Abstract
Bifurcation lesions remain a therapeutic challenge and present an increased risk of complications. It also seems clear that the provisional stenting strategy, using only one drug-eluting stent in the main vessel (MV), is the first choice of treatment for most patients. However, provisional stenting is not a unitary approach, and diverse technical possibilities such as the use of final kissing balloon inflation, or the type of drug-eluting stent implanted at the MV may influence the outcome of the procedure. In the context of provisional stenting, predilation of the side branch (SB) before MV stent implantation is another manoeuvre which could facilitate the performance of this technique. However, SB predilation has generated many controversies and it has been discussed at length during several sessions of the European Bifurcation Club meetings. In this paper we analyse the advantages and disadvantages of side branch predilation as well as the most relevant articles dealing with this topic. We conclude that predilation of the SB is in many cases probably not needed, but may be considered in order to simplify the procedure. Predilation of the SB is recommended when SB compromise after MV stenting is highly anticipated, such as in long ostial SB lesions or heavily calcified lesions.
Background
Several randomised trials have found that the elective two-stent technique was not superior to the provisional approach for coronary bifurcation lesions1-3. As a result, selective side branch (SB) intervention after main vessel (MV) stenting is now regarded as the standard strategy for most bifurcation lesions4,5. The risk of compromising the ostium of the SB may lead some operators to prefer a two-stent technique in complex bifurcation lesions with vessel dimensions above 2.75 mm. To prevent or overcome SB ostial compromise, several techniques, such as jailed wire or predilatation of the SB, have been introduced. Although predilatation could retain the patency of the SB after MV stenting and make the procedure simple, the benefit of this strategy is still a topic of debate.
Potential advantages and disadvantages of SB predilatation
Predilatation of the SB origin before MV stenting has the potential to maintain SB Thrombolysis In Myocardial Infarction (TIMI) flow and access to the SB after MV stenting. Therefore, predilatation could improve the procedural success rate of the SB through decreasing the rate of SB compromise and facilitating the subsequent re-crossing of the SB6. In addition, predilatation of the SB before MV stenting might be the ultimate SB treatment without the need for rewiring and post-dilatation of the SB. This enables the MV stent to preserve the original geometry, avoiding additional SB intervention (Figure 1).
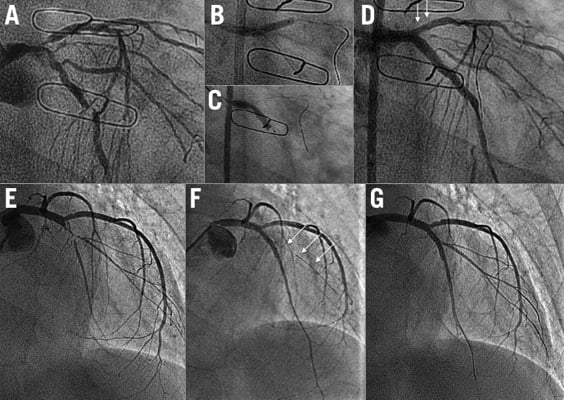
Figure 1. Examples of bifurcation lesions treated with (A-D) or without (E-G) side branch predilatation. In the first example, a bifurcation lesion at distal left main (A), predilatation of the side branch (B) followed by main vessel stent implantation (C) obtained an excellent immediate result (D) with neither rewiring nor balloon post-dilation of the side branch. In the second example, a bifurcation lesion at left anterior descending artery/diagonal branch (E), the non-predilated side branch (arrows) became occluded after main vessel stent implantation (F). Finally, the side branch was rescued and an excellent final result was also obtained (G).
Predilatation of the SB may lead to dissection of the SB, which may hamper access to the SB through the struts of the MV stent. It would also increase the possibility of potentially unnecessary kissing balloon inflation and/or SB stenting7. Previous studies have found that predilatation of the SB was associated with a higher rate of crossover to SB stenting during the provisional SB approach2,6.
Dedicated studies assessing SB predilatation before main vessel stenting
There has been a paucity of clinical studies assessing the impact of SB predilatation before MV stenting on procedural and long-term clinical outcomes in patients with true coronary bifurcation lesions. To date, only three studies are available: one is a randomised clinical trial and the other two are observational registries6,8,9.
The COBIS (COronary BIfurcation Stent) registry is a multicentre registry dedicated to bifurcation lesions treated solely with drug-eluting stents in order to investigate long-term clinical outcomes in a real-world practice. Using data from the COBIS registry, the effect of SB predilatation on procedural and long-term clinical outcomes in percutaneous coronary intervention for true non-left main bifurcations using a provisional approach was assessed6. The study cohort consisted of a predilatation group (n=175) and a non-predilatation group (n=662). Final kissing ballooning and crossover to a two-stent technique were more frequent in the predilatation group. At 21-month follow-up, the predilatation group had higher incidences of target vessel failure and target vessel revascularisation. Even after multivariate analysis, SB predilatation was still associated with the more frequent occurrence of target vessel failure (adjusted hazard ratio 2.11, 95% confidence interval 1.27-3.50, p=0.004). Results were maintained after a propensity score-matched population analysis. They concluded that SB predilatation before MV stenting is associated with an increased risk of repeat revascularisations. However, this study was not randomised and therefore potential confounding factors may have significantly affected the results. Predilatation of the SB was performed more frequently in patients with unfavourable lesion characteristics according to the operators’ decision. Despite propensity score adjustment in this retrospective registry, it is still likely that unmeasured confounders could have played a major role in the current series affecting the study results. Therefore, these results should be considered as hypothesis-generating and require confirmation in large randomised trials.
Pan et al randomised 372 patients with true bifurcation lesions to provisional stenting with (n=187) or without (n=185) SB predilatation to evaluate the effect of SB predilatation on procedural outcomes8. This paper studied relatively large side branches (reference vessel diameter=2.4 mm) and included the left main. The primary endpoint was the determination of TIMI flow at the SB after MV stent implantation. The prevalence of TIMI flow 0-1 after MV stenting was lower with predilatation than without (1% vs. 10%; p<0.001). TIMI flow less than three was also reduced after predilatation of the SB (p<0.001). Only 68% of patients in the predilatation group required further intervention due to suboptimal results (stenosis >50% or TIMI flow <3) compared with 100% of those in the non-predilatation group (p=0.001). In addition, there were no adverse effects from SB predilatation in the event that further intervention was required. In patients who required post-dilatation there were similar levels of inability to cross the lesion and rewiring time in both groups. The one-month and six-month clinical outcomes were similar between the groups. This study concluded that predilatation of the SB resulted in improved TIMI flow after MV stenting and less indication to subsequent treatment of the SB in patients with true bifurcation lesions during the provisional approach. However, TIMI flow in the SB during the procedure has very limited clinical impact as a primary outcome. The predilatation of the SB resulted in improved TIMI flow, but the rate of final TIMI flow was similar in both groups. Moreover, this study failed to demonstrate the superiority of SB predilatation over no SB predilatation in terms of clinical outcome. In addition, the criteria of SB ballooning after MV stenting, which were SB TIMI flow <3 and SB stenosis >50% in the present study, seem to be inappropriate. Because this study solely included true bifurcation lesions, which had more than 50% stenosis of the SB, all patients in the non-predilatation group needed to undergo SB balloon dilation after MV stenting. So, this study compared SB predilatation before MV stenting versus SB dilatation after MV stenting rather than SB predilatation versus no SB predilatation. SB balloon dilatation after MV stenting is not routinely performed in real-world practice.
A direct comparison of the two studies is difficult9 due to the differences in included population, design and methodology. The study of Song et al6 included a population primarily comprising small side branches (reference vessel diameter <2.1 mm) and confirms the importance of observational studies to formulate new hypotheses. These studies tend to include more patients, who are usually less selected, and their findings can be better extrapolated to daily clinical practice. However, only randomised studies which prospectively evaluate a direct question can provide a definitive answer to guide our clinical decisions. It is difficult to know whether the differences between the two studies is due to poor adjustment of baseline characteristics in the Korean retrospective and observational study6 or to a more restrictive selection of patients in the prospective and randomised Spanish study8.
Finally, in a third study, Ohya et al10 analysed the impact of predilatation before MV stent implantation using the kissing balloon technique (preKBT). These authors evaluated 204 consecutive non-left main true bifurcation lesions (182 patients) in which provisional stenting was performed with preKBT (n=144) or sequential predilatation (n=60). They concluded that preKBT could safely prevent SB compromise following MV stenting. Additionally, preKBT improved the rate of in-stent restenosis, target lesion revascularisation and major adverse cardiac events at six to eight months of follow-up compared with sequential balloon predilatation in non-left main true bifurcation lesions treated with provisional stenting. However, the study has several limitations. It was a non-randomised, retrospective study performed at a single centre with important differences in baseline conditions, which could have affected the procedural results.
Conclusions
Predilatation of the SB before MV stenting has several possible advantages and disadvantages. Because there are no firm data available to elucidate the clinical benefit of this strategy to date, predilatation of the SB should be left to the operator’s discretion. Considering that the main purpose of SB predilatation is to prevent or overcome SB compromise after MV stenting during the provisional approach, SB predilatation could be considered when SB compromise after MV stenting is highly anticipated, such as in long ostial SB lesions and calcification.
Conflict of interest statement
H-C. Gwon has received research funds from Abbott Korea, Medtronic Korea, Boston Scientific Korea, and Biotronik Korea. M. Pan has received minor lecture fees from Abbott.

