Abstract
Aims: Previously, we reported that the nine-month angiographic result after treatment of coronary bifurcation lesions with provisional T-stenting was not significantly different from that with routine T-stenting. To compare long-term clinical outcomes of the two stenting strategies, we extended the follow-up of our study on bifurcation stenting.
Methods and results: One hundred and one patients with coronary bifurcation lesions had been randomly assigned to provisional T-stenting and 101 to routine T-stenting, using sirolimus-eluting stents. We performed complete five-year follow-up. The primary efficacy endpoint was the incidence of target lesion revascularisation (TLR), and the primary safety endpoint was the incidence of definite/probable stent thrombosis (ST). We also monitored death, myocardial infarction (MI) and MACE (composite of death, MI and TLR). The cumulative five-year incidence of TLR in the provisional T-stenting arm was not significantly different from that in the routine T-stenting arm (16.2% vs. 16.3%, p=0.97). The same was true for MACE (22.8% vs. 22.9%, p=0.91), the composite of death and MI (9.9% vs. 13.9%, p=0.40), and ST (2.0% vs. 5.1%; p=0.25).
Conclusions: During five-year follow-up, routine T-stenting offered no advantage over provisional T-stenting with respect to TLR or MACE. ClinicalTrials.gov Identifier: NCT00288535
Introduction
In percutaneous coronary intervention (PCI) of bifurcation lesions, there are two competing procedural strategies1. According to the complex strategy, a stent is placed in both the main branch and the side branch. Alternatively, the simple strategy intends to stent the main branch only, while the side branch may be treated with plain kissing balloon angioplasty and only receives a stent as bail-out for threatened closure. Our knowledge of the long-term risks and benefits of the two stenting strategies for coronary bifurcation lesions is limited. Here, we report five-year outcomes of the Bifurcations Bad Krozingen (BBK) I study2 comparing routine T-stenting with provisional T-stenting for de novo coronary bifurcation lesions.
Methods
STUDY DESIGN
The design and two-year results of the BBK I study have been published previously2. For the current pre-specified analysis, we performed a systematic five-year follow-up. All information derived from contingent hospital readmission records or provided by the referring physician or by the outpatient clinic was entered into the computer database.
The catheter technique as well as pre-, peri-, and post-procedural management have been described in detail in our previous publication2. We always stented the main branch first, followed by routine or provisional placement of a side branch stent, as randomised. In the provisional T-stenting arm, high-grade residual stenosis (>75%) or flow-limiting dissection (TIMI flow <3) was required for justification of a side branch stent. Irrespective of stent placement in the side branch, we always performed a final kissing balloon dilatation. We recommended dual antiplatelet therapy for six months after PCI, followed by single antiplatelet therapy, mostly aspirin, indefinitely.
STUDY ENDPOINTS
The primary efficacy endpoint of the current five-year clinical follow-up was the incidence of target lesion revascularisation (TLR) in the intention-to-treat population. We assessed the incidence of definite/probable stent thrombosis (ST) as the primary safety endpoint, applying the criteria of the Academic Research Consortium. We monitored all-cause death, the composite of all-cause death and myocardial infarction (MI), and the composite of all-cause death, MI and TLR (major adverse cardiac events [MACE]) as secondary endpoints. The definitions of these endpoints were the same as previously described2. Events were adjudicated by two physicians not involved in the follow-up process.
STATISTICAL METHODS
For all statistical analyses, we used SPSS software package, Version 16 (SPSS Inc., Chicago, IL, USA). All tests were two-sided and statistical significance was set at 5%. We report discrete variables as counts (percentages) and continuous variables as mean±standard deviation. For discrete variables, we tested differences between groups with the χ2 test or Fisher’s exact test when expected cell sizes were less than five. We used the two-tailed t-test to compare continuous variables.
Cumulative event rates were calculated and graphically described according to the Kaplan-Meier method. A p-value of less than 0.05 was regarded as significant.
Results
STUDY POPULATION
The BBK I study enrolled 202 patients treated with sirolimus-eluting stents. We randomly assigned 101 patients to routine T-stenting and 101 to provisional T-stenting. There were no significant differences between the two study groups in any of the baseline clinical, angiographic or procedural characteristics2. The mean age of our study population was 67 years and 79% of the patients were male. Diabetes mellitus was prevalent in 22%. Three quarters of the bifurcation lesions were located in the territory of the left anterior descending coronary artery and 68% were true bifurcation lesions.
In three patients assigned to routine T-stenting, the main branch stent could not be crossed with the side branch stent. Vice versa, in 19 patients assigned to provisional T-stenting, a stent was implanted in the side branch because of high-grade residual stenosis in 14 patients or because of a flow-limiting dissection in five patients.
FIVE-YEAR CLINICAL OUTCOMES
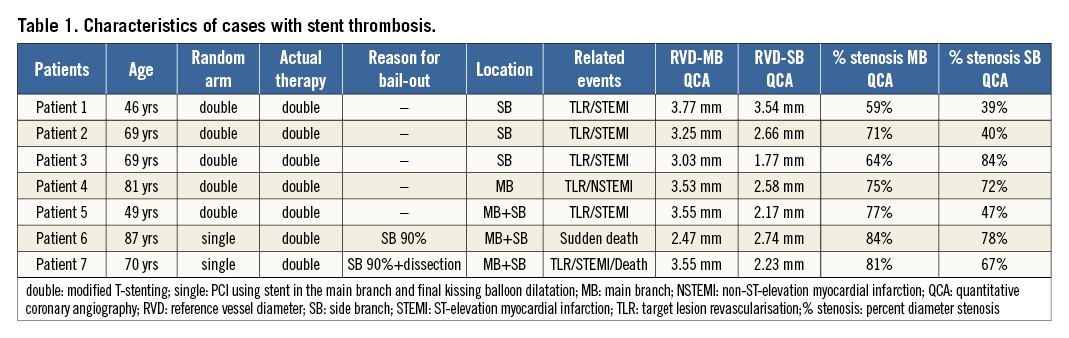
Clinical follow-up for five years after index PCI was available for all randomised patients. Our primary efficacy endpoint, the cumulative incidence of TLR during five-year follow-up was reached in 16.2% of the patients assigned to provisional T-stenting and in 16.3% and of the patients assigned to routine T-stenting (p=0.97) (Figure 1A). The five-year incidences of death were 7.9% in the provisional T-stenting arm versus 10.0% in the routine T-stenting arm (p=0.65) and those of the composite of death and MI 9.9% versus 13.9% (p=0.40), respectively (Figure 1B, Figure 1C). Thus, MACE occurred in 22.8% of the patients assigned to provisional T-stenting and in 22.9% of the patients assigned to routine T-stenting (p=0.91) (Figure 1D). The five-year incidence of definite/probable ST was numerically lower in the provisional T-stenting arm as compared with the routine T-stenting arm, albeit without reaching statistical significance (2.0% versus 5.1%; p=0.25) (Figure 2). ST did not occur in any patient treated only with main branch stenting (Table 1). Double stenting in the provisional T-stenting arm was associated with a distinctly elevated risk: five-year incidences reached 10.5% for definite/probable ST, 33.1% for TLR and 36.8% for MACE.
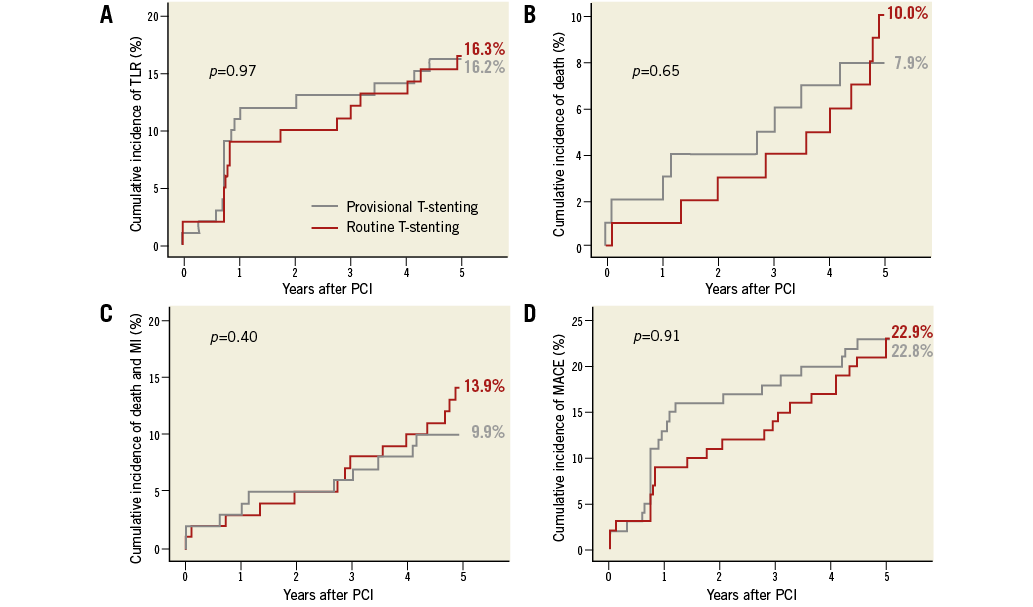
Figure 1. Kaplan-Meier curve estimates for cumulative event rates in patients with provisional T-stenting (grey) and routine T-stenting (red). A) Target lesion revascularisation (TLR). B) Death. C) Composite of death and/or myocardial infarction. D) Major adverse cardiac events (MACE). p-value by log-rank test.
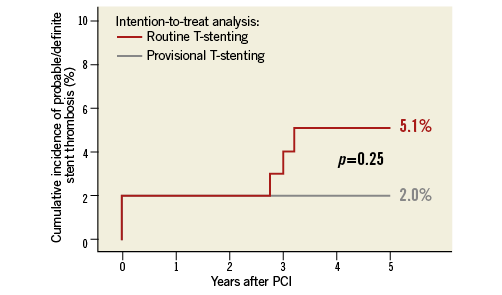
Figure 2. Kaplan-Meier curve estimates for definite/probable stent thrombosis rates with provisional T-stenting (grey) and routine T-stenting (red). p-value by log-rank test.
Discussion
As the key result of the five-year follow-up of the randomised BBK I study2, we found that in the long run routine T-stenting of coronary bifurcation lesions is similarly efficacious to provisional T-stenting. The TLR and MACE rates were equal in both study groups. Nevertheless, the need for double stenting in the provisional T-stenting arm was associated with a high risk of adverse events, including definite/probable ST. In the overall analysis, this resulted in numerically higher incidences of definite/probable ST and of the composite of death and MI after routine T-stenting compared with provisional T-stenting. Reassuringly, this did not affect survival, as five-year mortality rates were similar in both study arms.
The distinct risk of adverse events in patients assigned to provisional T-stenting who had a stent placed in the side branch is noteworthy. Bifurcation lesions which could not be treated adequately without a side branch stent appeared to carry an increased risk of subsequent thrombotic or restenotic events, independent of the potential risk imposed by complex stenting. Patients with double stenting substantially deteriorated the overall outcome of the provisional T-stenting group.
The long-term results of BBK I we report here expand the results of the five-year follow-up of NORDIC I3, published recently. NORDIC I reported a trend to higher TLR and MACE with complex versus simple stenting for bifurcation lesions. The incidences of definite/probable ST in NORDIC I were somewhat lower than in BBK I, possibly due to a lower risk profile (younger patients and a lower prevalence of diabetes mellitus). Moreover, the sample size of NORDIC I was roughly twice that of BBK I. On the other hand, BBK I applied a highly homogeneous procedural technique – T-stenting and systematic final kissing balloon dilatation performed in all study patients. This approach may have reduced potential confounders interfering with the detection of differences in outcome between complex and simple stenting.
Limitations
BBK I was powered for its primary angiographic endpoint, but not for clinical endpoints, which is a major limitation of this analysis. Only first-generation DES (sirolimus-eluting stents) were used in BBK I.
Conclusions
During five-year follow-up, routine T-stenting offered no advantage over provisional T-stenting with respect to ischaemic outcomes.
| Impact on daily practice According to our study, PCI of coronary bifurcation lesions should be performed with a simple stenting strategy, i.e., stenting of the main branch and kissing balloon dilatation of the side branch if needed. Patients in whom stenting of the side branch cannot be avoided, because of threatened closure or high residual stenosis of a major branch, must be considered as being at higher risk and deserve particular attention subsequently. |
Acknowledgements
The study was supported in part by a grant from Cordis. Cordis did not interfere with the design and conduct of the study, analysis and interpretation of the data or preparation, review, and approval of the manuscript.
Conflict of interest statement
M. Ferenc has received speaker honoraria from Cordis. The other authors have no conflicts of interest to declare.