Abstract
Aims: The present study sought to compare angiographic and clinical outcomes of a simple strategy versus a complex strategy in patients with coronary bifurcation lesions undergoing drug-eluting stent implantation.
Methods and results: Medline, the Cochrane Library, and other internet sources were searched for randomised trials comparing simple strategy versus complex strategy for treating patients with bifurcation lesions. Nine eligible randomised trials including 2,569 patients were identified. The meta-analysis showed that cardiac death (odds ratio [OR]: 0.99, 95% confidence interval [CI]: 0.40-2.41, p=0.98) and stent thrombosis (OR: 0.64, 95% CI: 0.31-1.34, p=0.24) were similar in the simple and the complex strategy. Compared with the complex strategy, the simple strategy was associated with a reduced risk of either early or follow-up myocardial infarction (OR: 0.53, 95% CI: 0.36-0.79, p=0.002; OR: 0.60, 95% CI: 0.43-0.86, p=0.01, respectively). The overall risks of side branch restenosis (OR: 1.44, 95% CI: 0.73-2.87, p=0.30), target lesion (OR: 1.72, 95% CI: 0.95-3.12, p=0.07) and target vessel revascularisation (OR: 1.59, 95% CI: 0.94-2.69, p=0.09) were comparable between the two groups. In the true bifurcation, with large side branches, and DK-crush subgroups, there were higher rates of reintervention seen in the simple strategy than in the complex strategy.
Conclusions: A complex strategy remains an optional treatment for patients with coronary bifurcation lesions without severe safety concerns. A complex strategy may be an optimal treatment for true bifurcation lesions with large side branches.
Introduction
Coronary bifurcation lesions can be technically challenging, and the simple strategy is the preferred treatment compared with the complex strategy1. In the past decade, randomised trials2-7 and meta-analyses8-11 have indicated “simple is better” for treating coronary bifurcation lesions, mostly due to a high incidence of myocardial infarction (MI) following the complex strategy. Indeed, the simple strategy not only reduces procedure-related complications, but also decreases device-related clinical events at follow-up. However, two recent randomised trials demonstrated that the complex strategy using a novel DK-crush technique was associated with a lesser need of revascularisation in the treatment of patients with true bifurcation lesions, compared with the provisional stenting technique12,13. The favourable clinical outcomes following the complex strategy in these two studies were attributed to the fact that the novel DK-crush technique was used and true bifurcation lesions with relatively large side branches were selected2-4,6,7. Furthermore, recent advances in stent technology and invasive imaging, and percutaneous coronary intervention in the treatment of patients with coronary artery disease have minimised the risk of complications, especially stent thrombosis14,15. In addition, a recent multicentre registry showed that the DK-crush technique was an independent predictor of low incidence of major adverse cardiac events (MACE) in patients with unprotected left main coronary artery disease (ULMCA)16. Therefore, we performed this updated meta-analysis which represents the largest analysis comparing clinical and angiographic outcomes between the simple and the complex strategy for treating patients with coronary bifurcation lesions.
Methods
LITERATURE SEARCH
Literature comparing the simple and the complex strategy for coronary bifurcation lesions were acquired through searching Medline, Scopus, and the Cochrane Controlled Trials Registry from January 2002 to May 2013. In order to search and include all relevant studies, we used combinations of various keywords, including bifurcation, coronary bifurcation, simple strategy, complex strategy, 1-stent technique, 2-stent technique, drug-eluting stent, randomised, and clinical trial. References from reviews and selected articles were further screened.
INCLUSION AND EXCLUSION CRITERIA
The inclusion criteria were: (1) English-language study; (2) randomised comparison between the simple and the complex strategy; (3) bifurcation lesions treated by drug-eluting stents (DES); (4) at least six months of clinical follow-up. The exclusion criteria were: (1) studies with bare metal stent implantation; (2) non-randomised or non-English-language studies; (3) studies with duplicate publication, or different follow-up periods from the same sample origin.
DATA EXTRACTION AND QUALITY ASSESSMENT
All relevant articles were independently reviewed by two investigators (GXF and ZYJ) to assess the eligibility of each article and abstract with standardised data-abstraction forms, and disagreement was resolved by a third investigator (TNL). The following data were extracted from the eligible RCTs: study name, first author, publication date, baseline demographics, procedural characteristics, clinical outcomes, and angiographic results at follow-up. The methodological qualities of the included randomised trials were assessed by the Jadad score17.
STUDY ENDPOINTS
The clinical endpoints included: cardiac death, myocardial infarction (MI), target lesion revascularisation (TLR), target vessel revascularisation (TVR) and definite stent thrombosis, as defined in each study. The angiographic results at follow-up included main vessel and side branch binary restenosis, defined as ≥50% diameter stenosis.
STATISTICAL ANALYSIS
Dichotomous variables are expressed as odds ratios (OR) and 95% confidence intervals (CI). The heterogeneity among trials was evaluated with Cochran’s Q test and I2 statistic, and high heterogeneity was considered present for p<0.10 of the Q test and/or I2 ≥50%. The random-effects model was used if there was significant heterogeneity across trials. If not, the fixed-effects model with the Mantel-Haenszel method was performed. Egger’s linear regression test was employed to test for funnel plot asymmetry at the p<0.10 level of significance. A sensitivity analysis was performed by omitting a single study from the analysis one study at a time. The p-value threshold for significance was 0.05. Statistical analyses were conducted using STATA software 12.0 (StataCorp, College Station, TX, USA).
Results
ELIGIBLE STUDIES AND PATIENT CHARACTERISTICS
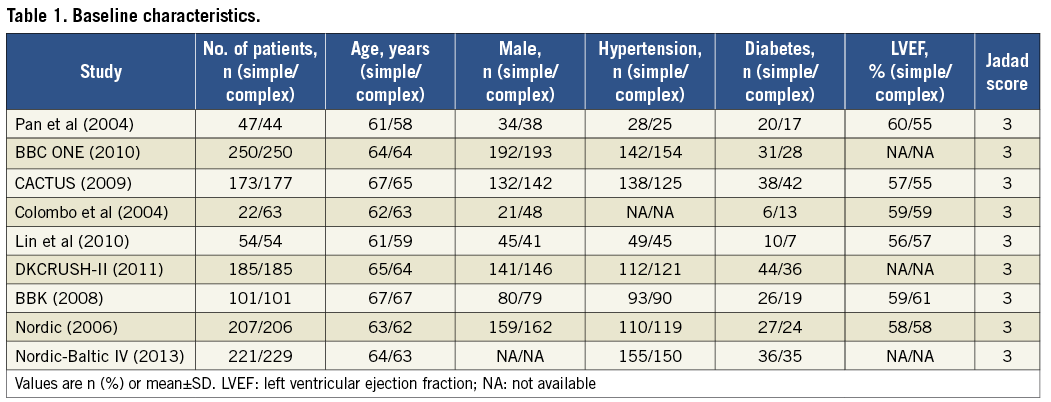
Nine eligible studies2-7,12,13,18, including a total of 2,569 patients, were identified in the present meta-analysis, with 1,260 patients in the simple strategy group and 1,309 in the complex strategy group (Figure 1). The quality of each study was high according to the Jadad score.
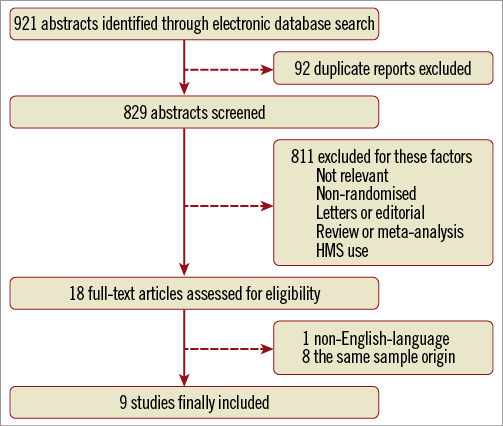
Figure 1. Flow chart of meta-analysis. BMS: bare metal stent
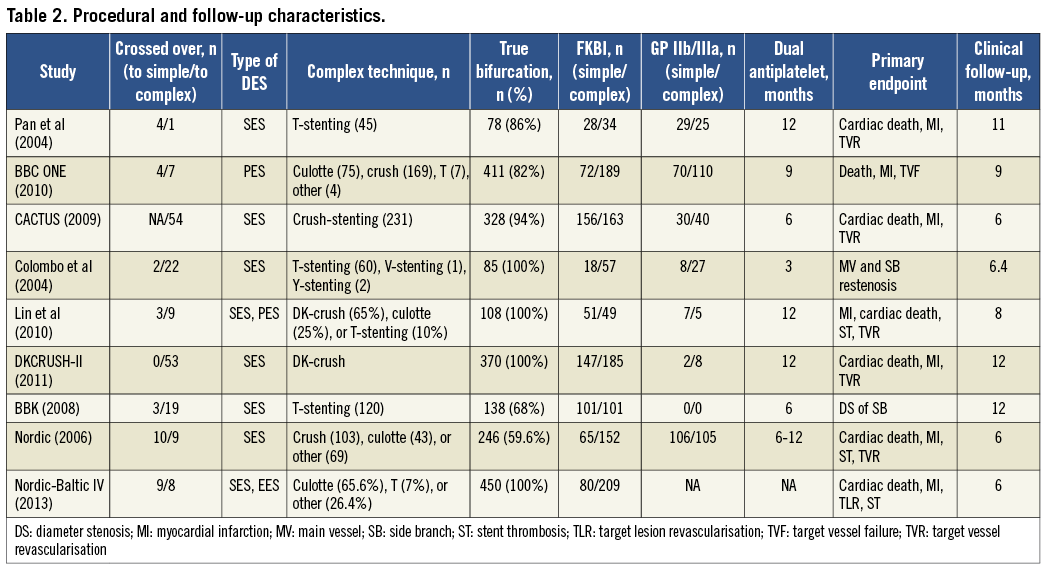
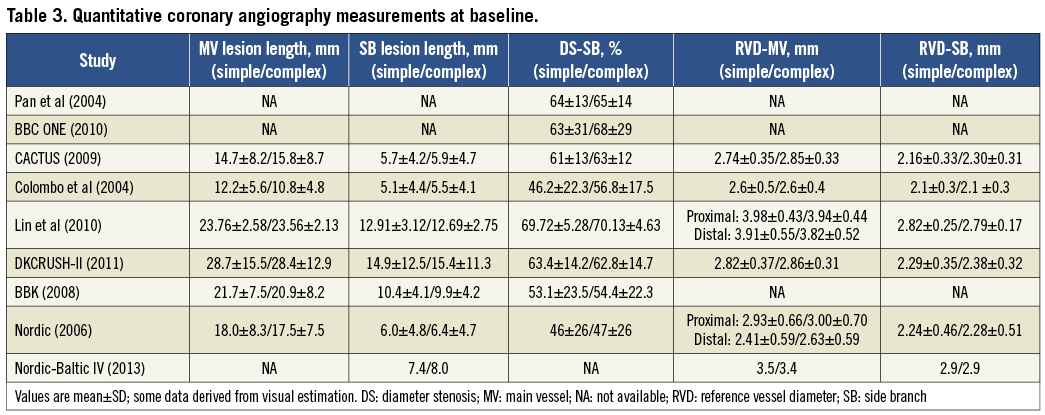
The baseline, procedural and follow-up characteristics, and quantitative coronary angiography measurements are listed in Table 1-Table 3. Three sub-analyses were performed according to the inclusion criteria in each study: large side branch and non-large side branch subgroups (stratified by whether the study enrolled the patients with side branch diameter ≥2.5 mm); true bifurcation and non-true bifurcation subgroups (stratified by whether the study only enrolled true bifurcation lesions); DK and non-DK subgroups (stratified by whether the DK-crush technique was used). The durations of dual antiplatelet therapy after index procedure varied from three to 12 months, and clinical follow-up periods ranged from six to 12 months.
CARDIAC DEATH AND STENT THROMBOSIS
As shown in Figure 2A, the complex strategy has a similar risk of cardiac death compared with the simple strategy for treating patients with coronary bifurcation lesions (OR: 0.99, 95% CI: 0.40-2.41, p=0.98), without significant heterogeneity among studies (p=0.95, I2=0%). No publication bias was found for cardiac death (Egger’s test: p=0.95).
There was no significant difference in the risk of stent thrombosis between the simple and the complex strategy (OR: 0.64, 95% CI: 0.31-1.34, p=0.24; Figure 2B), and no significant heterogeneity or publication bias was found (I2=0%, p=0.73; Egger’s test: p=0.25).
EARLY AND FOLLOW-UP MI
The simple strategy was associated with a significantly low incidence of early (in-hospital or one-month) MI (OR: 0.53, 95% CI: 0.36-0.79, p=0.002; Figure 2C), as well as follow-up MI (OR: 0.60, 95% CI: 0.43-0.86, p=0.005; Figure 2D). No evidence of statistical heterogeneity or publication bias was noted. The omission of a single study from the overall analysis had no significant impact on the pooled results of early MI. Sensitivity analyses suggested that the favourable results of the simple strategy were concealed in follow-up MI when the BBC ONE trial was omitted (OR: 0.76, 95% CI: 0.50-1.13, p=0.17).
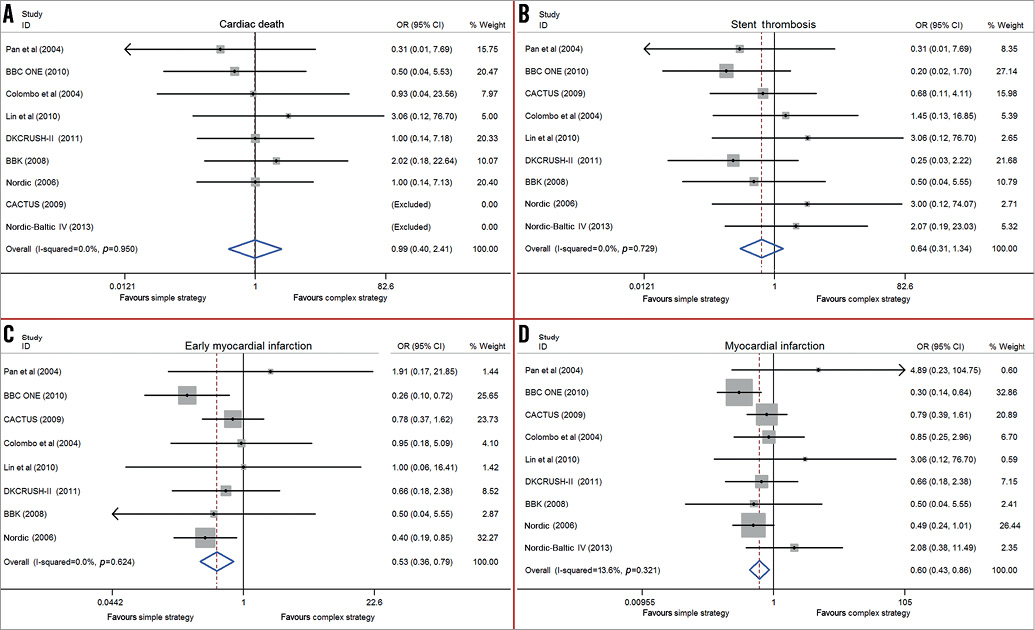
Figure 2. Forest plots from the included trials. Odds ratios of cardiac death (A), stent thrombosis (B), early myocardial infarction (C), and myocardial infarction (D), associated with simple strategy versus complex strategy for bifurcation lesions.
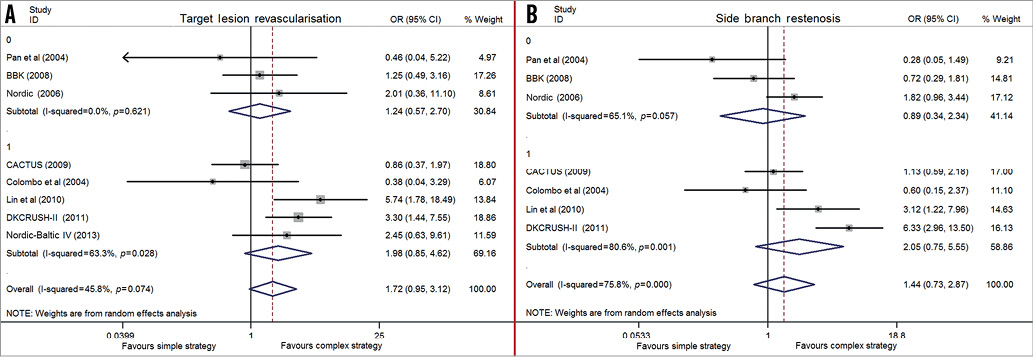
TLR AND TVR
The rate of TLR between the two strategies was similar (OR: 1.72, 95% CI: 0.95-3.12, p=0.07; Figure 3A), but with significant heterogeneity (I2=45.8%, p=0.07), as well as in TVR (OR: 1.59, 95% CI: 0.94-2.69, p=0.09; I2=48%, p=0.07, Figure 3B). No publication bias of TLR and TVR was found (Egger’s test: p=0.58 and p=0.56, respectively).
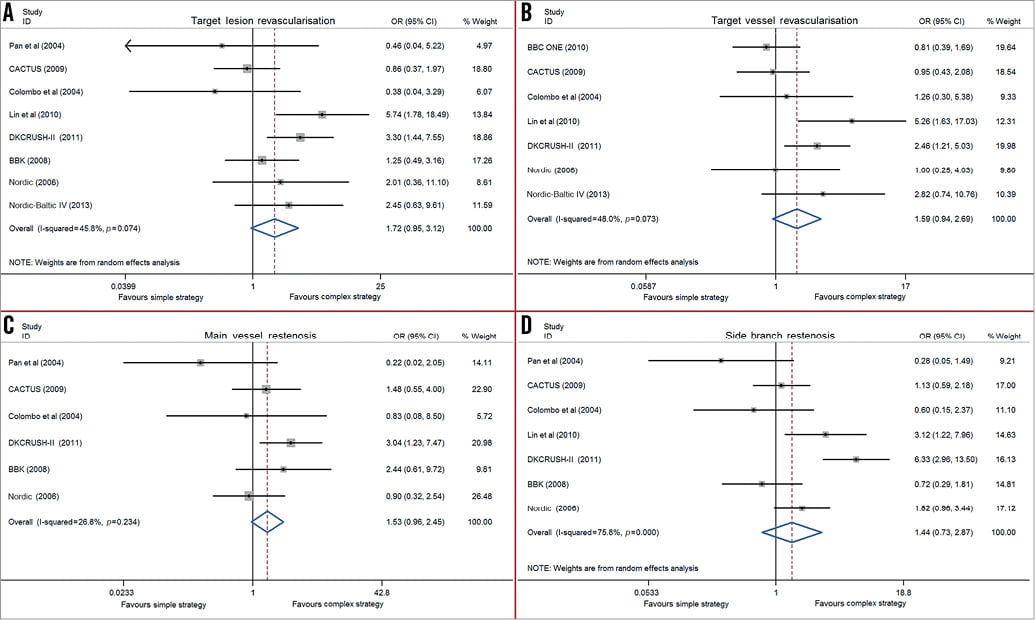
Figure 3. Forest plots from the included trials. Odds ratios of target lesion revascularisation (A), target vessel revascularisation (B), main vessel restenosis (C), and side branch restenosis (D), associated with simple strategy versus complex strategy for bifurcation lesions.
MAIN VESSEL AND SIDE BRANCH RESTENOSES
The main vessel restenosis rate was reported in six studies. There was a trend towards low main vessel restenosis in the complex strategy but this difference was not statistically significant compared with the simple strategy (OR: 1.53, 95% CI: 0.96-2.45, p=0.08; Figure 3C). No heterogeneity (I2=26.8%, p=0.23) or publication bias (Egger’s test: p=0.19) was found. The simple strategy had a similar side branch restenosis rate compared to the complex strategy (OR: 1.44, 95% CI: 0.73-2.87, p=0.30; Figure 3D), with a significant heterogeneity (I2=75.8%, p<0.001). There was no publication bias among studies (Egger’s test: p=0.31).
SUBGROUP ANALYSIS
In the large side branch subgroup analysis, there were no significant differences in TLR and side branch restenosis rate (Online Figure 1) between the simple and the complex strategy. However, the simple strategy was associated with a high risk of TVR (OR: 2.27, 95% CI: 1.27-4.05, p=0.01; Figure 4A) and main vessel restenosis (OR: 2.56, 95% CI: 1.14-5.78, p=0.02; Figure 4B) compared with the complex strategy. In the true bifurcation subgroup analysis, the simple strategy was also related to a high incidence of TVR and main vessel restenosis (OR: 2.04, 95% CI: 1.11-3.75, p=0.02 for TVR; OR: 2.06, 95% CI: 1.10-3.86, p=0.02 for main vessel restenosis; Figure 4C and Figure 4D) while similar TLR and side branch restenosis rates were observed in these two strategies (Online Figure 2A, Online Figure 2B). In the DK subgroup analysis, the complex strategy was associated with favourable clinical outcomes compared with the simple strategy: these significant differences in TLR, TVR, main vessel and side branch restenosis are visualised in Figure 4E-Figure 4H.
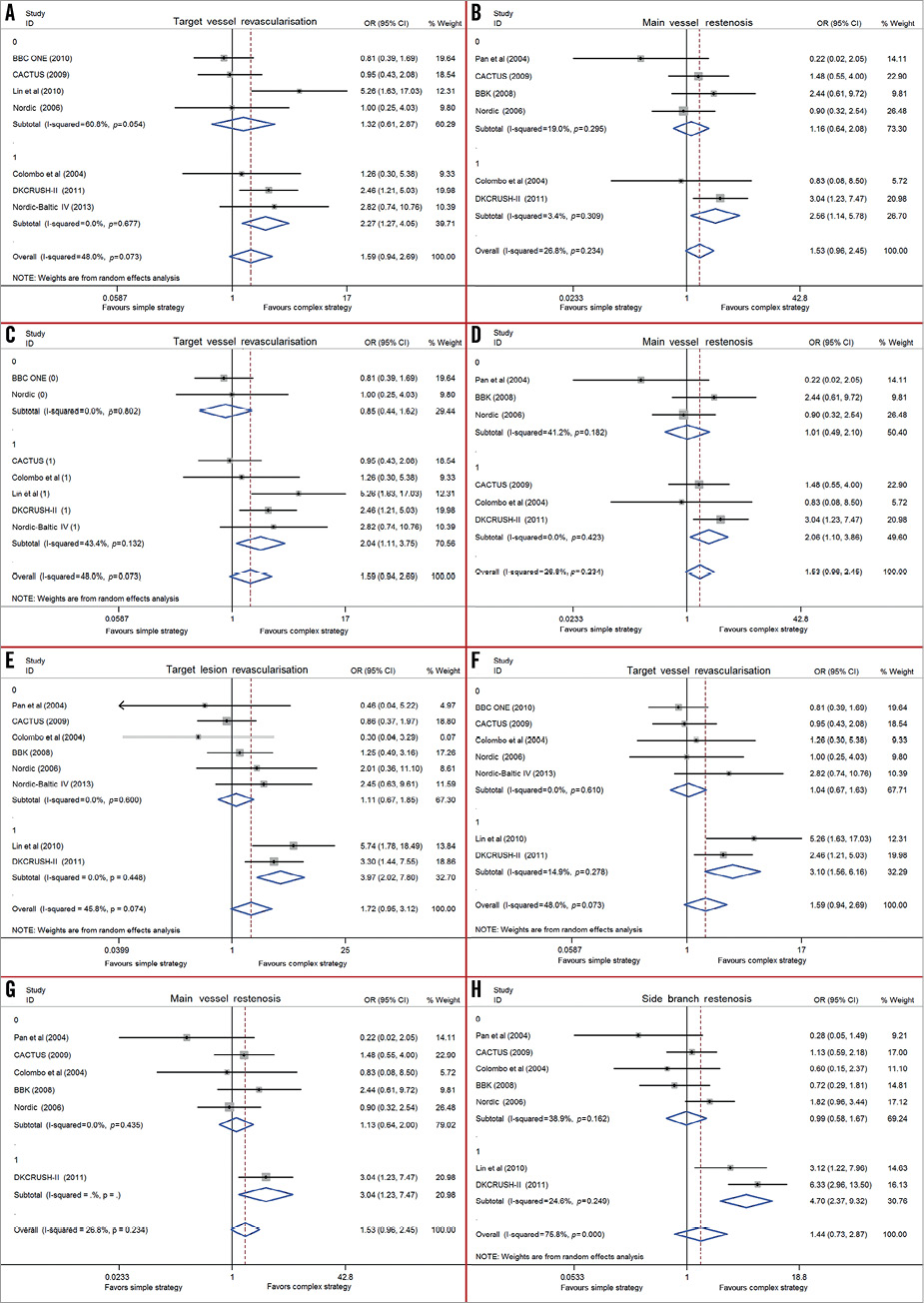
Figure 4. Forest plots from the included trials. Odds ratios of target vessel revascularisation (A), and main vessel restenosis (B) in the large side branch subgroup; target vessel revascularisation (C), and main vessel restenosis (D) in the true bifurcation subgroup; target lesion revascularisation (E), target vessel revascularisation (F), main vessel restenosis (G), and side branch restenosis (H) in the DK subgroup, associated with simple strategy versus complex strategy for bifurcation lesions.
Discussion
In the DES era, this updated meta-analysis demonstrated that the complex strategy had similar clinical safety (cardiac death and stent thrombosis) and efficacy (TLR, TVR) in the treatment of patients with coronary bifurcation lesions at follow-up, compared with the simple strategy. Patients following the complex strategy were associated with an increased risk of both early and follow-up MI. Subgroup analyses revealed that the complex strategy may be the optimal treatment for patients with true bifurcation lesions together with large side branches.
The incidence of MI was high, using the complex strategy for patients with coronary bifurcation lesions4,5,7. The recent patient-level pooled analysis from the Nordic and BBC ONE studies has shown that the incidence of periprocedural MI in the complex strategy group was 9.9% versus 3.5% in the simple strategy group (p<0.001)19. However, the DKCRUSH-II trial demonstrated a similar MI rate in patients with true bifurcation lesions undergoing either the DK-crush or provisional stenting at one-year follow-up (3.2% vs. 2.2%, p=0.75)13. It is reasonable to highlight that the definitions of MI were not consistent throughout the different studies. This lack of a unified definition was a criticism in reaching the conclusion. Thus, it is still speculative to conclude that the complex strategy was associated with concerns of a high degree of myocardial damage. In the current study, a significantly high rate of MI in the complex strategy was consistent with previous meta-analyses of RCTs9,10; however, it may not raise a safety concern due to the lack of correlation between periprocedural MI and cardiac death at clinical follow-up. A study by Vranckx et al has reported that type 4a MI may not be a reliable component of the primary composite endpoint in patients with acute coronary syndrome in a pooled analysis of the RESOLUTE all-comers trial20. Therefore, further evaluations are warranted to compare this endpoint between the two strategies, using the new universal definition of MI21.
Stent thrombosis may derive from multifactorial factors. There are a number of stent thrombosis risk factors in the complex strategy, including two-stent implantation, and complexity of the procedure. However, it is interesting to note that most of the individual RCTs failed to confirm the inferiority of the complex strategy at this endpoint. Undoubtedly, the insufficient power for achieving the statistical difference is probably the main reason. In the current study, with a relatively large sample size, we found that the incidence of stent thrombosis was similar between the complex and the simple strategy. It has been suggested that higher pressure post-dilation and frequent final kissing balloon inflation (FKBI) in the complex strategy potentially reduced the risk of stent thrombosis22. Conversely, most of the studies in the current study used first-generation DES, which partially increased the stent thrombosis risk of the complex strategy due to greater stent implantation23.
Whether the complex strategy in treating bifurcation lesions correlated with favourable clinical efficacy outcomes remains unsettled. According to the cost-effectiveness and time taken, the simple strategy with a simple technique and lower cost was preferred by interventional cardiologists in the majority of non-distal left main true bifurcations. Currently, the simple strategy is recommended in contemporary guidelines if the side branch is not large and has only mild or moderate focal disease at the ostium24. Long-term follow-up of the Nordic study has demonstrated that the simple strategy regarding the efficacy endpoints remained at least equal to the complex strategy25. Alternatively, consensus from the 7th European Bifurcation Club meeting also suggested that the simple strategy be recommended as the gold standard technique. On the other hand, the document highlighted that true bifurcations with large side branches and ostial disease extending more than 5 mm from the carina are likely to require a complex strategy26.
In the present study, it is impossible to address the impact of bifurcation classification and side branch characteristics on clinical outcomes between the simple and the complex strategy. True bifurcation lesions were not considered as mandatory inclusion criteria in the BBC ONE, BBK, and Nordic studies3,6,7. Relatively small side branches (namely reference vessel diameter <2.5 mm) were included in the study by Pan et al, and the CACTUS, BBK, and Nordic trials2,4,6,7. All these critical issues potentially increased side branch revascularisation at follow-up in patients with complex strategy. In contrast to earlier RCTs, the DKCRUSH-II trial showed that the complex DK-crush technique had less need for revascularisation in side branches compared with provisional stenting at follow-up. The favourable results in the DK group were associated with the fact that only patients with Medina 1,1,1 or 0,1,1 bifurcation lesions and reference side branch size ≥2.5 mm were enrolled13.
The DK-crush technique focusing on the performance and quality of double kissing inflation was associated with significantly reduced TVR in both main vessel and side branch27,28. The underlying mechanisms of less reintervention in patients with DK-crush technique have been preliminarily investigated. First, the first kissing immediately after balloon crush may optimise stent expansion and eliminate stent strut malapposition at the side branch ostium. Second, the FKBI rate is nearly 100%, with minimal unsatisfactory kissing29, subsequently leading to a better minimal lumen diameter in the side branch ostium. Third, a higher proportion of FFR value >0.8 and lower residual % diameter stenosis in the side branch were observed in the DK-crush technique compared with the provisional stenting technique30. The ongoing DK Crush V trial evaluating the performance of the provisional stenting and the DK-crush techniques for treating true distal left main bifurcations may offer more insight into the effect of the DK-crush technique on clinical events after PCI.
Apparently, all RCTs in the current study have several discrepancies with regard to enrolling different types of bifurcation lesions, vessel size of the side branch, types of DES, and mixing all two-stent techniques together. Furthermore, combining all two-stent techniques as the complex strategy may conceal the fact that some two-stent techniques are associated with detrimental clinical outcomes compared with others16,31. Future studies, possibly considering the above-mentioned characteristics, would be necessary to investigate further the clinical performance of simple and complex strategies in treating patients with true bifurcation lesions. Conversely, a new bifurcation classification adding information on lesion complexity may provide more confirmative comparison between the simple and the complex strategy.
Limitations
Our study has several limitations. First, this meta-analysis is not based on individual patient data. Second, crossover rate, duration of follow-up, stenting technique of the complex strategy, rates of use of IIb/IIIa glycoprotein inhibitors and FKBI were partially different among trials. To elucidate the relationship between these factors and stenting strategy, the potential sources of heterogeneity by subgroup were studied and meta-regression analyses were performed. Third, lack of angiographic or other invasive imaging modalities at follow-up did not allow us to investigate the impact of procedural strategy on clinical endpoints and the underlying mechanisms. Finally, the follow-up period in all enrolled studies was relatively short for comparison of complex strategy versus simple strategy.
Conclusions
The complex strategy remains an optional treatment for patients with coronary bifurcation lesions without severe concern regarding safety. The dissociation of the subgroups in the complex strategy group on reintervention is probably attributable to the novel DK-crush technique used in the DK subgroup.
| Impact on daily practice Randomised trials and previous meta-analyses have indicated “simple is better” for treating coronary bifurcation lesions. However, with the introduction of the novel two-stent technique (DK-crush), a complex strategy might remain optional for coronary true bifurcation lesions with larger-sized side branches in the newer-generation DES era. Moreover, the complex strategy might have less need of reintervention in the “complex” bifurcation lesion after DES implantation, without severe safety concerns. Future randomised trials with larger sample sizes and longer-term follow-up may provide a confirmative recommendation in choosing the simple or complex strategy for bifurcation lesions. |
Acknowledgements
The study was supported by the Jiangsu Provincial Special Program of Medical Science (BL2013001).
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
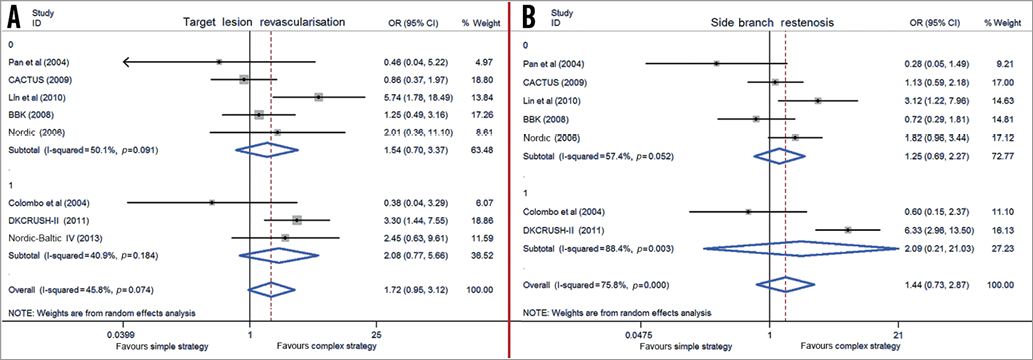
Online Figure 1. Forest plots from the included trials. Odds ratios of target lesion revascularisation (A), and side branch restenosis (B), associated with simple strategy versus complex strategy for bifurcation lesions in the large side branch subgroup.
Online Figure 2. Forest plots from the included trials. Odds ratios of target lesion revascularisation (A), and side branch restenosis (B), associated with simple strategy versus complex strategy for bifurcation lesions in the true bifurcation subgroup.

