“You never know what is enough unless you know what is more than enough”
William Blake (1757-1827)
Coronary bifurcations account for 15-20% of all percutaneous coronary interventions (PCI) and remain one of the most challenging lesions in interventional cardiology in terms of procedural success rate as well as long-term cardiac events1.
The first step in bifurcation treatment is to evaluate whether or not the side branch will cause clinical problems if it is lost during the procedure. A “significant” side branch is most often arbitrarily defined and based upon the subjective judgement of the operator. In practice, this implies that a significant side branch is a branch that the operator does not want to lose after evaluating the individual patient in a global context, i.e., patient symptoms, patient comorbidity, diameter and length of side branch, plaque burden and localisation in the bifurcation area, angle between main branch and side branch, size of the myocardial mass supplied by the side branch, location of ischaemia, viability of the supplied myocardium, collateralising vessel, left ventricular function, results of functional tests, and so forth1.
The risk of closure of a significant side branch in coronary bifurcation treatment is the main issue when planning the treatment strategy. The dilemma is clear: if it is known beforehand that there is a high risk of side branch closure, it is possible to choose a technique that protects the side branch up front (i.e., often a two-stent technique or a dedicated device). A more complex technique such as this may, however, have a higher risk of periprocedural biomarker leaks (myocardial infarction) and may also be burdened with a higher risk of long-term adverse effects (restenosis, stent thrombosis, myocardial infarction, etc.)2,3. On the other hand, if the risk of side branch closure is low, it is possible to choose the more simple strategy (provisional approach), with lower periprocedural risks and lower long-term event rates. However, this technique carries an innate risk of losing the side branch if, despite the pre-treatment risk evaluation, it closes during the procedure.
As a consequence, despite a fast-growing body of scientific literature in the field, the optimal management of bifurcation lesions is still the subject of considerable debate. Some of the concerns are: 1) in which lesions and when should a provisional one-stent strategy or a two-stent technique be used up front; 2) should a dedicated bifurcation stent device be used; and 3) what is the potential increased risk of long-term adverse effects (late lumen loss as well as late stent thrombosis) and is this associated with treatment complexity1?
To address these key questions, bifurcation technique studies with long-term follow-up are needed. In this issue of EuroIntervention, two papers with five-year follow-up of different approaches for bifurcation stenting are presented. The authors should be complimented for providing these important data.
Verheye and colleagues present five-year follow-up of a cohort of patients with drug-eluting side branch stenting following implantation of the dedicated Axxess™ stent (Biosensors International, Singapore) in coronary bifurcation lesions4. They found no difference in long-term clinical outcome between the two groups, “Axxess alone” and “Axxess with side branch stenting”. Whilst data are not randomised and although the use of the dedicated Axxess device needs careful patient selection before implantation, the long-term results support the idea of using dedicated devices when the coronary anatomy is suitable.
Ferenc and co-workers present the five-year follow-up of the randomised Bifurcations Bad Krozingen 1 (BBK 1) study comparing provisional T-stenting with routine T-stenting (a two-stent technique) and conclude that routine T-stenting offers no advantage over provisional T-stenting in terms of target lesion revascularisation or MACE5.
These randomised data are in line with the five-year follow-up of the combined patient-level meta-analysis of the BBC ONE trial (randomisation between provisional stenting versus a two-stent strategy) and the NORDIC I trial (randomisation between provisional stenting versus a two-stent strategy), promoting the provisional approach as the workhorse strategy in bifurcation stenting (oral presentation, TCT 2015).
In all four trials, however, first-generation DES with durable polymer were used (sirolimus in BBK 1 and NORDIC I, paclitaxel in BBC ONE and mostly sirolimus in the side branch stent in the Axxess registry)4,5. It has to be borne in mind that second-generation DES with biodegradable polymers and thinner stent struts might prove to have much better long-term outcomes, even after complex stenting techniques6. Furthermore, there is increasing evidence supporting the benefit of a two-stent strategy in bifurcations with side branches above 2.75 mm in diameter; it must be remembered that the vast majority of side branches in the four studies were close to 2.5 mm in diameter7. There was a low percentage of left main (LM) stenting in the four studies, and not much from the studies can be extrapolated to everyday practice where more and more PCI of the LM is being performed. Left main PCI calls for an effective, simple, swift and safe workhorse procedure, since most patients, and especially the fragile elderly patients who are declined for surgery, seldom tolerate long compromising of the LM flow due to complex techniques, ballooning and bulky devices.
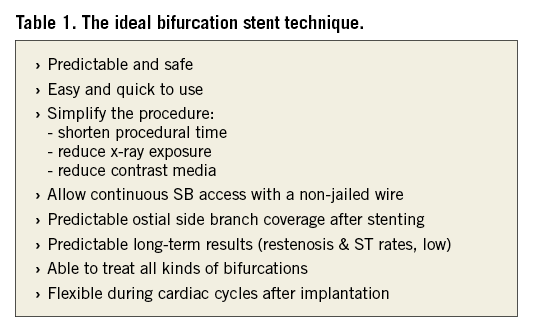
At the moment, there are a lot of different stenting strategies and different approaches to bifurcation stenting both within the provisional strategy and in all the different two-stent strategies1. The question is, what is the ideal technique or the ideal device for coronary bifurcation treatment (Table 1) and does one strategy or device fit all?
The way forward in trying to clarify this question calls for more long-term follow-up data in the already finalised studies to gain more knowledge of the long-term effects of the different techniques and devices. Furthermore, studies of stent techniques with the new-generation DES as well as with dedicated devices should be encouraged, to define their role in the treatment of bifurcations. Finally, the effect and place of biodegradable scaffolds in bifurcation treatment need to be defined8.
In conclusion, the long-term follow-up of bifurcation studies has pointed to the fact that the target is moving and that much more scientific work is needed, not only in non-LM bifurcation treatment but also in the treatment of the LM where dedicated devices may play a role in the future.
Conflict of interest statement
The authors have no conflicts of interest to declare.