Abstract
Aims: Percutaneous coronary intervention (PCI) is increasingly being used to treat left main stem (LMS) coronary artery disease. Disease at the LMS bifurcation is technically challenging to treat, and there is no consensus as to the best method. We previously described experimental and initial clinical results with the simultaneous kissing stents (SKS) technique in a small series using drug-eluting stents (DES). We now report our results in a larger cohort with long-term follow-up.
Methods and results: We treated 150 consecutive, unselected patients with unprotected bifurcation LMS with SKS using DES. The patients’ mean age was 67 years, 70% were male, 45% were non-elective and 35% were not surgical candidates. The New York Risk Score estimate of in-hospital mortality was (median) 0.7% (IQR 0.3-3.9%), logistic EuroSCORE 3.3% (1.3-11.9%) and angiographic SYNTAX score 20 (15-27). SKS were deployed in 99.3% of cases, and DES in 97%. There was no emergency CABG. The mortality rate at one year was 11.3% and at two years 12.7%. The (ischaemia-driven) target lesion revascularisation rate was 4.3% at one year and 6.2% at two years.
Conclusions: The SKS technique for treating ULMS bifurcation disease is simple, feasible, effective and durable in treating “all-comers” with LMS bifurcation disease. It is a two-stent technique worthy of consideration at the LMS bifurcation.
bbreviations
ACT: activated clotting time
ARC: Academic Research Consortium (definitions of stent thrombosis)
atm: atmospheres (pressure)
CABG: coronary artery bypass grafting
COPD: chronic obstructive pulmonary disease
Cr: creatinine (serum level in mg/dL)
Cx: circumflex coronary artery
CVA: cerebrovascular accident
DES: drug-eluting stents
IABP: intra-aortic balloon pump
IQR: interquartile range
LAD: left anterior descending coronary artery
LMS: left main stem
LV: left ventricle
MACCE: major adverse cardiac and cerebrovascular events
NSTE-ACS: non-ST-elevation acute coronary syndrome
PCI: percutaneous coronary intervention
PVD: peripheral vascular disease
SKS: simultaneous kissing stents
SYNTAX: SYNergy Between Percutaneous Coronary Intervention with TAXus and Cardiac Surgery study
TVR: target vessel revascularisation
Background
Until recently, coronary artery bypass grafting (CABG) was the “gold standard” for treating left main stem (LMS) disease. However, the SYNergy between Percutaneous Coronary Intervention with TAXus and Cardiac Surgery (SYNTAX) study, suggested equivalence in the rate of composite “hard” endpoints for percutaneous coronary intervention (PCI) using drug-eluting stents (DES) vs. CABG for selected patients with LMS disease, in a large subgroup analysis1. Being a subgroup analysis, this finding may be regarded as hypothesis-generating rather than definitive. A large, Korean, randomised study supported these findings, although the non-inferiority margin over CABG was wide2. There are also registries demonstrating the safety and efficacy of this approach in a wide variety of patients and clinical settings3, including in patients at high surgical risk4,5. The current ESC guidelines give PCI for ostial or body of LMS disease a Class IIa recommendation, and bifurcation LMS disease a Class IIb recommendation, even in surgical candidates6.
Approximately 70% of lesions affecting the LMS involve the bifurcation, and PCI of such lesions is associated with higher risk than for those of the body or ostium of the LMS7, although some operators have reported excellent results in the latter setting8. However, no single type of LMS bifurcation stenting technique has yet been proven superior to the others. Some two-stent techniques, e.g., the “crush” technique, have been associated with poorer outcomes than others, albeit in the non-LMS setting9. A single-stent technique “provisional T”, where a good result is achievable with a single stent, usually with “kissing” balloons, is probably the most widely used, and such evidence as there is, also substantially derived from non-LMS bifurcations, points to this having more favourable results than double-stent techniques10,11. However, selection bias, crossover to a double-stent technique, and subsequent retrospective analysis, may go some way to explain the apparently suboptimal results seen in two-stent techniques.
SKS has been described by several authors for treatment at the LMS bifurcation8,12. Nevertheless, this remains a controversial technique, partly because bench testing in rigid artificial vessels results in poor stent expansion and distortion13. We have previously presented the results of treating our first 30 patients, with 100% technical success, one in-hospital death (3.3%), an ischaemia-driven target lesion revascularisation rate (TVR) of 2/29 patients (6.9%) and re-endothelialisation and healing in a porcine model14.
We now present our clinical results at medium term follow-up in a consecutive cohort of our first 150 patients with unprotected, bifurcation LMS treated by PCI using the SKS technique with DES.
Methods
PATIENTS
This was a consecutive series of patients with a clear indication for revascularisation. Since 2000, the majority of patients with a LMS stenosis in our institution were treated with CABG. The authors however, offered PCI, with a policy of maximum feasible revascularisation. Our results were subject to, and justified by, regular hospital audit. DES were available to us from 2004, and this report covers the period from then onwards. The patients were “all-comers”, and therefore included a substantial proportion with myocardial infarction and cardiogenic shock and those unsuitable for CABG. Patients were classified as “elective” (defined as a planned procedure for stable symptoms), “urgent” (defined as requiring in-patient revascularisation, usually for NSTE-ACS) and “emergency” (defined as requiring immediate revascularisation, usually for STE-ACS and cardiogenic shock). A LMS lesion was defined as >50% diameter stenosis in both of two angiographic projections, or >70% in one, judged by eye. Involvement of the bifurcation by the plaque or planned stent procedure was required in all cases. We consistently used a single-stent approach for disease of the ostium and body of the LMS, and cases involving the bifurcation when the circumflex vessel was small, non-dominant or un-diseased. But whenever a two-stent strategy was thought to be necessary, a simultaneous kissing stent (SKS) technique was used as the default strategy. The indication for SKS may therefore be summarised as involvement of the LMS bifurcation (of any Medina type) in the presence of two large branches requiring stenting. We include the 30 patients from our first report, because their follow-up is now long-term.
PATIENT PREPARATION
Patients were pre-treated or pre-loaded with aspirin and clopidogrel. Testing for the platelet response to clopidogrel has been performed since 2008. An inadequate response triggers a doubling of clopidogrel dose or, since the availability of prasugrel, transfer to that agent. Treatment with dual antiplatelet therapy was recommended to be continued indefinitely. An 8 Fr guide catheter (typically Voda-shaped) was generally used via a femoral artery approach. Heparin was given to maintain an activated clotting time (ACT) >250 seconds. Abciximab was administered for patients with visible thrombus, ACS, diabetes or extensive stenting. TAXUS® stents (Boston Scientific, Natick, MA, USA) were the default implants until March 2009, PROMUS® stents (Boston Scientific) from then until May 2010, and PROMUS Element™ stents (Boston Scientific) thereafter. IVUS and/or pressure wire was used when angiographic assessment was inadequate. Control angiography was routinely performed for the first 30 patients, but thereafter only for recurrent symptoms.
THE SIMULTANEOUS KISSING STENT (SKS) TECHNIQUE
The SKS technique has been described previously15. A brief summary of the key practical points of the technique follows. 1) The lengths of the two stents were selected to cover not only the bifurcation, but also the body of LMS, to avoid distortion, dissection or residual stenosis of the ostium. 2) In rare patients with an exceptionally long LMS, this technique was avoided (no such cases were encountered here). 3) In cases involving disease of the proximal LAD or Cx, two long stents were selected to cover all the disease in the LMS and both branches, creating a single, sweeping curve into each vessel. 4) Sizing of each stent was 1:1 with respect to the reference segment of each branch, usually assessed distal to the disease, thereby “automatically” achieving an appropriate cross-sectional area both in the branches and in the LMS itself. 5) High-pressure balloon dilatation, with post-dilatation if necessary, was performed to ensure full stent deployment, particularly at points of constriction, such as the circumflex origin. Both balloons were inflated simultaneously to prevent one or other stent being crushed. 6) The best angiographic views for evaluation of lesion coverage and stent expansion were the left anterior oblique projection with caudal tilt for the bifurcation, and the left anterior oblique projection with cranial tilt for the ostium of the LMS.
CLINICAL ASSESSMENT AND FOLLOW-UP
Clinical details of the patients were obtained from hospital, catheter laboratory and operator records. We recorded the age, sex, clinical indication (urgency), presence of diabetes, logistic New York Risk Score16, logistic EuroSCORE17, angiographic SYNTAX score18, the Medina classification of the LMS bifurcation19 and the number of other vessels diseased and treated. The clinical indication was regarded as being synonymous with the urgency of the procedure (elective, urgent or emergency). All major adverse cardiac and cerebrovascular events (MACCE) were recorded, including death, new STE-ACS, cerebrovascular accident and emergency CABG, using standard definitions. Mortality and repeat intervention were determined at most recent follow-up, from hospital records and the UK Office of National Statistics. Stent thrombosis was determined according to the method of the Academic Research Consortium20.
PROCEDURAL DETAILS
Details of the procedures were collated from the catheter laboratory database, patient case notes and personal records of the senior interventional cardiologist (JG). These included the number of vessels diseased, the number of vessels treated, the size and type of stents used, the use of an intra-aortic balloon pump (IABP), the administration of a glycoprotein IIb/IIIa antagonist, and any other relevant features.
STATISTICS
Descriptive data were presented as mean (SEM) for normally distributed data and median (IQR) for skewed data. Calculation of logistic EuroSCOREs, New York scores and SYNTAX scores were performed online21-23. Raw mortality data were displayed using the Kaplan-Meier method. Comparison of observed and expected mortality was performed using funnel plots using the method of Spiegelhalter24,25.
Results
PATIENTS
SKS with DES was attempted in 150 consecutive patients with bifurcation LMS disease between March 2004 and June 2009. The mean age was 67 years, 55% were male, 17% were diabetic, 7% had renal impairment, 9% were in shock, and 14% were treated as an emergency, 31% urgently and 55% electively. Intra-aortic balloon counterpulsation was required in 19% of patients and 47% received a glycoprotein IIb/IIIa inhibitor. The median estimate of in-patient mortality, as calculated by logistic New York Risk Score, was 0.7% (IQR 0.3-3.9%) and, by logistic EuroSCORE, 3.3% (IQR 1.3-11.9%). The SYNTAX score was 20 (IQR 15-27). Twenty-three per cent of patients had a NY risk score >5%, 39% a EuroSCORE >6% and 13% a SYNTAX score >32. Thirty-five per cent were deemed unsuitable for CABG by either a cardiologist or a cardiothoracic surgeon. The Medina classification of the LMS bifurcation was 1,1,1 in 55%, 1,1,0 in 26% and “other” in 19% (Table 1).
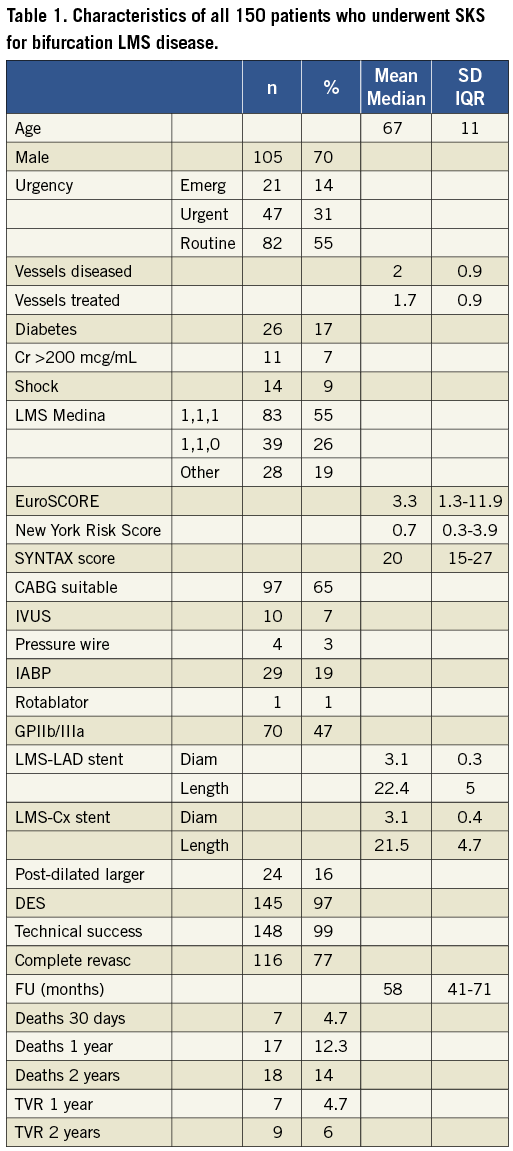
PROCEDURES
The SKS technique was technically successful in 148/150 (98.7%) patients (Table 1). 96.7% of patients received DES. The mean stent size at implantation was (nominally) 3.1×22 mm for the LMS-LAD stent and 3.1×22 mm for the LMS-Cx stent, although post-dilatation at high pressure with the deployment balloons was performed in all cases, and up-sizing with larger balloon(s) in 16%. In addition to the LMS, there was significant disease in a mean 2.0 other arteries, and PCI was performed in a mean 1.7 of these. Two examples of SKS deployment are depicted in Figure 1.
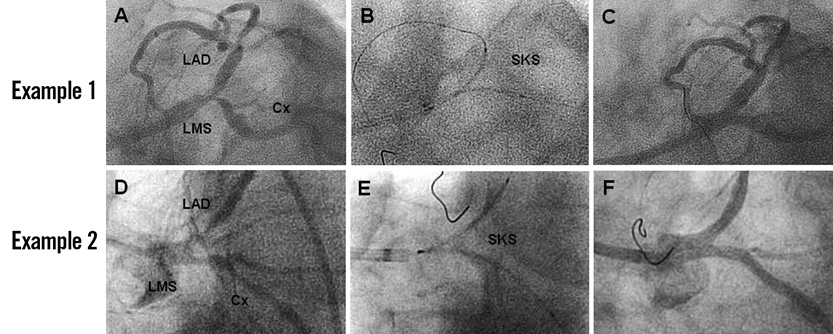
Figure 1. Two typical examples of the SKS technique for treating LMS bifurcation disease are shown. Example 1 (A-C). A 60-year-old man with diabetes presented with chronic stable angina and a LMS bifurcation lesion, Medina type 1,1,1 (A). Two 3.5×24 mm TAXUS™ stents were positioned (B) and simultaneously dilated to 16 atm pressure twice. The final result was excellent (C). Example 2. A 78-year-old man presented with an acute coronary syndrome, chest infection, aortic stenosis, impaired left ventricular function, a blocked RCA and a bifurcation LMS stenosis, Medina type 0,1,1 (D). After medical stabilisation, the approach was similar to Example 1. Two TAXUS™ stents were positioned (3×28 mm at LMS-LAD and 3×32 mm at LMS-Cx) (E) and simultaneously dilated to 16 atm pressure twice. The final result was excellent (F).
30-DAY OUTCOMES
The 30-day mortality of the entire cohort was 7/150 (4.7%). The characteristics of the seven patients who died are shown in Table 2. Six of the seven patients were treated as an emergency or urgently in the context of an ACS, two were in cardiogenic shock, the mean age was 71 years, 2.1 patients had other diseased vessels, none had renal failure, five were unsuitable for CABG, and two required IABP. The median scores for these patients were 27% (EuroSCORE), 17% (NYRS) and 24 (SYNTAX). Technical success was achieved in 6/7 cases. Complete revascularisation was achieved in 5/6 of the remaining patients, all of whom were stable at the time of leaving the catheter laboratory. The only elective patient who died was a 47-year-old man who developed an allergic reaction to clopidogrel. Overall, the 30-day mortality rates were 1/82 (1.2%) for elective, 3/47 (6.4%) for urgent, and 3/21 (14.3%) for emergency patients. Comparison of observed and predicted 30-day mortality is shown, using both NYRS and EuroSCORE, in Figure 2. The number of deaths was as expected according to the former and better than expected according to the latter. There was no emergency CABG. The 30-day MACCE rate of the entire cohort was 9/150 (6.0%).
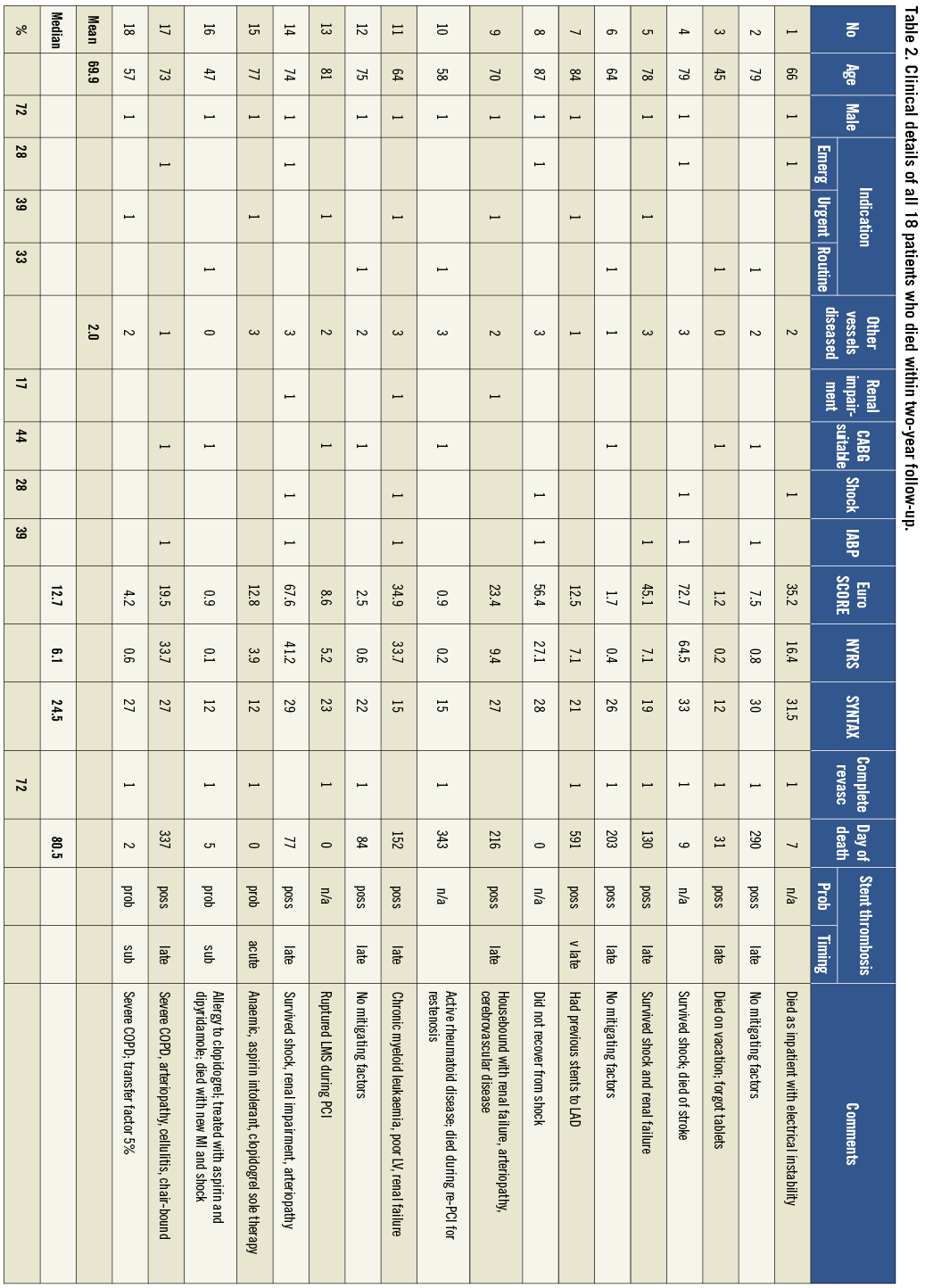
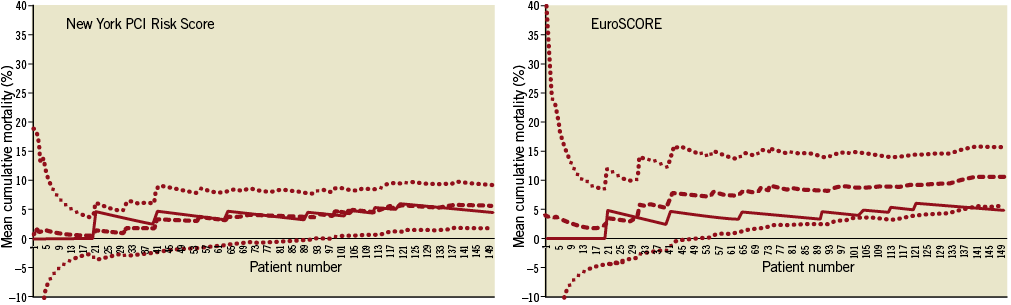
Figure 2. Funnel plots displaying the cumulative 30-day mean mortality rate compared with the mortality predicted by the NY risk score (upper panel) and EuroSCORE (lower panel). The x axis of each panel lists all 150 patients who underwent SKS in chronological order. The y axis is the cumulative mean risk of in-patient death. The continuous line is the observed cumulative mean mortality, each upward deflection representing a single death. The dashed line is the expected cumulative mean mortality. The dotted lines represent the 95% confidence intervals.
LATE OUTCOMES
Follow-up was to a median 58 (IQR 41-71) months, and no patient was lost to follow-up. The mortality rate was 17/138 (12.3%) at 12 months and 18/129 (14.0%) at 24 months. When analysed according to clinical presentation, the 24-month mortality rate was 6/82 (7.3%) for elective, 7/47 (14.9%) for urgent, and 5/21 (23.8%) for emergency patients (Table 2, Table 3 and Figure 3). Repeat revascularisation was required in 6/138 patients at 12 months (4.3%) and in 8/129 patients at 24 months (6.2%). Repeat PCI (SKB or SKS) was undertaken in 7/8 cases, and CABG in one. At two years, the sites of restenosis were LMS (3), LAD (3) and Cx (7). Repeat PCI was technically successful in all cases as it was possible to pass guidewires, balloons, IVUS catheters and, when necessary, stents through the original stents. Two examples of TVR are shown in Figure 4. The overall MACCE rate was 25/138 (18.1%) at 12 months and 28/129 (21.7%) at 24 months.
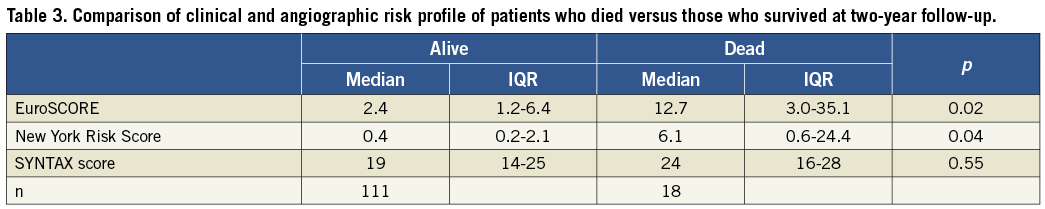
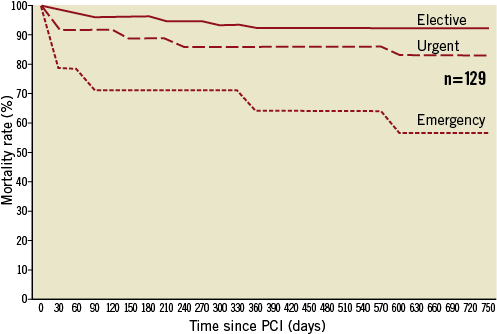
Figure 3. Kaplan-Meier plot of mortality after SKS, for 129 patients with complete two-year follow-up, subdivided according to clinical presentation: solid line (elective), dashed line (urgent), and dotted line (emergency). (See text for definitions)
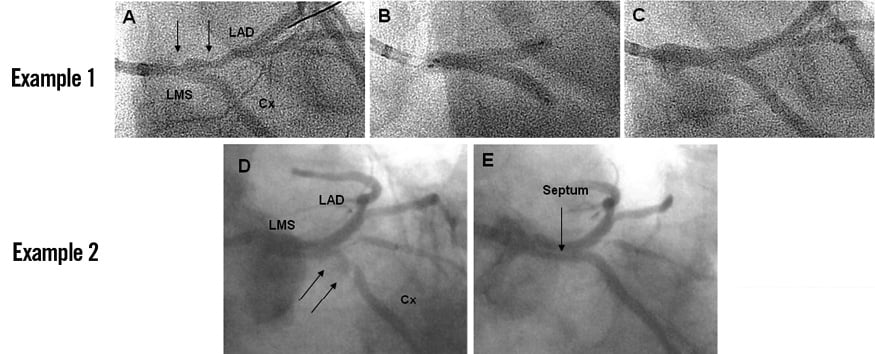
Figure 4. Restenosis in SKS - two examples. Example 1. Restenosis in the LMS-LAD stent (A-C). A 59-year-old man who had received SKS with two TAXUS™ stents (3.5×20 mm at LMS-LAD and 3.5×16 mm at LMS-Cx) eight months previously, presented with an STE-ACS. He was treated with fibrinolysis at another hospital with excellent effect and transferred to our centre. Angiography revealed restenosis affecting predominantly the LMS-LAD stent (arrows) (A). Both limbs of the SKS were pre-dilated with kissing 3.0 mm balloons. There was substantial recoil, so two new TAXUS™ 3.5×24 mm stents were implanted in SKS formation (B), with excellent results (C). Example 2. Restenosis in the LMS-Cx stent (D-E). A 55-year-old man had received SKS with two 2.75×24 mm TAXUS™ stents to treat a LMS stenosis six months previously. He experienced recurrent symptoms. Angiography revealed restenosis in the Cx limb of the LMS-Cx stent (arrows), both stents within the LMS appearing free of neointima. The portion of the LMS-Cx stent in the Cx was dilated with a 3.0 mm balloon at 20 atm pressure with an excellent final result. A layer of tissue covering the metal “septum” created by the two stents was also apparent (E).
STENT THROMBOSIS
Of the 18 deaths at two-year follow-up, according to the ARC definitions, five were not due to stent thrombosis (ST), these being acutely ill patients who died on the day of the procedure, or shortly afterwards, due to cardiac causes related to their clinical presentation (or the procedure, in one patient). The remaining 13 deaths were classified as follows: one probable acute ST, two probable subacute STs, nine possible late STs and one possible very late ST. Of the ten late and very late cases, only four were free of serious comorbidity, and all these deaths occurred before the introduction of clopidogrel testing (Table 2).
“SYNTAX-LIKE” PATIENTS
Application of SYNTAX study criteria (suitability for PCI or CABG, and for whom either modality would offer equivalent and full revascularisation) to our study population identified 80 patients (53% of our cohort). For this group, the mortality rate at 12 months was 6/73 (8.2%) and at 24 months 6/71 (8.5%). The corresponding TVR rates were 3/73 (4.1%) and 4/71 (5.6%), respectively. There were no other major adverse events, so the 12- and 24-month MACCE rates were 12.3% and 14.1%, respectively. In the SYNTAX trial, the 12-month MACCE rates were 17.8% (PCI) and 12.4% (CABG)1.
Discussion
This is the first description of the medium term results achieved in a substantial series of patients with unprotected LMS bifurcation disease treated with SKS. In this study, which involved a single centre, a single principal operator, a well characterised, inclusive, consecutive, group of patients, including those with ACS, cardiogenic shock, and surgical rejects, consistent technique and adjunctive medication were used, and follow-up was complete. The mortality rate was 4.7% at 30 days, and the majority of these deaths occurred in patients with ACS. The two-year mortality rate was 7.3% for elective, 14.9% for urgent and 23.8% for emergency patients. Repeat revascularisation was required in 4.7% of patients at 12 months and 6.2% at 24 months.
Comparison of our mortality outcomes with those from other similar registries and trials of LMS stenting reveals reasonable results, considering the casemix of our cohort, the overall mortality rate being 12.3% at one year and 14.7% at two years. For our SYNTAX-like patients, the one-year and two-year mortality rates were 8.2% and 8.5%, respectively, compared with one-year figures from the SYNTAX study itself of 4.4% for PCI and 4.2% for CABG. This difference may be explained by the more stringent nature of patient selection in a randomised study. Furthermore, symptom relief was excellent and durable, as evidenced by rates of symptom-driven TVR of 4.3% at one year and 6.2% at two years. By comparison, in a series with bifurcation LMS disease treated with sirolimus-eluting stents (with SKS in 68%), the TLR rate was 38%, although it was ischaemia-driven in 14%. In that study, restenosis was focal in 85% of cases, and involved the branch ostia in 82%, sparing the LMS itself26. One of the largest series of SKS in the LMS, prior to the present study, was that of the Seoul group, which employed sirolimus-eluting stents in 36 patients, with 100% success and, over two years of follow-up, no deaths, stent thromboses or MIs and a TLR rate of 14%8.
In our series, out of eight patients with symptomatic restenosis at two years, significant neointimal encroachment was seen in one or other “barrel” in the LMS in three cases, the LAD only in three and the Cx only in seven. The Cx is a common site of restenosis in other studies27. With SKS, this is unlikely to have been due to a systematic disparity in size between the LMS-LAD and LMS-Cx stents, because the average stent sizes were so similar in each limb of the bifurcation in our series (3.1 mm for the LMS-LAD and 3.1 mm for the LMS-Cx), but may be because the angulation of the Cx artery from the LMS tends to be greater than for the LAD, predisposing to poor stent expansion, wide cell opening, strut deformation and reduced shear stress. It was notable that repeat PCI, with SKB or SKS, was feasible, technically successful, and associated with sustained symptomatic benefit, in all cases undertaken. The single case referred for CABG could have been treated with repeat PCI, but CABG was recommended by another cardiologist.
Several potential criticisms of the SKS technique have been raised. The first is a perceived difficulty with repeat catheterisation. In fact, we did not experience any problems with repeat angiography or repeat PCI: the passage of wires, balloons, IVUS probes and stents to the LAD and Cx arteries was possible in all cases, although it sometimes required a few minutes to pass a wire to the second “barrel” of the SKS. The second is the risk of late stent thrombosis (ST) with an uncovered metal septum in the LMS. In our series, we meticulously evaluated all our deaths from the point of view of the possibility of ST. Although some deaths were of unknown cause in the community, it was notable that they included a preponderance of patients at high risk of such an event, with major predisposing factors such as renal impairment, arteriopathy and discontinuation of dual antiplatelet therapy. Although clopidogrel testing was introduced late in this series, no out-of-hospital deaths within two years follow-up have occurred since that time. In cases with a poor or borderline platelet response to clopidogrel, we now advocate the use of more potent oral agents such as prasugrel or ticagrelor. Continued dual antiplatelet therapy and smoking cessation are clear recommendations for this technique, although it is not known for how long a thienopyridine should be taken, and whether it is more important for this technique than for others involving the LMS.
This study has several limitations. First, it was conducted by a single operator, in a single centre. This did, however, bring the considerable advantage of consistency of technique, stent type, adjunctive therapy and follow-up. Second, there was no comparative group, such as one treated with CABG or one treated with another bifurcation stent technique. The former was not possible because of the large proportion of patients in this series who were not suitable for CABG; and the latter would have required dividing the group into two smaller cohorts. Third, the cohort size was modest (150) and follow-up was limited. Fourth, control angiography was only performed for recurrent symptoms, so subclinical, mild, angiographic restenosis was not documented. However, if restenosis had been severe, the lesion being in a major proximal site, it is highly likely that the patient would have developed significant symptoms. This was not the case in the vast majority.
A striking feature of this technique is its simplicity. It is straightforward to perform, and safe, provided the “tips and tricks” described above are followed. Remarkably, the technical success rate was close to 100%, despite the challenging clinical and technical casemix of this cohort. It is a double-stent technique which is quick to perform, in marked contrast to others, and provides rapid, reliable access to both main branches of the LMS. This is an attribute that is invaluable in the emergency situation. Furthermore, distal lesions may be treated easily, should this be required, even if it is necessary to stent the LMS first. No removal, or re-crossing, of guidewires is required at any stage, another safety advantage. SKS does, therefore, have major attractions, especially in unstable patients. It can be applied to a wide variety of morphologies and any Medina classification of bifurcation. It is particularly useful in cases of mismatch in size between the LMS and LAD. A single-stent approach in those circumstances can lead to undersizing of the stent in the LMS (or distortion of the architecture of the stent by oversized proximal optimisation) and the risk of dissection in the LAD. By sizing appropriately to each branch, SKS avoids these dangers and produces an ideal 1:1 relationship in total cross-sectional area of stented LMS and stented LAD/Cx. It also tends to avoid sharp angles with the side branch, instead giving rise to two smooth curves, one into each branch. This may have haemodynamic advantages.
Despite these considerable advantages, SKS has not been widely adopted. There are several possible reasons for this. One is that CT reconstructions tend to portray the stents as incompletely expanded or misshapen. This is inevitable if the model used for deployment is constructed from an incompressible material such as Perspex. Deployment in a latex model or in vivo is much more satisfactory, the stents tending to adopt an ovoid cross-section where they are in contact with each other. OCT reconstruction of coronary bifurcations is starting to reveal that ovoid sections at bifurcations is a common finding. The second relates to the metal carina. We recommend continuing both stents back to include the ostium of the LMS to avoid distortion of the proximal LMS and dissection, so the carina may typically be 6-12 mm long. However, our animal work demonstrated endothelialisation of the struts at that point, and control angiography has revealed tissue coverage in some patients, if viewed from the appropriate angle. The third concern is the duration of dual antiplatelet therapy. Our practice is to advise lifelong continuation, but we have no evidence that this is better than discontinuation, and it exposes patients to prolonged bleeding risk. Ultimately our results demonstrate that these concerns are matched by good results, given the clinical presentation, with meticulous technique and adjunct therapy.
Conclusion
The SKS technique, using DES, supported by long-term dual antiplatelet therapy and clopidogrel testing, gives good results in a typical, consecutive population of patients with bifurcation LMS disease. The mortality rate is commensurate with the acuity of presentation and the casemix of the population treated. The symptom-driven TVR rate is single-digit at one year, with very few cases presenting after that, indicating sustained benefit. Repeat PCI, if required, is feasible, safe and effective. Very long-term follow-up of these patients continues. The SKS technique has the potential to be more widely used at the LMS bifurcation.
Conflict of interest statement
All authors have accepted sponsorship to attend educational meetings from Boston Scientific. C.J. Malkin has benefited from an interventional fellowship sponsored by Boston Scientific.

