-value <0.05. All analyses were performed with the statistical programme SPSS 16.0 (SPSS Institute Inc., Chicago, IL, USA).
Results
BASELINE CHARACTERISTICS
The baseline clinical characteristics of the patients are summarised in Table 1. Notably, patients in the one-stent group had more frequent acute myocardial infarction (25.8%), congestive heart failure (31.5%) and left ventricular EF <30% (7.8%) compared to the two-stent group (16.7%, p=0.016, 23.4%, p=0.049, 2.5%, p=0.022, respectively).
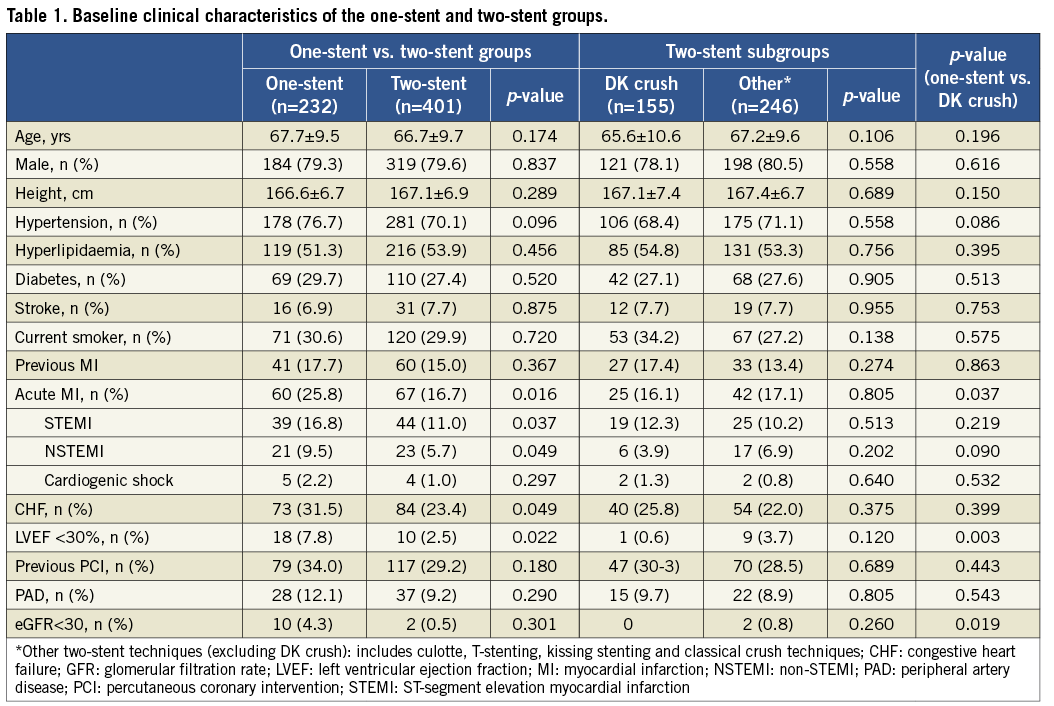
The lesion characteristics are shown in Table 2. Patients in the one-stent group had more complex non-left main coronary artery disease compared to the two-stent group, as evidenced by a significantly higher SYNTAX Score (39.2±15.8 vs. 34.5±16.1 in the two-stent group, p<0.001), more chronic total occlusions (CTOs), and more severe calcification.
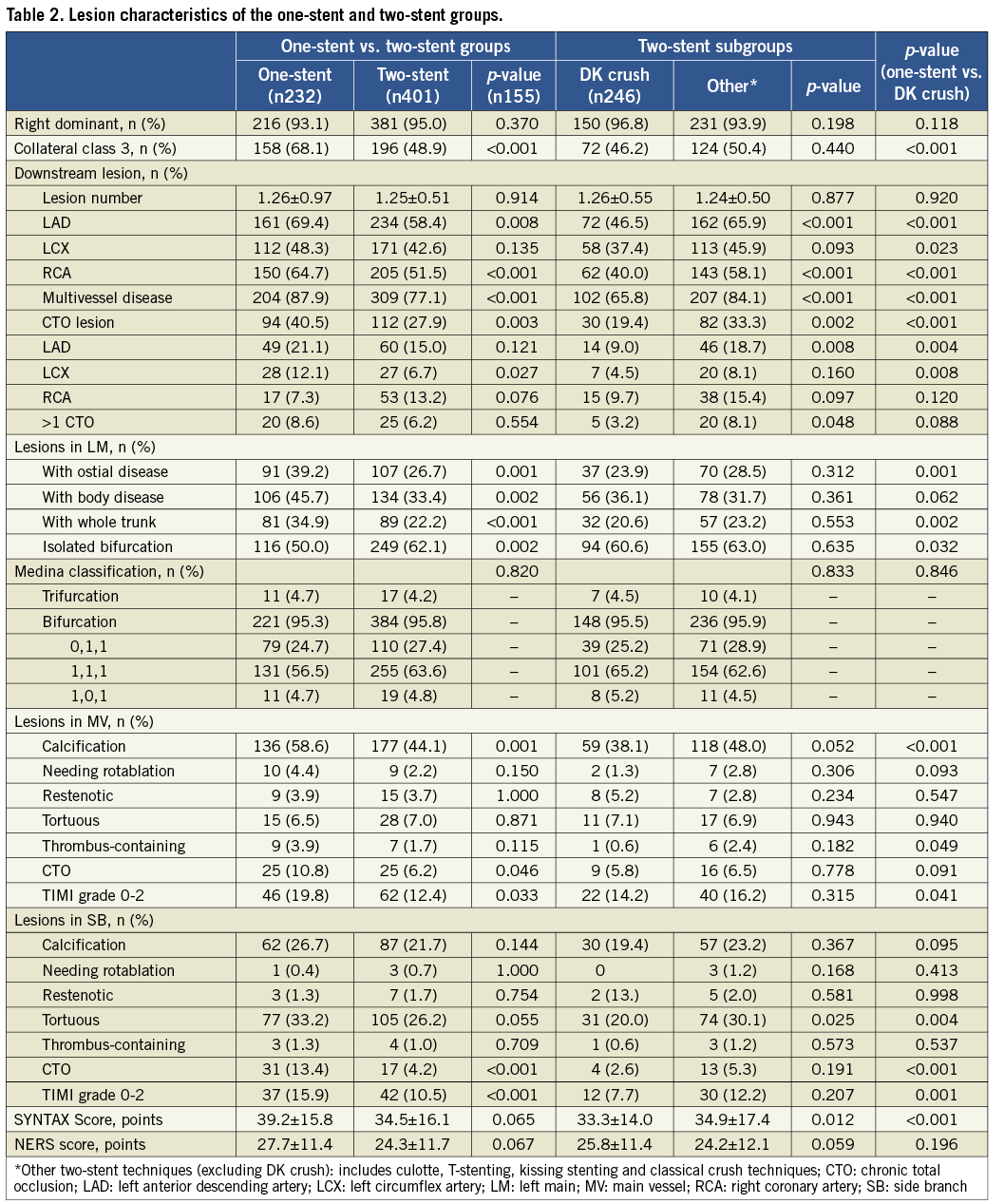
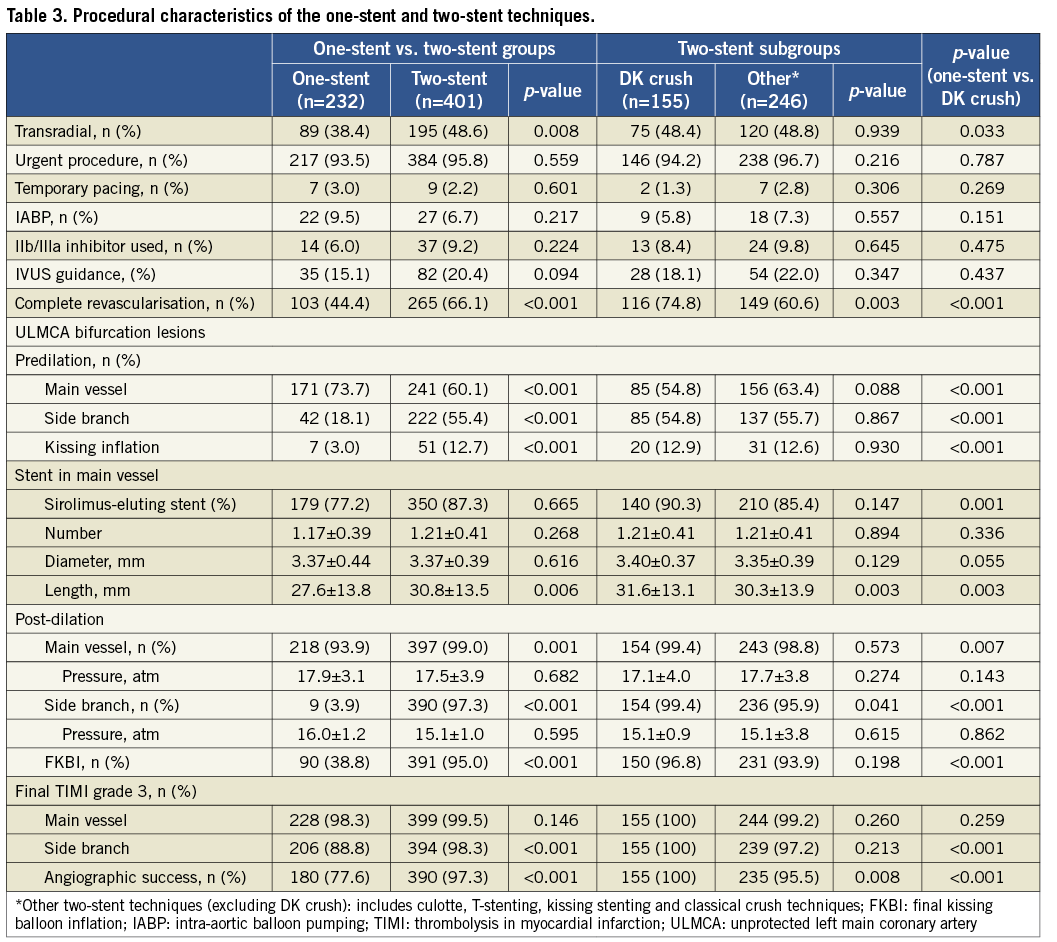
Table 3 shows the angiographic and procedural characteristics of the distal left main bifurcation lesion in the study groups. Stent length in MV was 30.8±13.5 mm in the two-stent group, significantly longer than that measured in the one-stent group (27.6±13.8 mm, p=0.006). The rate of TIMI grade 3 flow in the side branch, and the incidence of angiographic success in ULMCA bifurcation lesions, was 88.8% and 77.6%, respectively, in the one-stent group, compared to 98.3% and 97.3%, respectively in the two-stent group (both, p<0.001). The incidence of complete revascularisation for all diseased coronary segments (defined as ≥2.5 mm in diameter) was significantly higher in the two-stent group compared to the one-stent group (66.1% vs. 44.4%, p<0.001).
ANGIOGRAPHIC FOLLOW-UP
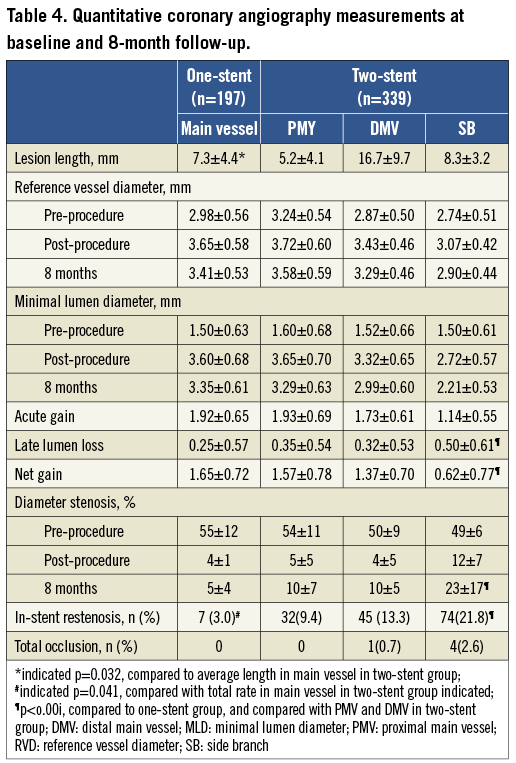
Overall, follow-up angiography was performed in 536 patients (84.7%): 197 in the one-stent group (84.9%) and 339 in the two-stent group (84.5%) (Table 4). The average lesion length in MV in the two-stent group was longer. The LLL and net gain in MV in the one-stent group were 0.25±0.57 mm and 1.65±0.72 mm. By comparison, in the two-stent group, the LLL and net gain were significantly greater (p<0.05) in the proximal MV (0.35±0.54 mm and 1.57±0.78 mm), distal MV (0.32±0.53 mm and 1.37±0.70 mm), and SB (0.50±0.61 mm and 0.62±0.77 mm). This resulted in a higher rate of binary ISR in the MV (11.35%, p=0.041) and SB (21.8%, p<0.001) in the two-stent group.
CRUDE ANALYSIS OF CLINICAL OUTCOMES
The crude rates of clinical outcomes are listed in Table 5. There were 65 MACE (28.0%) at five years in the one-stent group compared to 114 MACE (28.4%, p=0.927) in the two-stent group (Figure 2). The DK crush was associated with a lower incidence of MACE compared to the one-stent technique (14.8% vs. 28.0%, p=0.002); conversely, the other two-stent techniques (excluding DK crush) were associated with a higher incidence of five-year MACE compared to the one-stent technique (37.0% vs. 28.0%, p=0.059) (Figure 2). Further analyses indicated that cardiac death, MI, and TVR were significantly lower in the DK crush group (Figure 3).
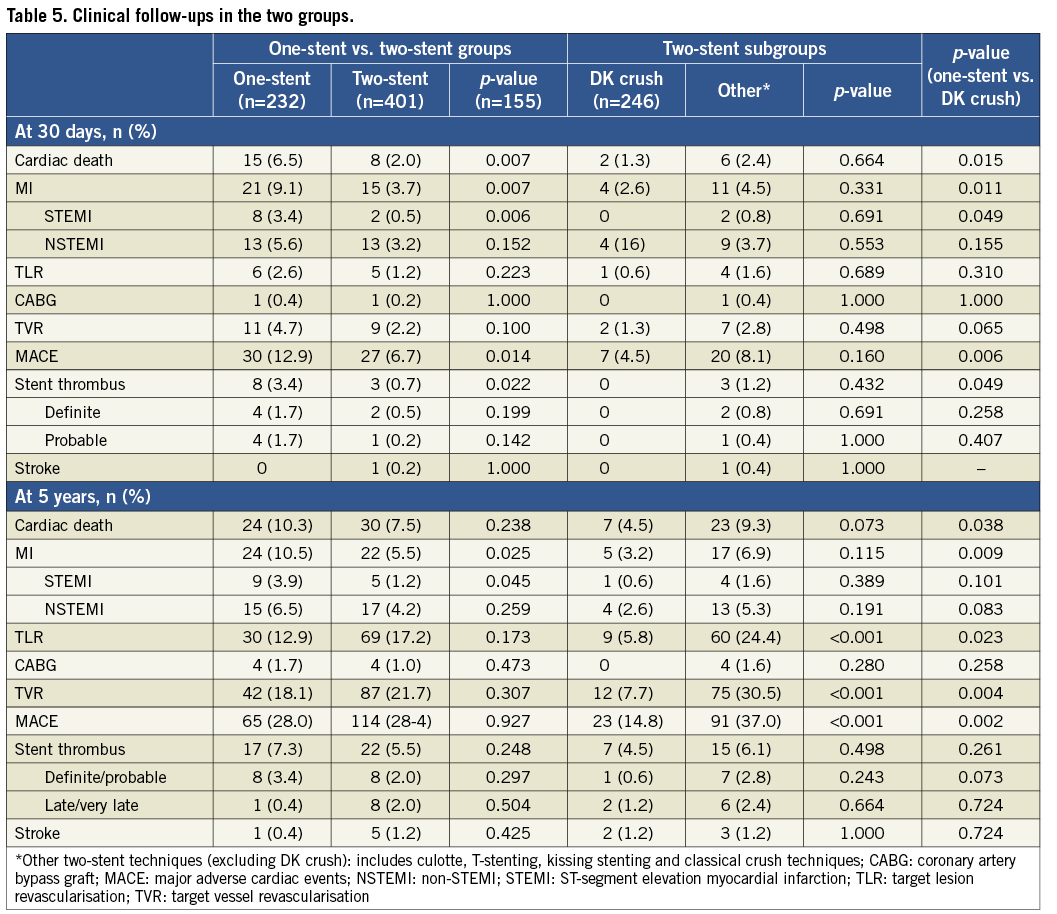
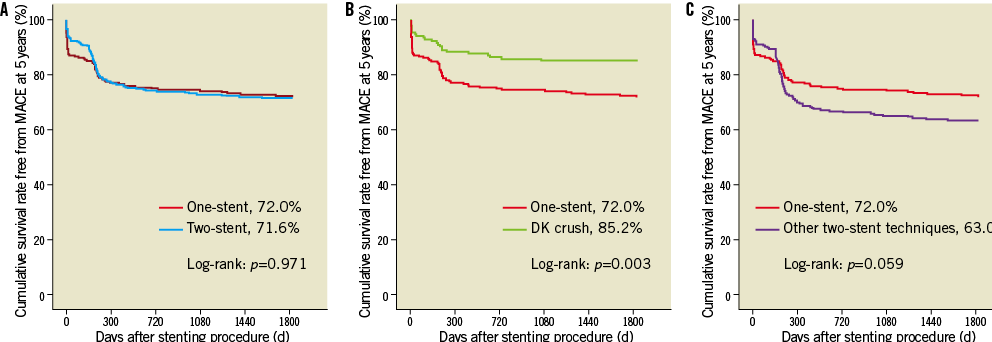
Figure 2. Comparison of crude MACE-free survival rates at 5-year follow-up. (A) 5-year MACE: one-stent vs. two-stent, (B) 5-year MACE: one-stent vs. DK crush, (C) 5-year MACE: one-stent vs. other two-stent techniques (including culotte, T-stenting, kissing and classical crush stenting techniques); MACE: major adverse cardiac events
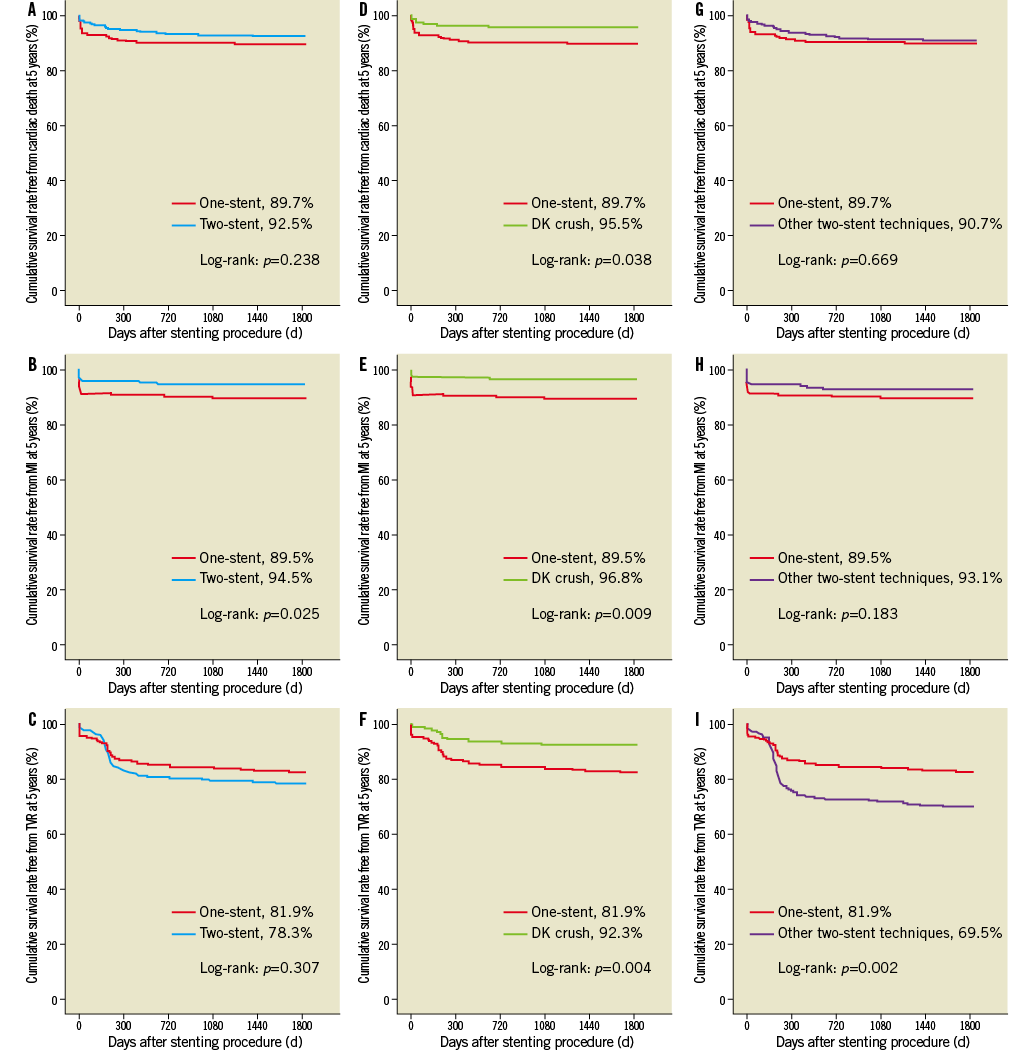
Figure 3. Comparison of crude survival rates free from cardiac death, myocardial infarction, and target vessel revascularisation at 5-year follow-up. (A, B, C) 5-year cardiac death, MI and TVR: one-stent vs. two-stent; (D, E, F) 5-year cardiac death, MI and TVR: one-stent vs. DK crush; (G, H, I) 5-year cardiac death, MI and TVR: one-stent vs. other two-stent techniques (including culotte, T-stenting, kissing and classical crush stenting techniques). MACE: major adverse cardiac events
By Cox regression analysis, we determined that a high SYNTAX Score (≥33, HR: 1.773, 95% CI: 1.298-2.422, p<0.001) or NERS score >20 (HR: 1.623, 95% CI: 1.109-2.878, p=0.005), the non-DK crush two-stent technique (HR: 0.589, 95% CI: 0.349-0.996, p=0.048) and incomplete revascularisation (HR: 2.330, 95% CI: 1.334-4.069, p=0.003) were independent predictors of MACE at five-year follow-up.
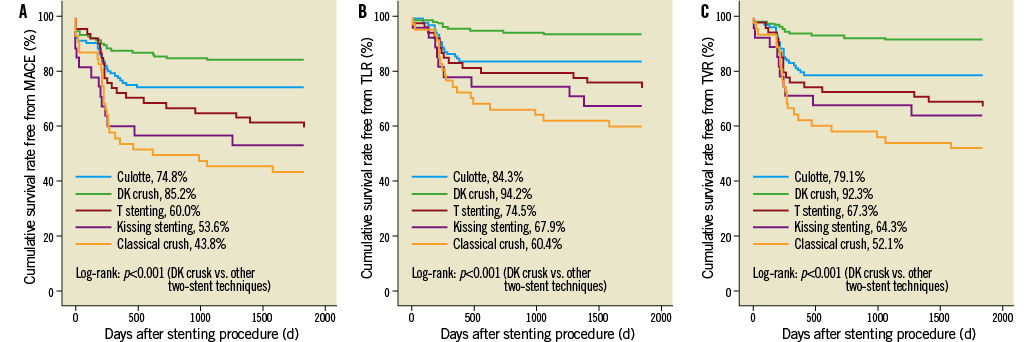
Figure 4. Comparison of crude survival rates free from (A) MACE, (B) TLR, and (C) TVR at 5 years between DK crush and other two-stent techniques (including culotte, T-stenting, kissing and classical crush stenting techniques). MACE: major adverse cardiac events; TLR: target lesion revascularisation; TVR: target vessel revascularisation
Discussion
The major findings of the current study are that: 1) among patients undergoing two-stent techniques for distal left main bifurcation lesions, DK crush stenting was associated with the lowest incidence of MACE and repeat revascularisation over a five-year period; and 2) DK crush appeared to have comparable or more favourable long-term clinical outcomes compared to the one-stent approach.
ONE-STENT VS. TWO-STENT TECHNIQUES
Distal left main bifurcation lesions account for >50% of patients with left main coronary artery involvement4-6. DES placement in this lesion subset remains challenging4,5,7. The one-stent technique to treat this challenging lesion subset has been shown to lead to more favourable outcomes compared to the two-stent technique4,5,27-29. The CACTUS and DKCRUSH-II studies reported approximately 30% crossover rates from the one-stent to the two-stent approach when bifurcation lesions were localised in coronary vessels outside the left main11,14. In the current study, this crossover rate was 16.9%, similar to the 20% reported in the LEMAX (Left Main XIENCE V) study30, but lower compared to the 28% reported in the FRIEND study31, and the 51.5% reported in the SYNTAX-LEMANS study32. Interestingly, non-final kissing balloon inflation (FKBI), a known predictor of clinical events after complex stenting for bifurcation lesions, was an independent risk factor for STEMI at 30 days in the present study4,5,11,14. Conversely, the FKBI rate was 38.8% in the one-stent group in the present study, which was lower than that in previous studies5,6,31. The impact of FKBI on clinical outcome after the one-stent technique for ULMCA distal bifurcation lesions has, however, remained undefined. Lehmann et al recently reported that single-stent PCI, involving distal ULMCA bifurcation lesions without SB intervention, was possibly associated with higher long-term mortality33, which is in contrast to the randomised NORDIC-Baltic Bifurcation Study III for bifurcation lesions localised in coronary vessels outside the left main34.
SUBGROUP ANALYSIS OF TWO-STENT TECHNIQUES
Two-stent techniques were mainly used based on the following considerations: 1) complex anatomical features of the distal left main coronary artery; 2) unacceptable severe stenosis in the LCX ostium post crossover left main-LAD stenting; 3) need for full coverage of the LCX ostium; and 4) to avoid acute closure of the LCX. Similar to other studies investigating ULMCA PCI4,5,28,35, the two-stent technique was chosen at the operator’s discretion according to anatomy and the operator’s experience.
In addition, in the ULMCA bifurcation lesions, several studies have reported that the two-stent strategies may potentially be associated with adverse clinical outcomes29,35,38. In the present study, the other two-stent strategies (excluding DK crush) were consistent with all these findings, showing a trend towards a higher incidence of MACE at five-year follow-up. However, in the global population, the long-term clinical outcomes in the two-stent techniques were comparable to the one-stent technique, which appeared to be attributable to the application of the DK crush technique. DK crush is a novel technique that has been shown to increase substantially the likelihood of FKBI and procedural success, with a subsequent reported significant reduction in TLR and TVR in unselected bifurcation lesions, compared to a simple stent strategy11. In this study, DK crush was associated with the lowest rates of TLR, TVR and MACE, suggesting that DK crush may potentially be superior to other two-stent techniques, and possibly even the one-stent technique, in true distal left main bifurcation lesions. The main procedural advantage of DK crush is that rewiring of the side branch ostium is only performed through one layer of struts, which substantially improves FKBI and procedural success rates (FKBI: 100% in the current study compared to 75.3% in non-left main lesions in the BBC ONE and Nordic I trials39).
Limitations
An important limitation of the current study was the lack of randomisation. However, the clinical relevance of this study is based on the finding that the stenting approach carries a predictive value, a key point that should be carefully considered before treating distal ULMCA bifurcation lesions. Another limitation of the current study was the interplay between the medical team and the patient’s expectation, which was driven by the surgeon’s skills28 and the patient’s economic status and cultural background40. The lack of EuroSCORE collection precluded assessment with the Global Risk Score (the combination of SYNTAX Score and additive EuroSCORE)41. The baseline characteristics of the one-stent group and the different two-stent techniques were unevenly distributed. However, the lower incidence of TLR in ULMCA bifurcation lesions of the DK crush subgroup was in line with our previous finding in a randomised trial of unselected bifurcation lesions11, indicating that DK crush surpasses the other complex stenting techniques or even the one-stent technique with respect to the reduction of repeat revascularisation. Lastly, previous studies have shown unsatisfactory FKBI to be a predictor of TLR11,37. However, this was not precisely defined in the current study.
Conclusions
With distal left main true bifurcations, the two-stent technique (excluding DK crush) is an independent predictor of long-term MACE. The DK crush technique is potentially associated with more favourable long-term clinical outcomes. Appropriately powered randomised controlled trials are required to compare DK crush with one-stent and other two-stent strategies.
Funding
This study was funded by the Jiangsu Provincial Outstanding Medical Program (JPOMP-20041230).
Conflict of interest statement
The authors have no conflicts of interest to declare.