Abstract
Background: Controversy still exists regarding the optimal treatment of coronary bifurcation lesions.
Aims: We aimed to analyse the evidence from randomised controlled trials (RCTs) to compare outcomes following different bifurcation stenting techniques.
Methods: We systematically searched for RCTs comparing different techniques published up to July 2022. We then conducted a pairwise meta-analysis to compare outcomes between provisional stenting (PS) versus upfront 2-stent techniques. Moreover, we performed a network meta-analysis (NMA) to compare all strategies with each other. The primary endpoint was major adverse cardiac events (MACE).
Results: Twenty-four RCTs (6,890 patients) analysed PS, T-stenting, double-kissing (DK)-crush, crush, or culotte stenting. The pairwise meta-analysis did not reveal a significant difference between the PS and 2-stent techniques. However, the prespecified sensitivity analysis, which included RCTs exclusively enrolling patients with true bifurcation lesions, showed a lower rate of MACE following 2-stent techniques, and meta-regression indicated that a longer side branch lesion was associated with a greater benefit from the 2-stent strategy, which was the most apparent in RCTs with a mean lesion length >11 mm. NMA revealed that DK-crush was associated with the lowest MACE rate (odds ratio 0.47, 95% confidence interval: 0.36-0.62; p<0.01; PS as a reference).
Conclusions: Overall, 2-stent techniques were not significantly better than PS in terms of clinical outcomes. However, the results of the sensitivity analysis suggested that there might be a benefit of a 2-stent approach in selected patients with true bifurcation lesions, especially in the case of long side branch lesions. An NMA revealed that DK-crush was associated with the lowest event rates when compared with other techniques.
Introduction
Since the introduction of percutaneous coronary interventions (PCIs), the treatment of lesions located at the coronary bifurcations presents a challenge due to the complexity of these interventions1. For that reason, clinical outcomes following PCI for coronary bifurcation lesions are still worse than interventions for other lesions2.
Multiple approaches have been developed for managing coronary bifurcation lesions, including various bifurcation stenting techniques3. The clinical outcomes of these techniques have been evaluated in several randomised controlled trials (RCTs), but the interpretation of individual trials is challenging because of comparisons of different strategies and inconsistent findings456. In recent years, several network meta-analyses (NMAs) have been performed to synthesise the results of RCTs on different bifurcation stenting strategies, but they did not include the latest trials789. Moreover, they were limited by comparing bifurcation stenting techniques with dedicated stents610 or analysing aspects of bifurcation treatment other than stenting strategies611.
The latest European Society of Cardiology (ESC)/European Association for Cardio-Thoracic Surgery (EACTS) 2018 Guidelines on myocardial revascularisation recommend provisional stenting (PS) as the first-choice approach for PCI of bifurcation lesions12. Nevertheless, the results of a few large RCTs have been published since the publication of these guidelines,789.
We aimed, therefore, to perform a pairwise meta-analysis assessing the outcomes of PS versus all 2-stent techniques considered together and an NMA to compare different stenting strategies to each other, based on the latest available evidence from RCTs.
Methods
This systematic review was prospectively registered in the PROSPERO (The International Prospective Register of Systematic Reviews) database before completing searches and starting study selection, screening against eligibility criteria, data extraction, risk of bias evaluation, or data analysis (registration number CRD42022340212). Our study conforms to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, including the PRISMA extension statement for reporting NMAs. The PRISMA NMA Checklist has been included in Supplementary Table 1.
Search strategy, data selection, and extraction
PubMed and Scopus were searched for original articles, published in English, presenting results of RCTs comparing different PCI techniques of coronary bifurcation lesion treatment. Searches were performed in July 2022, applying the terms “percutaneous coronary intervention,” “stenting,” “bifurcation,” and “randomised.” A search strategy is presented in Supplementary Table 2. Two co-authors independently performed the initial screening of articles by title and abstract. Then, full texts of reports potentially meeting inclusion criteria were obtained and evaluated for eligibility. Discrepancies between reviewers were resolved by consensus with the co-authors. RCTs were considered eligible for inclusion in the meta-analysis if at least 2 bifurcation lesion-stenting strategies were compared. We excluded reports without at least a 3-month clinical follow-up, RCTs evaluating bifurcation stenting techniques in chronic total occlusion lesions or using dedicated bifurcation stents, and trials assessing aspects of bifurcation treatment other than bifurcation stenting techniques. No restrictions were applied regarding publication year, sample size, or stent generation. In the case of multiple reports from the same trials, papers with the longest follow-up were included in the meta-analysis. Studies’ identification, screening, eligibility assessment, and inclusion have been depicted on the PRISMA flowchart (Figure 1).
The following data were extracted from eligible reports: the first author’s name/clinical trial name, publication year, number of participating centres, baseline clinical characteristics, angiographic and procedural characteristics, and endpoint definitions. In addition, 2 authors independently extracted outcome data (the number of events, the total number of cases in a given arm, and estimates with corresponding 95% confidence intervals [95% CIs]), and discrepancies were verified and resolved by consensus. Next, the included RCTs were assessed for bias independently by 2 co-authors using the Cochrane risk-of-bias tool for randomised trials version 2 (RoB 2), which encompasses the assessment of the randomisation process, deviations from the intended interventions, missing outcome data, and measurement of the outcome. Using this tool, the included RCTs were then classified as either having a low risk of bias, some concerns, or a high risk of bias. The results of bias evaluation (which represent the authors’ consensus) have been depicted on a diagram using a dedicated RoB 2 Excel tool (Supplementary Figure 1).
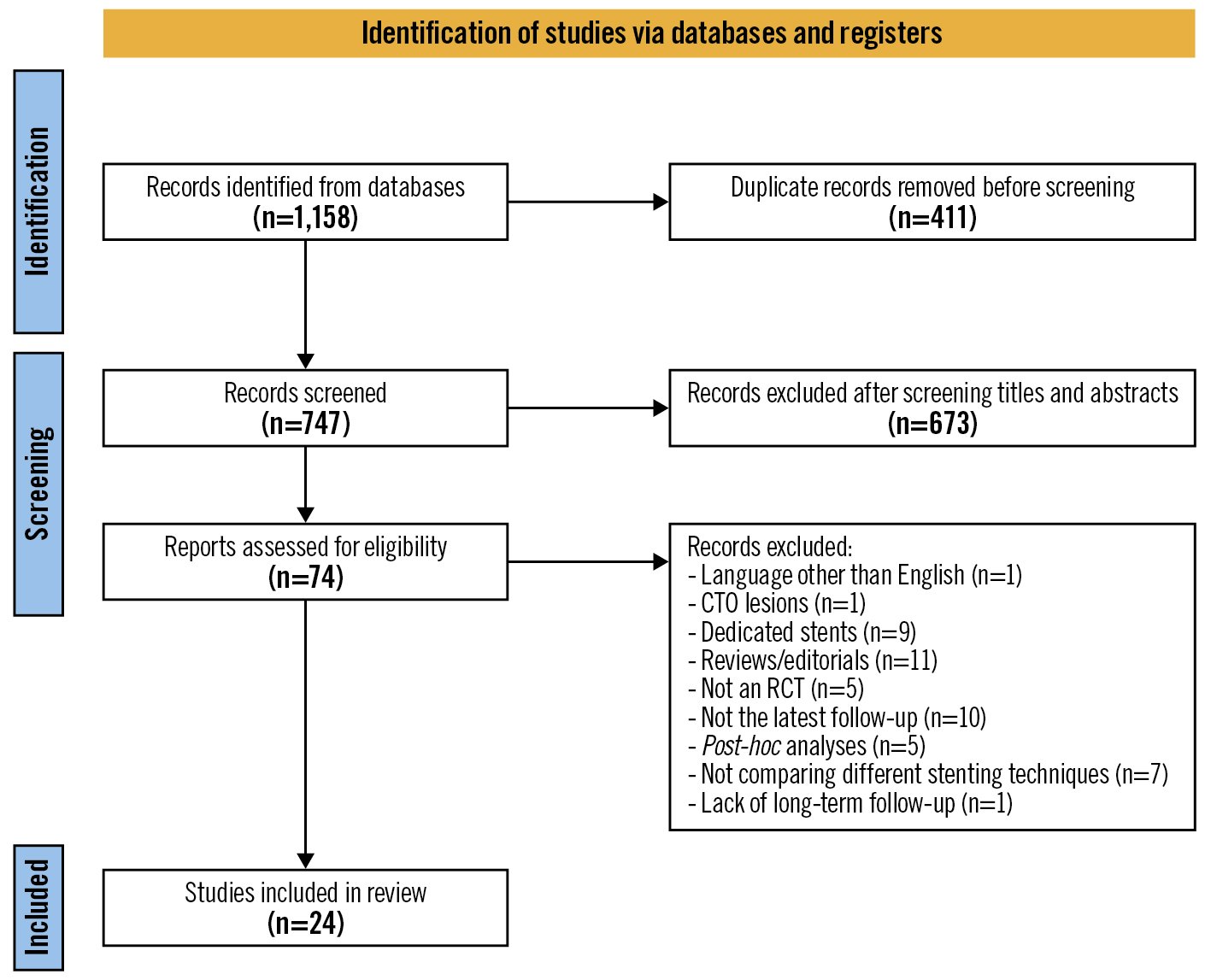
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart of randomised controlled trials included in the systematic review and meta-analysis. CTO: chronic total occlusion; RCT: randomised controlled trial
Study endpoints
The primary outcome of interest was a combined endpoint of major adverse cardiac events (MACE) at the longest available follow-up, defined according to the given study’s definition. If the MACE rate was not reported, MACE was considered a composite of cardiac death, myocardial infarction (MI), or target lesion revascularisation (TLR). Secondary analysed outcomes in this meta-analysis were cardiac death, MI, TLR, and stent thrombosis (ST) according to each trial’s protocol. The definitions of endpoints in the analysed RCTs are provided in Supplementary Table 3.
Statistical analysis
All statistical analyses were performed in R version 4.2.0 (The R Foundation for Statistical Computing) using packages “meta”, “metafor” and “netmeta.” Unless specified otherwise, categorical variables have been shown as the number of patients (percentages), and quantitative variables have been presented as the mean (standard deviation). Odds ratios (ORs) and hazard ratios with corresponding 95% CIs were used as relative treatment effect measures. All meta-analyses were performed according to the intention-to-treat approach. A 2-tailed p-value of less than 0.05 was considered significant.
Pairwise meta-analysis
A random-effects pairwise meta-analysis of binary outcomes data was conducted to compare PS versus 2-stent techniques. Heterogeneity in the meta-analysis was tested using Cochrane Q statistics. Moreover, we visually inspected the contour-enhanced funnel plots to assess small-study effects. In the prespecified sensitivity analyses, we included RCTs without a high risk of bias, RCTs that had enrolled only patients with true bifurcations, trials using only second-generation drug-eluting stents (DES), and RCTs in which the proximal optimisation technique (POT) had been required or encouraged by the study’s protocol (at least in the PS arm). We also performed a non-prespecified sensitivity analysis by including RCTs enrolling only patients with left main bifurcation lesions. Moreover, to identify the unexplained sources of heterogeneity in the pairwise meta-analysis, we created random-effects meta-regression models using the mean side branch lesion length and publication year as covariates. Owing to the remarkable differences in the follow-up duration between RCTs, we also performed a meta-regression by follow-up duration and sensitivity random-effects meta-analysis of time-to-event outcomes.
Network meta-analysis
A frequentist random-effects NMA was carried out to compare all bifurcation stenting techniques to each other using both direct and indirect evidence on treatment effects. The 2-stent arms of RCTs that allowed more than 1 technique in this group were allocated to the most frequently used strategy in a given arm. To illustrate the network, we generated network plots.
We have presented the network relative effects of treatment using forest plots, where PS was set as a reference. Moreover, we have shown relative treatment effects from the NMA and direct evidence in the league table. The league table’s lower triangle contains network treatment estimates from the NMA. The upper triangle incorporates direct treatment estimates from the pairwise comparisons.
The relative ranking of the treatments was estimated using p-scores, which can be interpreted as the mean extent of certainty that one treatment strategy is better than another treatment.
Heterogeneity among the results of included RCTs was assessed using the Q test. In addition, local inconsistency was checked by comparing direct and indirect treatment estimates. To evaluate the small study effects, we drew the “comparison-adjusted” funnel plots, which were assessed for asymmetry visually. Moreover, we performed prespecified sensitivity analyses after excluding RCTs with a high risk of bias and trials with multiple 2-stent techniques in 1 arm.
Results
Study selection and characteristics
After excluding duplicates, 747 records were screened, and after the title and/or abstract evaluation, 74 records were selected for a full-text assessment for eligibility. Finally, 24 RCTs − enrolling a total of 6,890 patients who had undergone bifurcation PCI using one of the following techniques: PS, T-stenting (including all its modifications)13, double-kissing crush (DK-crush), crush, or culotte stenting − were included in the review17891415161718192021222324252627282930313233. A PRISMA flowchart of study inclusion is presented in Figure 1, and the details of the included RCTs are shown in Table 1. Seven of these trials allowed more than 1 technique in the 2-stent arm. The weighted mean clinical follow-up in all RCTs was 26.2 months. Clinical and angiographic/procedural characteristics are presented in Supplementary Table 4 and Supplementary Table 5, respectively. The results of the risk-of-bias assessment of the analysed RCTs are depicted in Supplementary Figure 1.
Table 1. Details on included randomised controlled trials.
| Study | Publication year | Years of patient enrolment | Multicentre trial | First arm (n) | Second arm (n) | Predominant technique in 2-stent arm | Clinical follow-up (months) | Angiographic follow-up (months; percentage of patients) | DES generation | Routine FKB in the provisional arm (according to protocol) | POT in the provisional arm (according to protocol) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| BBC ONE27 | 2010 | 2004-2007 | Yes | Provisional, n=250 | 2-stent, n=250 | Crush, 67.6% | 9 | NA; NA | First | No | No |
| BBK I26 | 2015 | 2005-2006 | No | Provisional, n=101 | T-stenting, n=101 | NA | 60 | 9; 95% | First | Yes | No |
| BBK II28 | 2016 | 2010-2015 | No | Culotte, n=150 | Modified T-stenting, n=150 | NA | 12 | 9; 91% | First and second | NA | NA |
| CACTUS29 | 2009 | 2004-2007 | Yes | Crush, n=177 | Provisional, n=173 | NA | 6 | 6; 86% | First | Yes | No |
| Colombo et al1 | 2004 | 2001-2002 | Yes | 2-stent, n=63 | Provisional, n=22 | T-stenting, 93% | 6 | 6; 87.1% | First | Yes | No |
| DEFINITION II7 | 2022 | 2015-2018 | Yes | 2-stent, n=328 | Provisional, n=325 | DK-crush, 77.8% | 36 | 13; 54.5% | Second | No | Yes |
| DKCRUSH-I30 | 2009 | 2005-2006 | Yes | Crush, n=156 | DK-crush, n=155 | NA | 24 | 8; 82% | First | NA | NA |
| DKCRUSH-II31 | 2017 | 2007-2009 | Yes | DK-crush, n=185 | Provisional, n=185 | NA | 60 | 8; 91.6% | First | No | No |
| DKCRUSH-III32 | 2015 | 2009-2011 | Yes | DK-crush, n=210 | Culotte, n=209 | NA | 36 | 8; 83.5% | Second | NA | NA |
| DKCRUSH-V8 | 2019 | 2011-2016 | Yes | Provisional, n=242 | DK-crush, n=240 | NA | 36 | 13; 65.8% | Second | No | Yes |
| EBC MAIN9 | 2021 | 2016-2019 | Yes | Provisional, n=230 | 2-stent, n=237 | Culotte, 53% | 12 | NA; NA | Second | Yes | Yes |
| EBC TWO33 | 2016 | 2011-2014 | Yes | Provisional, n=103 | Culotte, n=97 | NA | 12 | NA; NA | Second | No | Encouraged |
| Lin et al14 | 2010 | 2007-2009 | No | Provisional, n=54 | 2-stent, n=54 | DK-crush, 65% | 8 | 8; ND | First | No | No |
| NBBS IV15 | 2020 | 2008-2012 | Yes | Provisional, n=221 | 2-stent, n=229 | Culotte, 65.6% | 24 | 8; 68.2% | First and second | No | No |
| NBS16 | 2013 | 2004-2005 | Yes | Provisional, n=207 | 2-stent, n=206 | Crush, 50% | 60 | 8; 86% | First | No | No |
| NSTS17 | 2013 | 2005-2007 | Yes | Crush, n=209 | Culotte, n=215 | NA | 36 | 8; 76.4% | First | NA | NA |
| Pan et al18 | 2004 | 2002-2003 | Yes | Provisional, n=47 | T-stenting, n=44 | NA | 6 | 6; 40.7% | First | NA | No |
| PERFECT19 | 2015 | 2007-2013 | Yes | Crush, n=213 | Provisional, n=206 | NA | 12 | 8; 71.6% | ND | No | No |
| Ruiz-Salmerón et al20 | 2013 | 2009-2011 | No | Provisional, n=33 | T-stenting, n=36 | NA | 9 | 9; 84.1% | Second | No | No |
| SMART-STRATEGY II21 | 2021 | 2013-2016 | Yes | Provisional, n=23 | 2-stent, n=23 | ND | 12 | 9; ND | Second | No | No |
| Ye et al22 | 2010 | 2008-2009 | No | DK-crush, n=25 | Provisional, n=26 | NA | 8 | 8; 21.6% | ND | No | No |
| Ye et al25 | 2012 | 2008-2011 | No | DK-crush, n=38 | Provisional, n=37 | NA | 12 | 8; 77% | First and second | No | No |
| Zhang et al23 | 2016 | 2010-2013 | No | Provisional, n=51 | Culotte, n=51 | NA | 9 | 9; 100% | First and second | No | No |
| Zheng et al24 | 2016 | 2013-2014 | No | Crush, n=150 | Culotte, n=150 | NA | 12 | 12; 84% | ND | NA | NA |
| BBC ONE: The British Bifurcation Coronary study: Old, New, and Evolving strategies; BBK I: Bifurcations Bad Krozingen I; BBK II: Bifurcations Bad Krozingen II; CACTUS: Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents; DEFINITION II: Two-stent vs Provisional Stenting Techniques for Patients With Complex Coronary Bifurcation Lesions; DES: drug-eluting stent; DKCRUSH-I: Study Comparing the Double Kissing Crush with Classical Crush for the Treatment of Coronary Bifurcation Lesions; DKCRUSH-II: Randomized Study on Double Kissing Crush Technique Versus Provisional Stenting Technique for Coronary Artery Bifurcation Lesions; DKCRUSH-III: DK Crush Versus Culotte Stenting for the Treatment of Unprotected Distal Left Main Bifurcation Lesions; DKCRUSH-V; EBC MAIN: The European Bifurcation Club Left Main Coronary Stent Study; EBC TWO: European Bifurcation Coronary TWO; FKB: final kissing ballon; NA: not applicable; NBBS IV: Nordic Baltic Bifurcation Study IV; NBS: Nordic Bifurcation Study; ND: no data; NSTS: Nordic Stent Technique Study; PERFECT: Optimal Stenting Strategy for True Bifurcation Lesions; POT: proximal optimisation technique; SMART-STRATEGY II: STRATEGY for Left Main Coronary Bifurcation Lesion II | |||||||||||
Pairwise meta-analysis comparing PS versus 2-stent techniques
This analysis, including 18 RCTs comparing these 2 strategies (5,022 patients), did not show any difference between the 2 groups regarding MACE (OR 1.19, 95% CI: 0.9-1.58; p=0.23) (Central illustration A) or any secondary outcomes (Supplementary Figure 2). In this analysis, significant heterogeneity was observed between the RCTs regarding MACE (Central illustration A), MI, and TLR (Supplementary Figure 2). Visual inspection of the contour-enhanced funnel plot for MI revealed asymmetry between the smaller RCTs, but the risk of publication bias was unlikely, since all the trials, except three large-scale trials, were located in the “area of non-significance” (Supplementary Figure 3).
Sensitivity analyses and meta-regression
Four prespecified sensitivity analyses were performed for pairwise meta-analysis. The first of them, including only RCTs enrolling patients with true bifurcations, demonstrated a significant benefit from 2-stent techniques in terms of MACE (OR 1.52, 95% CI: 1.08-2.13; p=0.02) (Central illustration B), mainly driven by a higher risk of TLR following PS (OR 1.64; 95% CI: 1.04-2.56; p=0.03) (Supplementary Figure 4). Other prespecified sensitivity analyses, i.e., after excluding RCTs with a high risk of bias, those using first-generation drug-eluting stents, or those without POT, did not show any significant advantage of the 2-stent technique over PS (Supplementary Figure 5-Supplementary Figure 7). Additionally, the non-prespecified sensitivity analysis, which included only left main bifurcations and a meta-analysis of the time-to-event data, also did not show any difference between the analysed arms (Supplementary Figure 8, Supplementary Figure 9). The statistical heterogeneity regarding the primary endpoint, MI, and TLR remained significant in the above-mentioned sensitivity analyses.
The meta-regression, using the mean side branch lesion length as a continuous covariate, showed lower rates of the primary endpoint of MACE associated with the 2-stent technique in the RCTs that had enrolled patients with longer side branch lesions (estimate of 0.06; 95% CI: 0.02-0.10; p=0.002; residual heterogeneity Q=17.07; p-value for residual heterogeneity of 0.15). This effect was apparent in the RCTs with a mean study-level side branch lesion length of more than 11 mm (Central illustration C). A similar relationship between side branch lesion length and the advantages of 2-stent techniques was also found for myocardial infarction and target lesion revascularisation (Supplementary Figure 10). Another meta-regression demonstrated that the RCTs published in recent years tended to show a lower rate of MI in patients treated with 2-stent techniques; other analysed outcomes were not associated with the publication year (Supplementary Figure 11). Of note, the follow-up duration did not modify the relationship between the 2-stent technique and the primary or secondary outcomes (Supplementary Figure 12).
Network meta-analysis comparing all techniques to each other
In the NMA, 22 RCTs were analysed for the primary endpoint of MACE. Two RCTs were not included in the NMA because of a lack of data on the predominate bifurcation stenting strategy in the 2-stent arm or missing results in the intention-to-treat analysis. The network plots for MACE and secondary endpoints are presented in Figure 2, and the number of patients analysed in the NMA, along with event rates according to the bifurcation stenting technique, are shown in Supplementary Table 6.
NMA revealed that DK-crush was associated with significantly lower event rates than all other bifurcation stenting strategies regarding the primary endpoint (OR 0.47, 95% CI: 0.36-0.62, as compared to PS, the second-best strategy in terms of MACE) and TLR. Moreover, DK-crush was related to a lower risk of MI and stent thrombosis compared to all other techniques, except for T-stenting. However, the rate of cardiac death in patients treated with DK-crush was similar to patients undergoing bifurcation PCI using other techniques. No other significant differences between bifurcation treatment strategies have been revealed. According to the p-scores, DK-crush ranked highest in terms of all analysed endpoints. The results of the NMA are shown both on the forest plots (using PS as a reference) (Central illustration D, Figure 3) and in the league table (Figure 4).
No heterogeneity nor local inconsistency between direct and indirect treatment estimates was revealed in NMA (Figure 4, Supplementary Table 7). Moreover, there was no significant asymmetry in the funnel plots, except for TLR (Supplementary Figure 13).
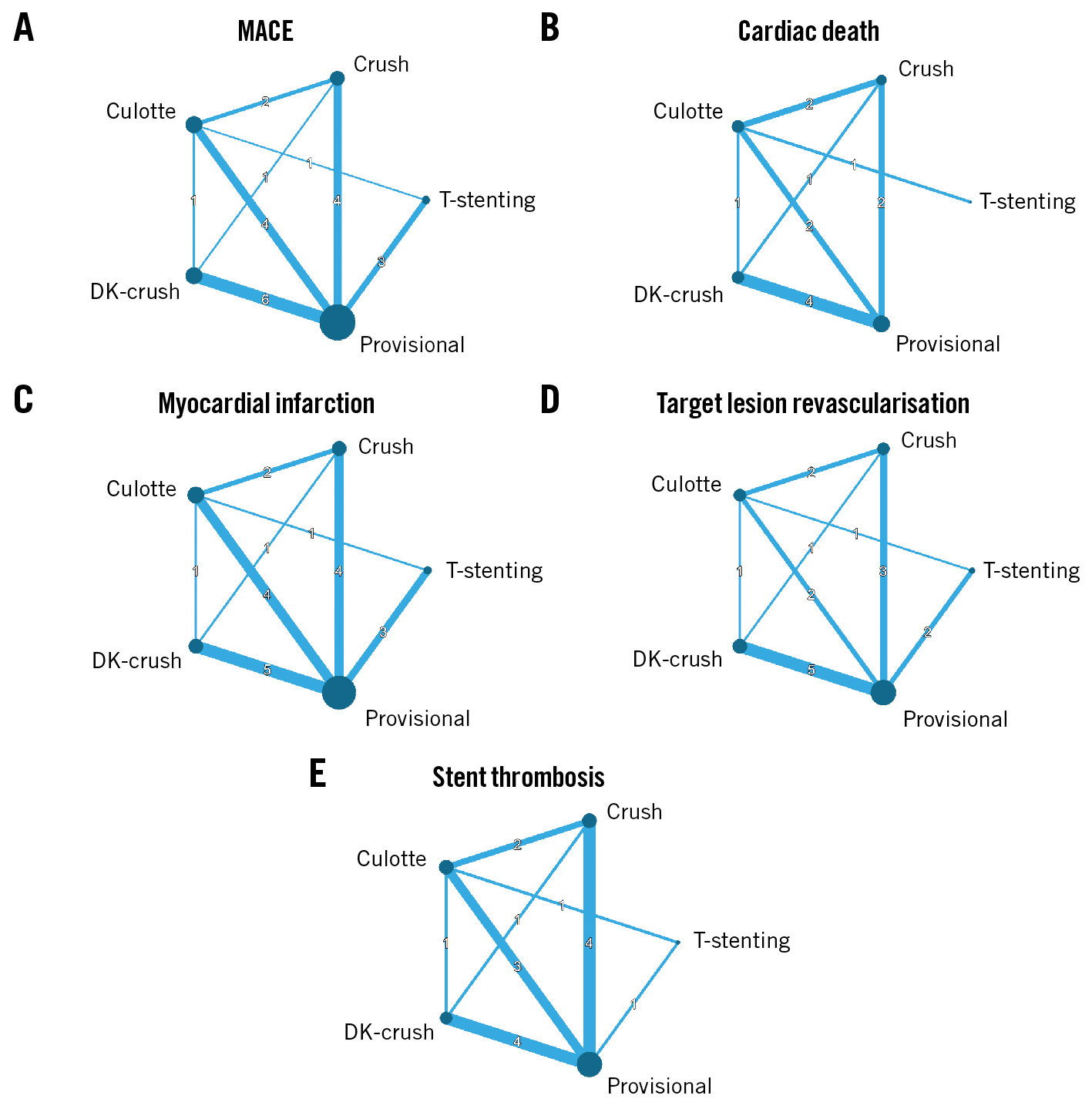
Figure 2. Network plots for MACE and secondary endpoints. A) MACE, (B) cardiac death, (C) myocardial infarction, (D) target lesion revascularisation, and (E) stent thrombosis. The size of the nodes corresponds to the number of patients randomised to a given strategy, and the thickness of connecting lines correlates with the number of available direct comparisons. DK-crush: double-kissing crush; MACE: major adverse cardiac events
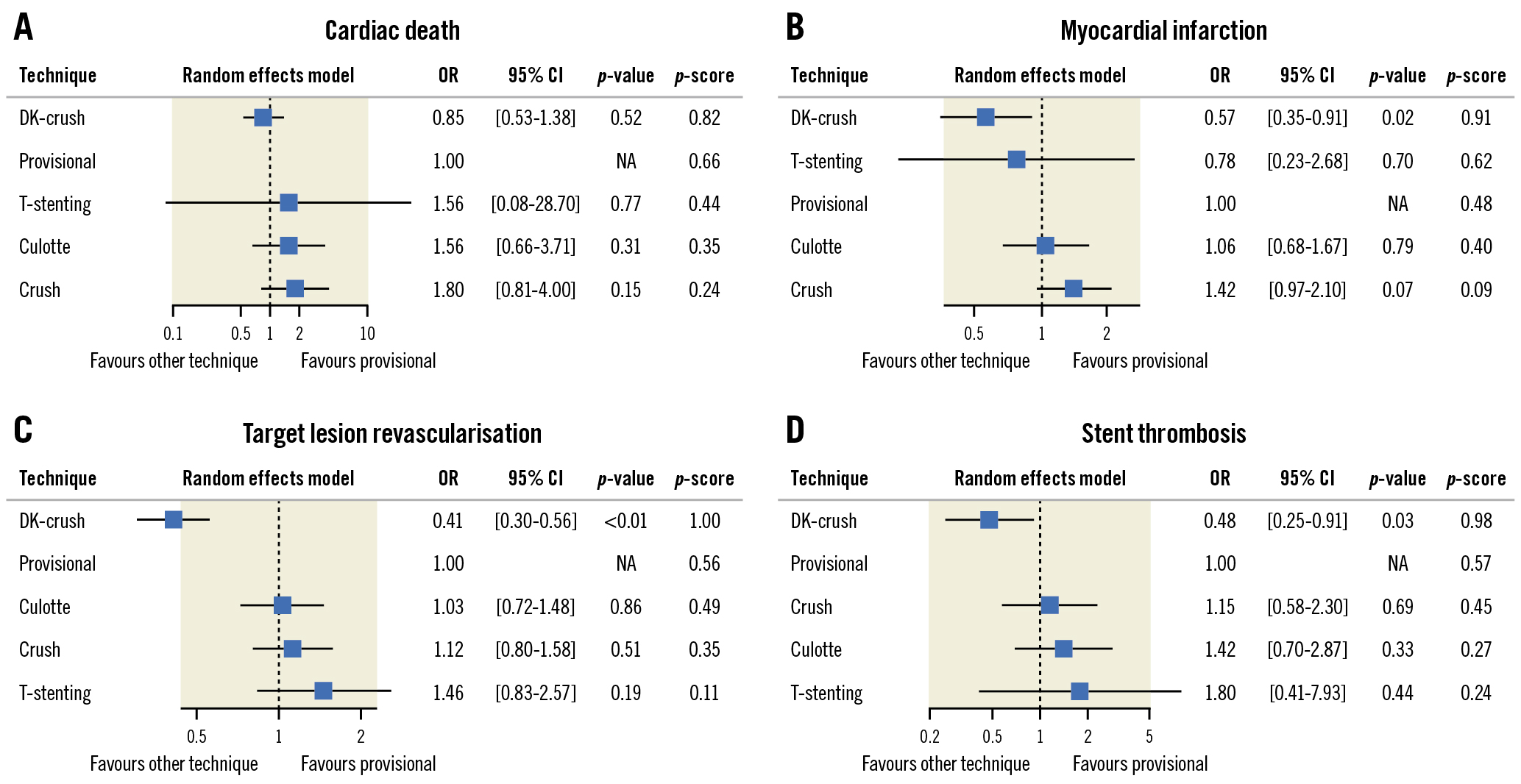
Figure 3. Forest plots and p-scores presenting the results of network meta-analysis for secondary outcomes. A) Cardiac death, (B) myocardial infarction, (C) target lesion revascularisation, and (D) stent thrombosis. Provisional stenting is shown as a reference. CI: confidence interval; DK-crush: double-kissing crush; NA: not applicable; OR: odds ratio
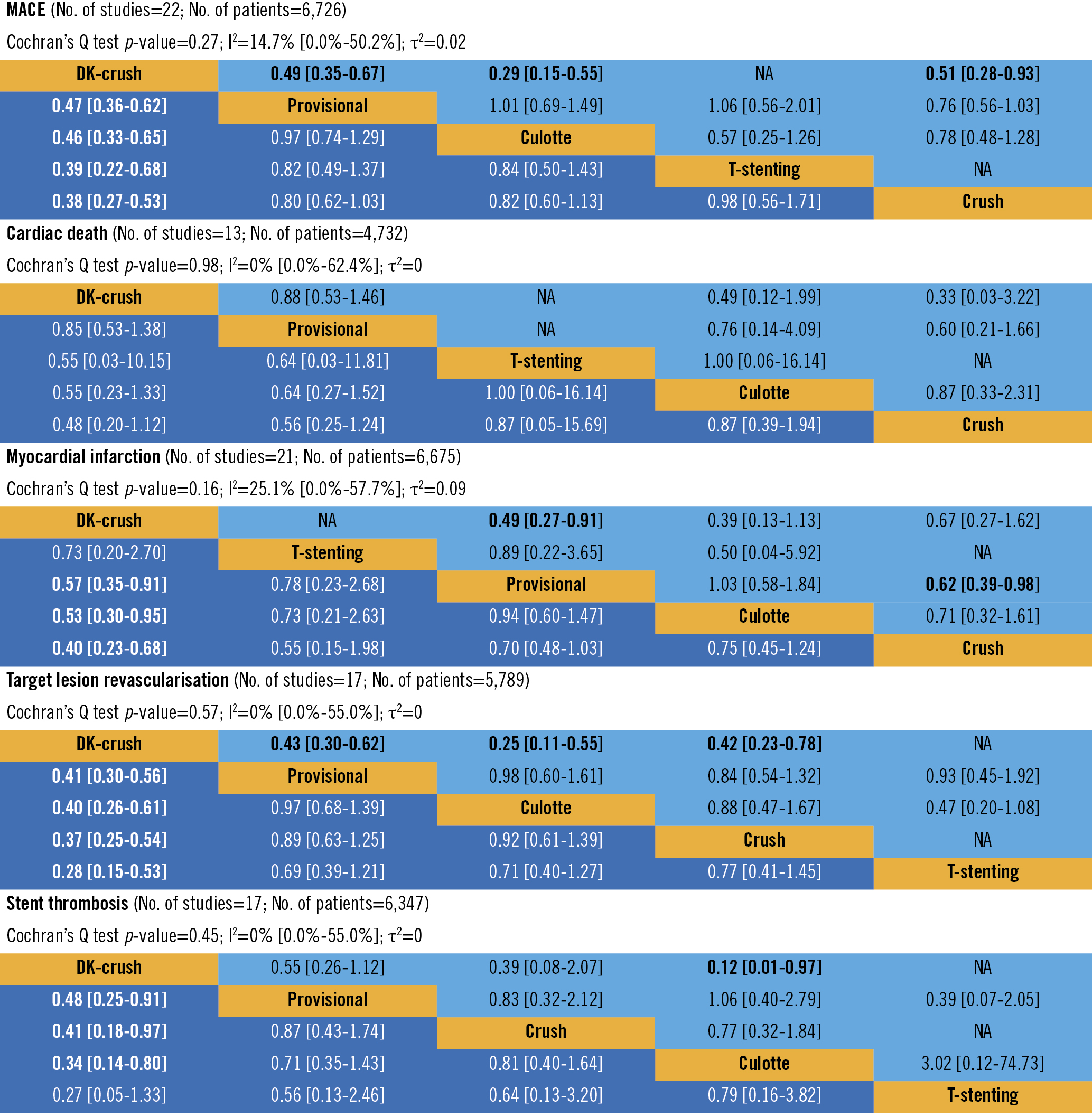
Figure 4. The results of the network meta-analysis presented using the league table. The lower triangle (dark blue boxes) contains network treatment estimates (odds ratios and 95% confidence intervals; comparison of treatment in a row versus a column), and the upper triangle (light blue boxes) contains direct treatment estimates from pairwise comparisons (comparison of treatment in a column versus a row). Significant differences in event rates between treatment strategies are in bold. DK-crush: double-kissing crush; NA: not applicable (lack of direct comparisons of 2 techniques in included trials).
Sensitivity network meta-analyses
The sensitivity analysis, after excluding the RCTs with a high risk of bias, revealed the same findings as the primary analysis (Supplementary Figure 14, Supplementary Figure 15). The second sensitivity analysis, without the RCTs that allowed for multiple techniques in 1 arm, provided similar results to the previous one, but DK-crush was not significantly better than PS regarding MI or stent thrombosis (Supplementary Figure 16, Supplementary Figure 17). In both of these sensitivity analyses, DK-crush was the best single strategy in terms of primary and secondary endpoints according to the treatment rankings.
Discussion
Our systematic review and meta-analysis on the percutaneous treatment of coronary bifurcation lesions have shown the following: 1) overall, there was no significant difference between PS and 2-stent techniques. 2) However, when only the RCTs with true bifurcation lesions were included, there was a lower risk of MACE in patients treated with 2-stent techniques. 3) The benefits of the 2-stent strategy were more apparent in patients with longer side branch lesions; this was especially observed in RCTs with a mean lesion length greater than 11 mm. 4) When considering all bifurcation strategies individually, DK-crush was associated with the lowest event rates compared to the observed rates of other techniques within each of the included trials.
Multiple RCTs have provided much of the evidence on different strategies of bifurcation lesion stenting by comparing a simple PS approach with complex upfront 2-stent techniques1789141516171819202122232425282930313233. However, the results of these RCTs have been somewhat contrasting, posing interpretive challenges. By pooling evidence from all available RCTs, we have shown that PS versus 2-stent techniques do not differ regarding MACE. This is in line with 2 previous meta-analyses634. Of note, as compared with a previous meta-analysis by Ford et al35, we did not detect any difference in cardiac death rates between these 2 techniques. Some essential differences should be considered when interpreting this difference. First, Ford et al included trials exclusively with long-term follow-up. Our meta-regression analysis, however, did not show the advantage of any strategy becoming more apparent over a longer follow-up. Second, 2 landmark trials on bifurcation stenting − EBC MAIN (The European Bifurcation Club Left Main Coronary Stent study) and the 3-year outcomes of the DEFINITION II trial (Two-stent vs Provisional Stenting Techniques for Patients With Complex Coronary Bifurcation Lesions) – were not included in the previous meta-analyses, but they were in ours6793435.
Of note, most of the trials included in this meta-analysis were still using first-generation DES and stenting techniques without POT1141516171823252628293031. To make our results more current, sensitivity analyses were performed including only those RCTs using second-generation DES and the POT technique, without any difference from our primary analysis. The lack of improvement may be due to the small number of RCTs included in these sensitivity analyses (6 and 4 trials, respectively). There is still a need for RCTs that include routine POT and final kissing-balloon in the 2-stent techniques, as well as with a greater use of intravascular imaging, which nowadays represents the gold standard for managing bifurcation lesions5.
Specifically, looking at the RCTs that only included patients with true bifurcation lesions, we showed a lower risk of MACE in the 2-stent versus 1-stent strategy, which, to the best of our knowledge, is a novel finding. However, considering the significant heterogeneity of the included trials, these results suggest improved outcomes in selected patients treated with 2-stent techniques rather than all patients with true bifurcations. For example, subgroup analyses of previous NMAs have shown an advantage of the 2-stent approach only in RCTs where the mean side branch lesion length ≥10 mm636. Nevertheless, this cut-off in the previous meta-analyses was selected somewhat arbitrarily. Therefore, taking this into account, we performed a meta-regression which demonstrated that the longer the mean study-level side branch lesion was, the greater the advantage of the 2-stent strategy. This was the most apparent in RCTs with a mean length of more than 11 mm. This finding seems to reaffirm the current European Bifurcation Club recommendations to consider an upfront 2-stent strategy if the side branch lesion length is >10 mm5. However, bearing in mind the limitations of the meta-regression, it should be interpreted with caution, as this analysis was observational in nature and referred to the study-level rather than patient-level data. Hence, the exact mechanism of the lower incidence of MACE in the 2-stent arms of trials with longer mean side branch lengths remains unclear.
Our NMA, in analysing all the bifurcation techniques individually, demonstrated excellent outcomes with the DK-crush technique, in line with multiple RCTs and previous NMAs61136. Contrary to the previous NMA by Di Gioia et al, our meta-analysis demonstrated the benefit of DK-crush, not only in terms of MACE and TLR but also with lower rates of MI and ST. This might be explained by the consideration in our analysis of the 3-year outcomes of the DEFINITION II trial, which included only very complex true bifurcations, where the advantage of DK-crush is the greatest. It is noteworthy to consider, when interpreting the results of RCTs with a limited number of enrolling centres whose operators are highly familiar with DK-crush (e.g., in the DKCRUSH-V trial, the primary operators’ previous DK-crush cases were reviewed by the steering committee before starting randomisation to ensure appropriate technique), that the reproducibility of these trials’ findings in real life is limited5. DK-crush is indeed time- and resource-consuming and requires more experience than the other stenting strategies5. In the recent EBC MAIN trial, for example, DK-crush was used only in 5% of cases in the 2-stent arm, demonstrating low utilisation of this technique in European centres. Owing to this, the clinical applicability of findings from the pairwise meta-analysis comparing PS with all 2-stent techniques might be higher than the results of the NMA, especially in the case of centres/operators that are not experienced in performing DK-crush.
A substantial amount of between-trial heterogeneity in the pairwise meta-analysis regarding MACE, MI, and TLR, which remained significant in multiple sensitivity analyses, must be acknowledged. This variation in trial outcomes may result, for example, from differences in study design, endpoint definitions, and patients’ clinical and angiographic characteristics. High between-trial heterogeneity might also be explained by differences in the outcomes of techniques included in the 2-stent strategy arm. Of note, we demonstrated a substantial decrease in residual heterogeneity in the meta-regression, indicating the potential effect of study-level side branch lesion length on the benefit of 2-stent techniques. However, as discussed above, this finding should be interpreted as hypothesis-generating rather than confirmatory.
Although some NMAs analysing different bifurcation stenting techniques have been published in recent years610113436, our paper presents some remarkable novelties. First, our analysis included the recent landmark trials, which provided much new data on the role of particular techniques in the treatment of bifurcation lesions79. Second, the prespecified sensitivity analysis, which included studies exclusively enrolling patients with true bifurcation lesions, showed a potential benefit of 2-stent techniques in this specific subgroup of patients. Third, the meta-regression showed that the longer the mean side branch lesion was (as a continuous variable), the greater the advantage of the 2-stent strategy. Fourth, we performed the whole spectrum of prespecified sensitivity analyses to assess the evidence on bifurcation techniques in the current bifurcation treatment scenarios by including RCTs utilising second-generation DES or POT.
Limitations
Some limitations should be acknowledged. First, the definitions of endpoints differed across the included RCTs, especially regarding MACE, which was considered in our meta-analysis according to the given study’s definition. Moreover, Bifurcation Academic Research Consortium criteria for standardised endpoints in coronary bifurcation studies have been recently published37. Owing to this, these standardised definitions were not used in the RCTs included in our meta-analysis. However, the results for secondary endpoints, for which the definitions varied to a lesser degree than those for the primary endpoint, were mainly consistent with the MACE findings.
In addition, RCTs analysed in our paper differed significantly regarding follow-up length. However, meta-regression showed that the follow-up duration did not affect the results. Furthermore, the sensitivity analysis of time-to-event data (available only for 8 of 18 RCTs included in the pairwise meta-analysis) was consistent with the meta-analysis of binary-outcome data.
The trials included were also of mixed quality. Notably, in the older trials the risk of bias was generally higher. In addition, as operators could not be blinded to patient allocation, the included RCTs were not double-blinded, which is a potential source of bias. However, the sensitivity analyses, after excluding the RCTs with the highest risk of bias, demonstrated results consistent with the primary analysis. Moreover, meta-regression by the publication year revealed that the findings of the meta-analysis were consistent across all years except for myocardial infarction (newer RCTs tended to show more benefit from 2-stent techniques in terms of this endpoint).
There was a relatively high crossover rate, especially in the case of RCTs analysing PS versus 2-stent techniques. Unfortunately, our meta-analysis was performed based only on the intention-to-treat principle (23 of 24 RCTs included in the review provided sufficient data for this analysis), as data on per-protocol or as-treated analyses were not routinely reported. However, this high crossover from 1-stent to 2-stent techniques reflects the modern PS approach. Thus, the clinical applicability of the intention-to-treat analysis is the greatest4.
Additionally, 6 of the RCTs included in NMA allowed for more than 1 technique in the 2-stent strategy arm. In these cases, we allocated these groups to the most frequently used technique in a given arm, which varied from 50% to 93%. Owing to this limitation, we conducted a sensitivity analysis by excluding these RCTs, which provided similar findings as the primary analysis.
Finally, there were considerable differences in terms of devices utilised (i.e., drug-eluting stent generations), interventional techniques (including POT and final kissing-balloon inflation), and bifurcation anatomies (for example, the prevalence of true bifurcations, left main bifurcations, vessel sizes, and lesion lengths), which might explain the heterogeneity of the results. We were able to address some of these issues by performing several sensitivity and meta-regression analyses. However, the others required the use of individual patient data, which were unavailable.
Conclusions
In the treatment of coronary bifurcation lesions, overall, 2-stent techniques were not significantly better than PS. However, there might be some benefit from 2-stent techniques in selected patients with true bifurcation lesions, especially in those with longer side branch lesions. Moreover, when bifurcation stenting techniques are analysed individually at the network level, DK-crush was associated with lower event rates as compared with other techniques.
Impact on daily practice
This meta-analysis demonstrated no advantage of the routine use of 2-stent techniques in patients with coronary bifurcation lesions. However, the results of the sensitivity analysis suggest that there might be a benefit of a 2-stent approach in selected patients with true bifurcation lesions, especially in the case of long side branch lesions. In addition, a network meta-analysis revealed that DK-crush is associated with the lowest event rates compared to all other techniques.
Acknowledgements
The first author (K. Bujak) was supported by the 2021 EAPCI Education and Training Grant. The authors have not received any specific funding for conducting this review.
Conflict of interest statement
D. Milasinovic reports speaker fees from Abbott, Terumo, Boston Scientific, and Biosensors. G. Stankovic reports personal fees from Medtronic, Terumo, Boston Scientific, and Abbott Vascular, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.