Abstract
This article introduces the new terminology proposed by the European Bifurcation Club in order to simplify the identification, description, localisation and measurement of coronary bifurcation lesions as well as the selection of appropriate treatment strategies. A bifurcation lesion is a coronary artery narrowing occurring adjacent to, and/or involving, the origin of a significant side branch that you do not want to lose. The very simple Medina classification is intended for exchange and clinical research purposes. It is combined with a clear side branch definition and is associated with multiple measurement and imaging modalities, which take into account the complexity of lesions and treatments. Dedicated angiography as well as 3D angiography and multislice computed tomography are absolutely necessary for measurement of the bifurcation angles. The MADS (Main, Across, Distal, Side) classification is based on the final position of the stents in the bifurcation and on the order in which stents are implanted according to a strategy reflecting lesion and technique complexity. Although this classification still seems exhaustive, it does not involve the numerous guide and balloon manoeuvres, which would require a thorough a posteriori electronic classification of all inherent specific technical details.
Introduction
The past 35 years have witnessed the ever-increasing use of coronary angioplasty, the revolutionary advent of bare metal stents followed by drug-eluting stents and, more recently, bioresorbable scaffolds. In this context, the treatment of coronary bifurcations remains a complex and controversial issue. Nevertheless, several definitions and classifications of lesions and treatments have been established and widely adopted. The purpose of this article is to assess the relevance of these tools in relation to the numerous technical strategies implemented in the treatment of bifurcation lesions.
Definition of coronary bifurcation disease
All currently available definitions1,2 are based on the involvement of a side branch (SB) in the main branch (MB) lesion, and generally take into account the diameter of the side branch. Definitions do not include the distance between the MB lesion and the SB, but rather the absence of a normal area between the MB minimal luminal diameter (MLD) and the SB. In most cases, the diameter of the SB used to define a bifurcation lesion corresponds to a diameter large enough to accommodate a stent (1.1/1 ratio between the stent and the arterial diameter for a 2.25 mm stent, i.e., a 2 mm SB).
A bifurcation lesion can also be defined according to the potential clinical consequences associated with the loss of the SB. The risk associated with a lost SB does not depend solely on its diameter3 in linear relation to the myocardial mass supplied, but probably to a greater extent on the elevation of biomarkers and late enhancement volume assessed by magnetic resonance imaging (MRI). These two parameters cannot be easily anticipated as they are related not only to the myocardial mass at risk, but also to the collateral supply to the SB or its collateralising role. Attempts have been made to anticipate the risk of myocardial infarction on the basis of an endocoronary ECG of the SB occluded by an MB balloon4.
The definition of coronary bifurcation lesions adopted by the EBC is pragmatic: a bifurcation lesion is ‘‘a coronary artery narrowing occurring adjacent to, and/or involving, the origin of a significant side branch’’2. A significant SB is a branch that one does not want to lose in the global context of a particular patient (symptoms, location of ischaemia, branch responsible for symptoms or ischaemia, viability, collateralising vessel, left ventricular function, etc.).
Classification of coronary bifurcation lesions
The objective is to associate each type of bifurcation with a prognosis, a technical difficulty or an optimal type of treatment, although this should not be regarded as systematically relevant. Many classifications have already been established in the field of interventional cardiology. It was therefore legitimate to classify the various types of significant lesion in the three segments of a bifurcation. Several classifications have been proposed, all of which require substantial memorisation efforts5-8. The significant advantage of the classification established by Medina lies in its simplicity9 (Figure 1). Each segment is assigned a value 0 in the absence of significant stenosis and 1 in the presence of a stenosis >50%. A value of 0 or 1 is therefore assigned to each of the three segments separated in the following order: proximal segment (PM), main distal segment (DM), side branch (SB), the values being separated by commas (Figure 2).
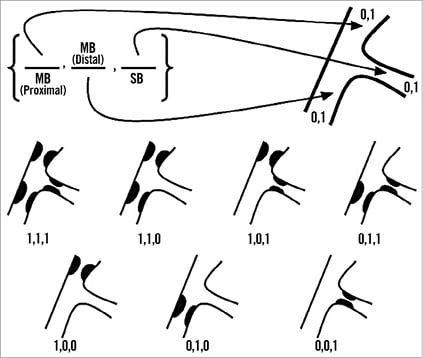
Figure 1. Medina’s classification.
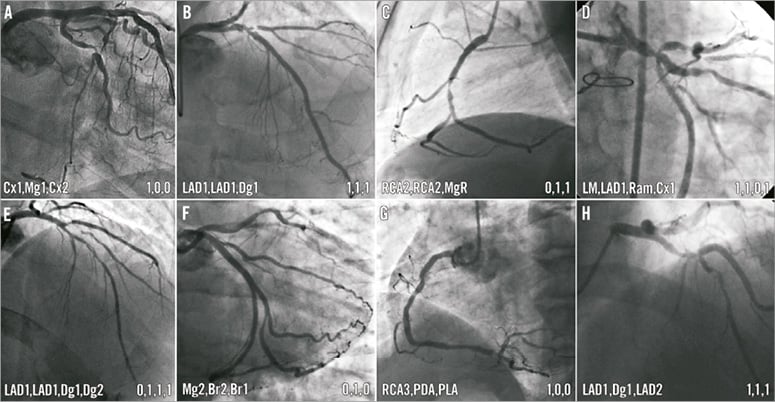
Figure 2. Eight examples of Medina’s inspired denominations of a bifurcation lesion (LAD 1=proximal LAD, proximal to first septal branch). Coronary segments corresponding to bifurcation (trifurcation) are presented as in the Medina classification, PM, DM and SB separated by commas. Usual abbreviations (or segment numbers) and coronary segmentation are used. The choice of the order of segments is left to the operator, before the procedure, based on their importance (diameter, distal length, flow, myocardial mass, viability, etc.) but not on technical aspects.
The EBC suggested that the Medina classification should be accompanied by a clear pre-treatment definition of the SB and the distal MB. Indeed, it seems natural that the longest and largest distal branch should be designated as the main distal branch, given the linear relationship between diameter, length, flow and supplied myocardial mass. The definition of the three bifurcation segments should be established in the same manner as the Medina classification (with the two commas).
The Medina classification was unanimously acclaimed and adopted during the first meeting of the European Bifurcation Club in September 2005 in Bordeaux1. Although it has supplanted the previous classifications, it is still the subject of harsh criticism, especially in the USA2,10-14.
Movahed maintains that a bifurcation lesion classification should be simple in order to be adopted and should include three major parameters.
– Is the diameter of the proximal healthy segment at least 2/3 of the sum of the diameters of both branches (otherwise the simultaneous kissing stent or SKS technique cannot be applied)?
– Are both ostia of a bifurcation involved or only the main or side branch? (When both ostia are involved the implementation of a complex strategy is inevitable).
– What is the angle between the branches (shallow or steep angle)?
The classification proposed by Movahed is impossible to memorise (Figure 3). It does not take into account the fact that the post-treatment diameter of the bifurcation proximal segment is equal to 2/3 of the sum of the distal diameters, according to Murray’s law, modified by Huo and Kassab and simplified by Finet15-18. This classification is treatment-oriented, arbitrary and is not supported by any reliable clinical trial. The SKS technique has never been evaluated in any randomised trial or multicentre registry. The contraindication to the crush and culotte strategies in instances where the angle between the two distal branches (EBC: angle B for “between”) is greater than 70° is based on two studies which are now relatively outdated19,20. Since then, it has been shown that technical failure in this setting is not exclusively related to the angle21,22. In addition, the involvement of the ostia of the distal branches is difficult to define, given that a lesion in the SB ostium may be located in the wall of the MB23 and the degree of stenosis is overestimated both by visual assessment and by quantitative angiography not dedicated to bifurcations24,25.
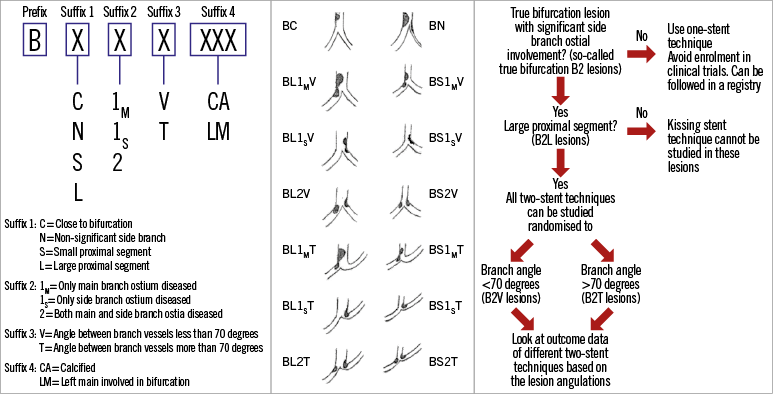
Figure 3. Movahed coronary bifurcation lesion classification (modified from Movahed references). Left panel: method to build a bifurcation class. Middle panel: simplified classification as the suffix 4 is not used. Right panel: Movahed recommendations for treatment and study design.
Regarding the only published patient-level meta-analysis combining data from the Nordic I and BBC One trials26, Movahed suggested that the difference in the incidence of the combined endpoint (all-cause mortality, myocardial infarction and target vessel revascularisation) in favour of the provisional strategy was related to the greater lesion severity in the complex group (larger SB with longer and tighter lesions). Both study groups were adjusted by means of a propensity score, which resulted in the hazard ratio being higher in the simple strategy group than before adjustment. This study confirmed the superiority of the simple strategy in all subgroups (true bifurcation lesions, large SB, tight and long SB lesions, equivalent diameters of two branches, etc.). In September 2014, data were reported showing that overall mortality at five years was higher in the complex group (Behan, oral communication at the EBC 2014). The only available randomised study in favour of the complex strategy27 was weakened by the definition of a combined endpoint at 12 months after systematic coronary angiography at eight months.
Medina wrote that the main purpose of a bifurcation classification is that it “allows for homogenous terminology when comparing different series and techniques”9. A further issue relates to whether a bifurcation classification can predict outcomes or determine the interventional approach, in which case the classification could be modified28,29. The complexity of treating bifurcations arises mainly from the fact that bifurcations vary not only in anatomy (plaque burden, location of plaque, angle between branches, diameter of branches, bifurcation site) but also in the dynamic changes that occur during the procedure, such as plaque shift and dissection30.
Medina’s classification can be carried out by visual angiographic analysis. However, the fact that 2D angiographic analysis is not adequate for SB assessment should prompt the use of dedicated quantitative coronary angiography (QCA) software providing the three reference diameters, as well as lesion length, percentage and bifurcation angles31. Medina’s classification can also be performed on the basis of data from IVUS, optical coherence tomography (OCT) or multislice computed tomography (MSCT)32-34. A Medina “fractional flow reserve (FFR) index” has also been considered, though this is not feasible as FFR can only be used to analyse two vessels and not three segments.
Classification of bifurcation treatment techniques
The advantage of a classification of techniques is that they can be described in a simple manner and that their respective benefits and drawbacks can be listed and compared. This type of classification should be simple but also exhaustive and/or open. Few treatment classifications have been reported or published. The classification by Lefèvre included four techniques34, Movahed’s classification6 only a few more, and Louvard’s5 was more complex but non-exhaustive when it was first published.
In order to be easy to memorise and exhaustive, the classification proposed by the EBC2 was based on two principles: the final position of the stent(s) (1 to 3 stents) in the bifurcation and the implantation order. The position of the first stent in a bifurcation corresponds to a given strategy. There are four strategies designated as MADS (named by R. Kornowski) (Figure 4): M strategy begins by a stent in the proximal Main segment. Strategy A begins with a stent in the main vessel Across the SB. Strategy D defines a Double stent implantation whether simultaneous or not and in an aborted form a stent and a balloon at the ostium of the two distal branches, with a slight protrusion (V stenting) or a long new carina35. S strategy consists of a stent implantation in the SB first with protrusion (short or long) or not. After implantation of the first stent(s), further stents can be implanted using different techniques. No wire or balloon manoeuvres are described in MADS, such as SB protection by wire or balloon, or different ways to crush an SB stent (kissing, balloon crush, double kissing crush, etc.). In addition to the “straight” strategies, the inverted strategies whereby the smallest distal branch is considered the main distal are also described (hence there are straight and inverted culotte techniques).
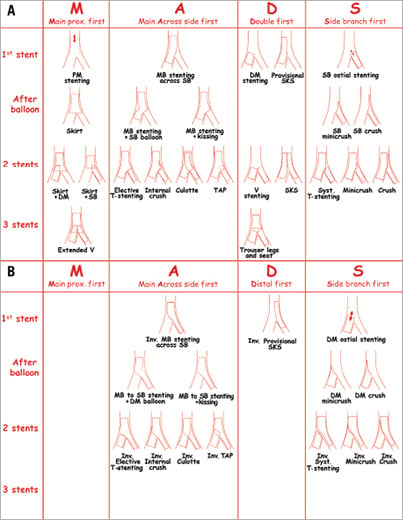
Figure 4. MADS classifications for straight (A) and inverted (B) strategies.
All the techniques described in the MADS classification have been reported or published. Many complex techniques have not been thoroughly described, even though every detail may have an impact on the outcome36,37. An electronic CRF based on MADS would probably allow a more accurate classification in the context of a core lab analysis.
MADS provides a description of the various techniques according to the logical course of the procedure. The final classification based on stent positioning has never been proven inadequate, whatever the technical strategy implemented. Certain measurements such as the length of protruding segments or stent overlap can be obtained through core lab QCA. At least one study comparing two MADS strategies has been carried out38.
Conclusion
The EBC definition of coronary bifurcation lesions, the Medina designation and classification of lesions and the MADS treatment classification are now part of the glossary used by the specialists of coronary bifurcation stenting. The simple and even basic nature of these classifications warrants the combined used of dedicated measurement methods for randomised studies. In the future, analysis of the data provided by the classification of lesions should make it possible to associate each type of lesion with a specific prognosis and optimal treatment strategy.
Acknowledgements
The authors thank Catherine Dupic for assistance in manuscript preparation.
Conflict of interest statement
Y. Louvard has received fees from Terumo and Medtronic for workshops. A. Medina has no conflicts of interest to declare.

