Abstract
Background: Side branch (SB) dilation with an ultra-short balloon after main vessel (MV) stenting may minimise stent failure in coronary bifurcation lesions.
Aims: We sought to investigate the feasibility and efficacy of the Glider balloon (GB), a side branch (SB)-dedicated balloon 4 mm in length, in coronary bifurcation stenting.
Methods: In bench testing, stent configuration was examined with micro-focus computed tomography after crossover stenting followed by GB dilation or kissing balloon inflation (KBI). In the clinical study we performed GB dilatation after MV stenting for 207 lesions in 194 patients. Failure of the GB dilation and additional procedures due to inducible stent failure were investigated as well as adverse cardiac events at 1-year follow-up.
Results: In bench testing GB dilation maintained cross-sectional stent area without significant deformation and presented effective jailed strut removal in a high-angled bifurcation model. In the clinical study the cohort included left main, true bifurcation lesion, and two-stent treatment in 42.0%, 45.9%, and 14.0%, respectively. The proximal optimisation technique (POT) or POT-like inflation was performed in 82.1%. GB crossing failure, SB stenting due to dissection, and stent deformation requiring correction by KBI or MV dilation occurred in 8.7%, 1.4%, and 5.8%, respectively. Finally, simple GB dilation without KBI was completed in 91.8% for SB dilation. At one-year follow-up, target lesion revascularisation, cardiac death, myocardial infarction, and stent thrombosis were found in 7.2%, 2.1%, 2.1%, and 1.0%, respectively.
Conclusions: Simple GB dilation after adequate expansion of the proximal MV stent provided acceptable acute and long-term results as an alternative to KBI.
Introduction
Provisional stenting in coronary bifurcation lesions is universally recommended to reduce elective two-stent techniques which increase adverse events due to larger metal overlap or stent deformation induced by this complex procedure1. The proximal optimisation technique (POT) with a short balloon dilation only in the proximal main vessel (MV) stent is also strongly recommended, because it provides a more symmetric stent expansion with less malapposition1,2,3. Kissing balloon inflation (KBI) with simultaneous inflation of the MV and SB balloons is a conventional method for SB dilation; however, routine performance of KBI in clinical studies has not been shown to be beneficial4 and is associated with adverse results5,6. KBI with two balloons that minimally overlap in the proximal MV and re-POT after KBI are recommended to reduce oval dilation, overdilation in the proximal stent, and stent malapposition induced by the KBI1,3,7,8. The re-POT sequence, which is the subsequent performance of POT, simple SB dilation, and re-POT, is also recommended as a treatment which may be considered1. This is a superior procedure in terms of global strut malapposition, stent obstruction at the SB ostium, and symmetric stent expansion compared to conventional KBI9,10.
The Glider™ PTCA balloon catheter (Teleflex Medical, Wayne, PA, USA) is a unique SB-dedicated balloon with an ultra-short length (4 mm), obliquely skived tip, and torqueable shaft11,12 (Figure 1). Combining POT and SB dilation with the Glider balloon (GB) possibly provides SB ostial expansion without damaging the distal SB and minimises MV stent deformation. We sought to examine the feasibility of the GB for SB dilation as an alternative to KBI in a coronary bifurcation model and to investigate the efficacy of the GB in a single-centre observational study.
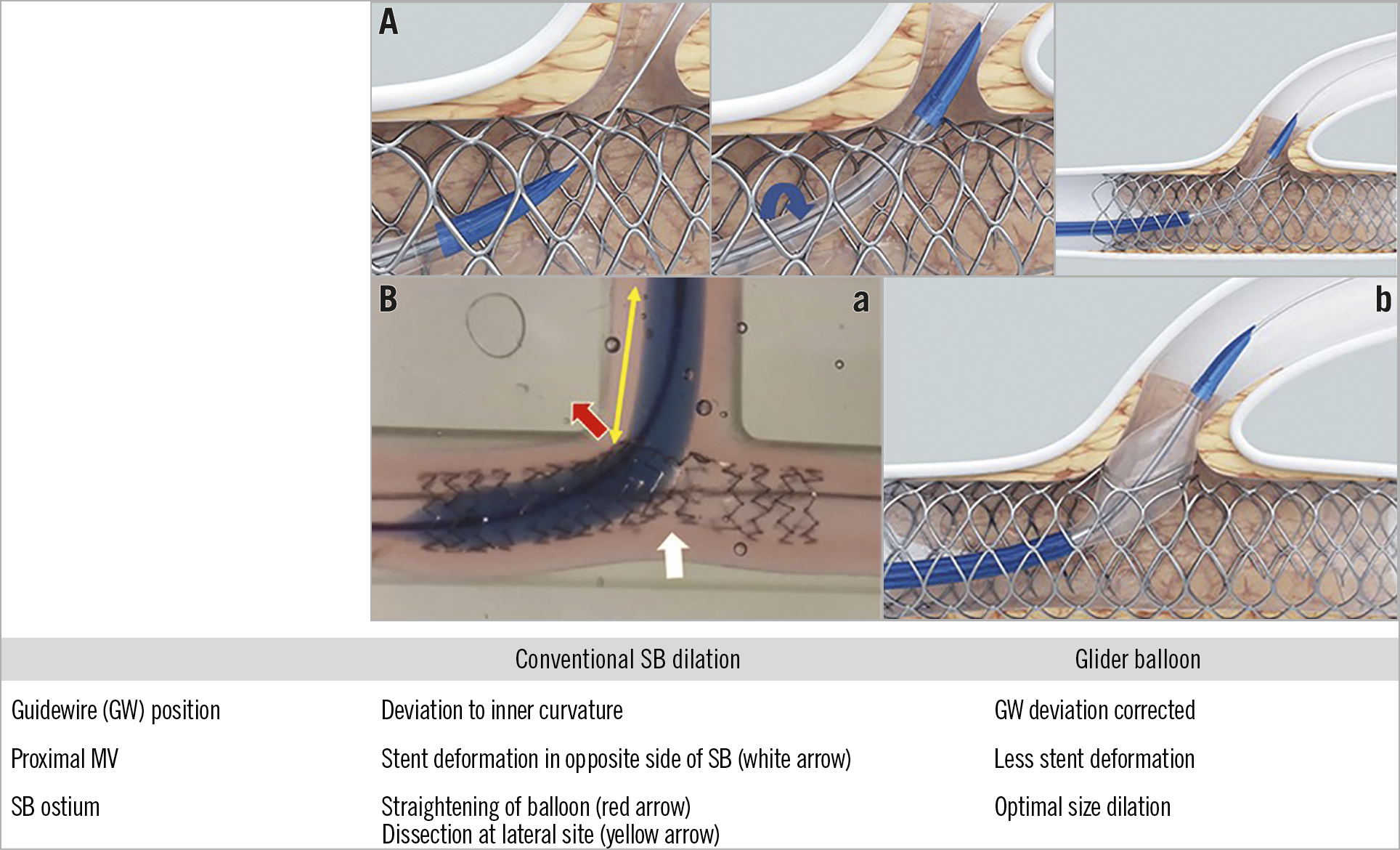
Figure 1. Scheme of SB dilation. A) Scheme showing how to deal with the initial stack of the Glider balloon (GB). When the GB tip is stacked at the SB jailed strut (left), the catheter is pulled back proximally and rotated to change the direction of the obliquely skived tip (middle). Finally, the catheter is advanced into the SB without any significant resistance (right). Courtesy of Teleflex Medical Incorporated. B) Comparison between conventional SB dilation and GB dilation. GB dilation can provide more optimal SB dilation with less guidewire (GW) deviation and stent deformation.
Methods
BENCH TESTING
Two different coronary bifurcation models consisting of 3.5 mm and 3.0 mm silicone tubes with bifurcation angles of 45° and 80° were prepared (Figure 2A). A couple of three different kinds of 3.5/18 mm stent (Supplementary Appendix 1) were implanted at 12 atm in each model. The SBs were dilated with a 3.0/4 mm GB in the SB ostium at 10 atm in one stent and with KBI using 3.5 mm and 3.0 mm non-compliant balloons at 10 atm, the proximal sites of which were minimally overlapped, in the other stent (Figure 2A). The stent was examined with micro-focus computed tomography (CT) (TDM1300-IS; Yamato Scientific, Tokyo, Japan) (Figure 2B). The cross-sectional areas at the second struts neighbouring both edges and at the most dilated site in the proximal MV were measured (Supplementary Figure 1A(1)). The jailed area was defined as the area of remaining overhanging struts at the SB ostium after the SB dilation procedure (Supplementary Figure 1A(2)).
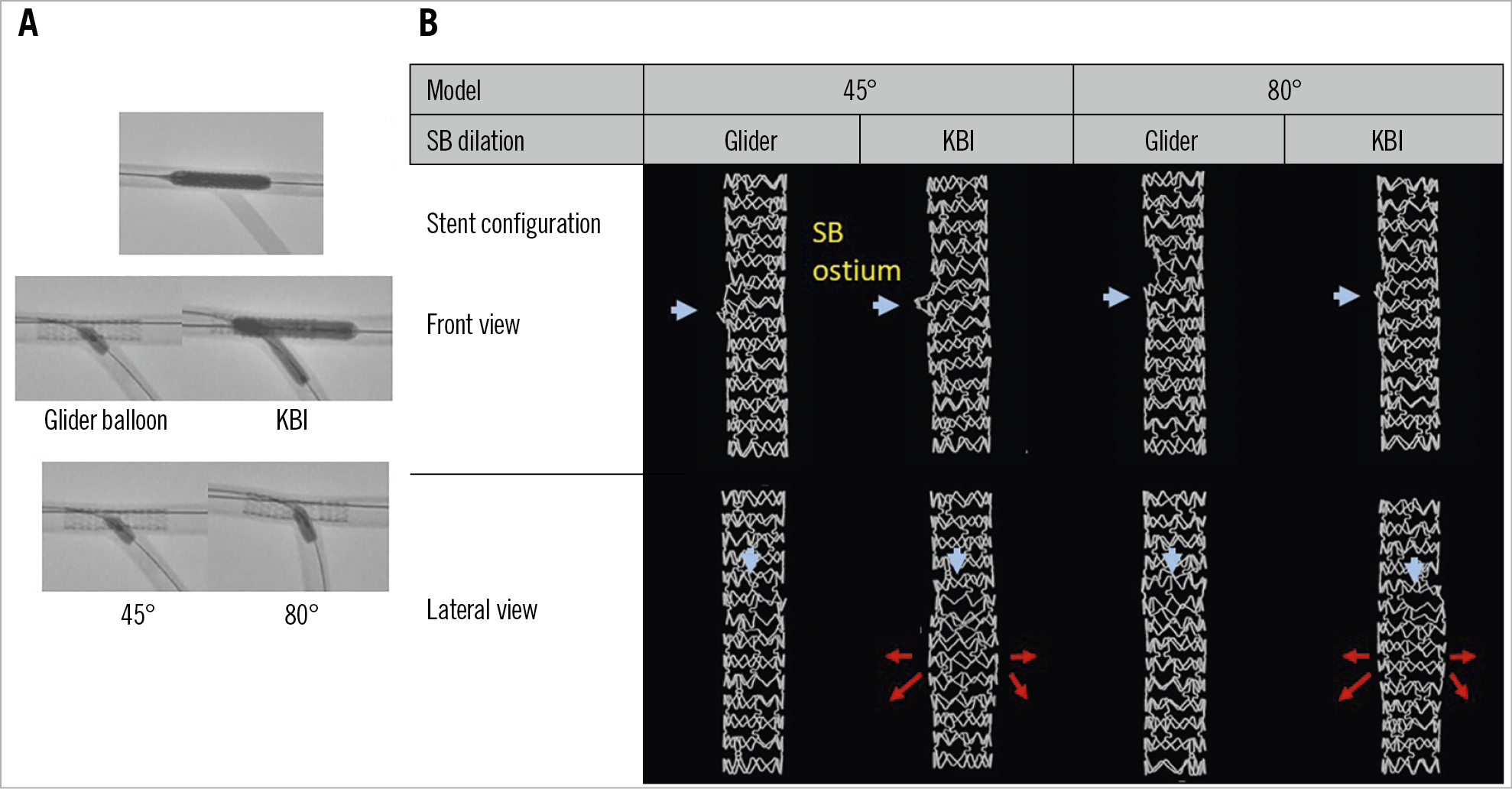
Figure 2. Bench testing comparison of side branch dilation with the GB and KBI. A) Procedure: after crossover stenting in the MV (upper panel), SB dilation with the GB or KBI was performed (middle panel) in the silicone models with bifurcation angles of 45° and 80° (lower panel). B) Representative stent configuration of each bench test (XIENCE PRIME®; Abbott Vascular, Santa Clara, CA, USA). Upper and lower panels show front and lateral views, respectively. Blue arrows indicate the SB ostium. The KBI induced oval-shaped dilation at the balloon overlapping site (red arrows) in both the 45° and 80° models.
CLINICAL STUDY
STUDY DESIGN
This clinical study is a single-centre observational study that enrolled a total of 194 patients with 207 consecutive coronary bifurcation lesions who underwent drug-eluting stent implantation and GB treatment in the National Hospital Organization Kyushu Medical Center between February 2014 and April 2018. The inclusion criteria are listed in Supplementary Appendix 2. The intervention strategy and stent type were selected at the operator’s discretion. The local Ethics Committee of our institution approved the study protocol and all patients provided written informed consent.
PERCUTANEOUS CORONARY INTERVENTION
All coronary interventions were performed with a 6 to 8 Fr guiding catheter under intravascular ultrasound (IVUS) guidance (OptiCross™ Polaris; Boston Scientific, Marlborough, MA, USA), optical coherence tomography (OCT) (Dragonfly™, ILUMIEN™, OPTIS™; Abbott Vascular, Santa Clara, CA, USA), or optical frequency domain imaging (OFDI) (FastView®, Lunawave®; Terumo, Tokyo, Japan). In the crossover stenting, MV stent size was selected according to the distal MV reference in the imaging observation, and POT with a short non-compliant balloon larger than the stent size was encouraged before SB dilation in cases where the difference between the proximal and distal MV references was >0.20 mm. In cases which did not satisfy this criterion and coinciding with inadequate proximal stent expansion, a stent delivery balloon after semi-retrieval, or a predilation balloon which was the same as or downsized by one quarter from the size of the stent was inflated with high pressure (16-26 atm) at the appropriate position of the POT balloon (POT-like inflation). After confirmation by imaging observation of the SB guidewire recrossing in the optimal distal cell of the overhanging struts at the SB ostium, a GB was advanced to the SB and dilated 2 to 4 times with its marker at the SB ostium not touching the GB proximal edge to the MV stent at the opposite side of the SB. In case of stack of the GB at the SB ostium initially, it was pulled back into a larger proximal site and rotated to change the direction of the obliquely skived tip before passing through the obstacle struts. In case of failure of GB advancement to the SB, another attempt was made after dilation with a 1.25 to 2.0 mm semi-compliant balloon. In the elective two-stenting procedures, GB dilation was performed in the stent-jailed branch ostium after the POT, similar to crossover stenting. Finally, imaging observation was performed. Re-POT or MV stent dilation with a balloon of the same size as the stent was encouraged in case of detection of significant stent malapposition or underexpansion, and final KBI was encouraged in case of significant carina shift. All patients received dual antiplatelet therapy with 81 to 200 mg aspirin daily and 75 mg clopidogrel or 3.75 mg prasugrel daily, which was continued for ≥6 months.
ANGIOGRAPHIC AND CLINICAL FOLLOW-UP
Acute procedural failure was defined as follows: 1) GB crossing failure, 2) SB dissection induced by the GB dilation which required SB stenting, and 3) stent deformation induced by the GB dilation which required correction with the final KBI or MV dilation. Follow-up angiography was performed at 8 to 12 months. Cardiac death, myocardial infarction, stent thrombosis, target lesion revascularisation, and the composite of these endpoints defined as major adverse cardiac events (MACE) were surveyed at one-year follow-up. The definitions of these endpoints are described in Supplementary Appendix 3.
ANGIOGRAPHY AND IMAGING ANALYSIS
Serial angiographies at the PCI and follow-up period were assessed quantitatively. In the imaging analysis, stent malapposition, deformation, and underexpansion were detected in each component of the bifurcation - proximal MV, bifurcation site, distal MV, and SB. Details of these analyses are shown in Supplementary Appendix 4.
STUDY ENDPOINTS
The primary endpoint is failure of the GB dilation including crossing failure, SB stenting due to dissection, and additional procedure due to inducible stent failure. Secondary endpoints are target lesion revascularisation and MACE at one-year follow-up of the GB treatment.
STATISTICAL ANALYSIS
Data are presented as numbers and percentages for categorical variables and mean±SD for continuous variables. Continuous variables were compared between the groups using an unpaired Student’s t-test, whereas categorical variables were compared using a chi-square test. All p-values were two-sided and considered statistically significant at levels <0.05. All statistical analyses were performed with EZR software (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a modified version of R Commander (R Foundation for Statistical Computing, Vienna, Austria).
Results
BENCH TESTING
GB dilation in the SB ostium did not show any increase of MV stent area, while KBI induced large stent expansion at the balloon overlapping site, the so-called bottleneck phenomenon (Figure 2, Supplementary Figure 1B(1), Supplementary Figure 1B(2), Moving image 1, Moving image 2). GB dilation showed a comparable remaining jailed area in the 45° model and less in the 80° model compared to KBI (Supplementary Figure 1B(3)). Stent deformation at the opposite side of the SB after GB dilation was not present in any of the three stent platforms.
CLINICAL STUDY
PATIENT AND LESION BACKGROUND (Table 1, Supplementary Table 1)
The majority of the patients were male; hypertension and dyslipidaemia were noted in approximately 80% of the treated patients. Of the enrolled patients, 22.3% had acute coronary syndrome. The treated lesions were in 87 left main arteries (LM; 42.0%), 83 left anterior descending arteries (LAD; 40.0%), 18 left circumflex arteries (LCX; 8.7%), and 19 right coronary arteries (RCA; 9.2%).
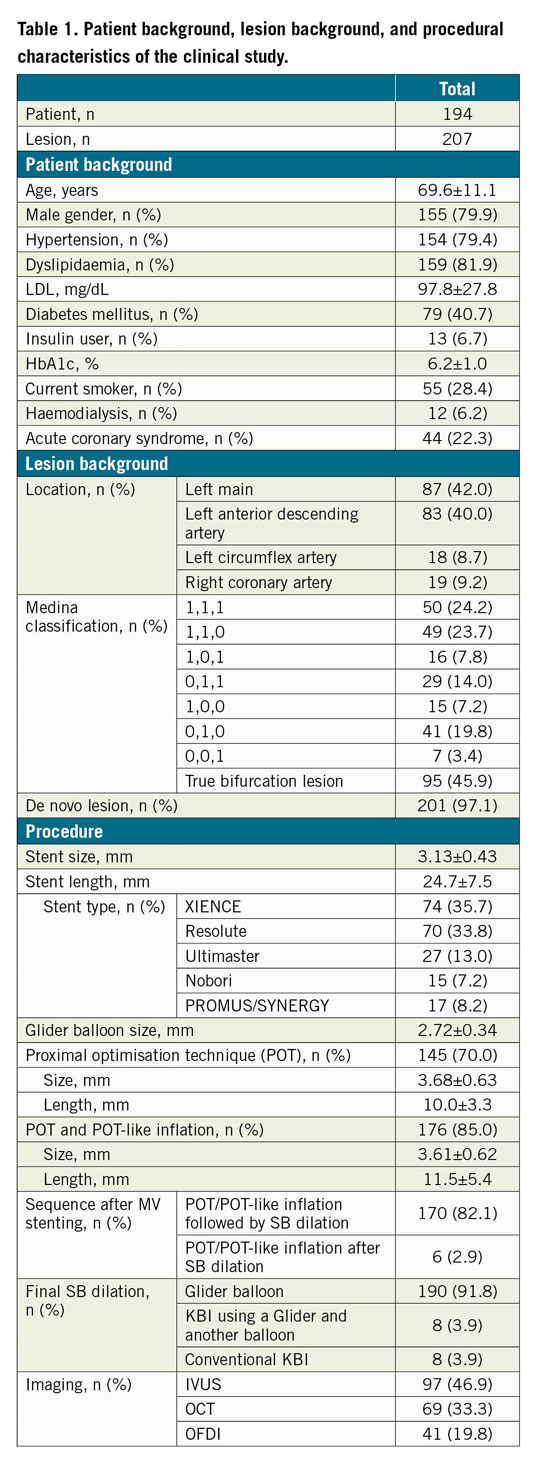
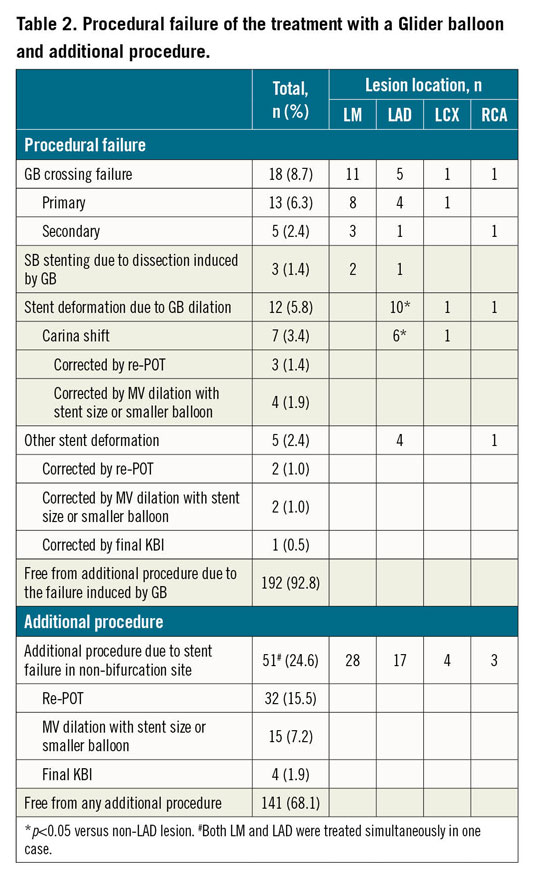
PROCEDURE AND PROCEDURAL FAILURE OF THE GLIDER BALLOON
A total of 178 and 29 lesions were treated with crossover stenting (Figure 3) and two-stenting, respectively. Two-stenting cases included more true bifurcation lesions with severe SB stenosis, more final KBI (Supplementary Table 1), and less SB stenosis at post-PCI angiography (Supplementary Table 2). The lesions were treated with the relatively large size GB (2.72±0.34 mm). POT/POT-like inflation was performed before GB dilation in 82.1%, in which the balloon size was also large enough (3.61±0.62 mm) compared to the stent size (3.13±0.43 mm) (Table 1).
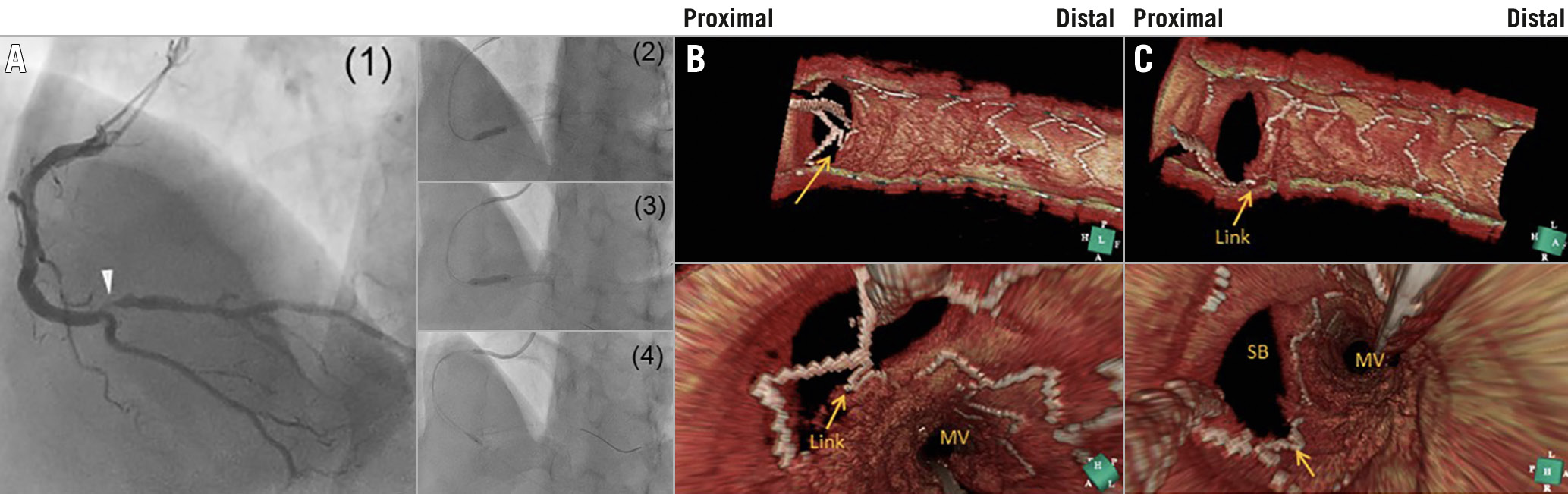
Figure 3. A representative effective case of GB dilation after crossover stenting. A) Coronary intervention. (1) Baseline coronary angiography showed a 0,1,0 bifurcation lesion with right bifurcation angle in the distal RCA. (2) A 3.25/15 mm XIENCE Xpedition® stent (Abbott Vascular) was deployed at 12 atm. (3) The stent delivery balloon was inflated at 16 atm again after some retrieval of the balloon proximally to appose the stent completely. (4) A 2.5/4 mm GB was inflated at the SB ostium. B) Three-dimensional OCT images after guidewire recrossing the SB (upper, cut-plane view; lower, fly-through view). The guidewire was recrossed in the distal cell; however, a link connection was located at the centre of the carinal site (arrows). C) Three-dimensional OCT images after the GB dilation. The jailed strut and link connection were clearly removed from the SB ostium (arrows).
Primary crossing failure of the GB was found in 13 lesions (6.3%) including five two-stenting cases, and secondary failure after dilation with a small balloon was noted in only five lesions (2.4%). GB crossing failure occurred more in the LM and in two-stenting (Table 2, Supplementary Table 3). SB stenting due to dissection was performed in only three lesions (1.4%) (Table 2). One case of spiral dissection due to slippage of the GB into the distal SB occurred because the GB was not positioned precisely in the SB ostium (Supplementary Figure 2). Imaging immediately after GB dilation showed a similar incidence of stent malapposition around the bifurcation as in the proximal MV (14.0% vs 12.6%) (Supplementary Table 2), and stent deformation around the bifurcation was found in only 4.8% (Supplementary Table 2). Serious carina shift with luminal narrowing in the distal MV was induced in 7 lesions (3.4%), which occurred most often in the LAD (6/83 cases, 7.2% vs non-LAD lesion 1/124 cases, 0.8%, p=0.02) (Table 2, Supplementary Figure 3). All of these failure lesions were corrected by MV dilation or re-POT without final KBI. Stent deformation induced by GB dilation was detected in 5 cases (2.4%), which required final KBI in only one case. Thus, 192 lesions (92.8%) were free from additional procedure for correction of the failure induced by the GB dilation. Since re-POT and MV dilation were subsequently performed for correction of the stent failure in a non-bifurcation site detected by the imaging in 32 (15.5%) and 15 (7.2%) lesions, respectively, the procedure was completed by GB dilation without any additional procedures in 141 lesions (68.1%) (Table 2).
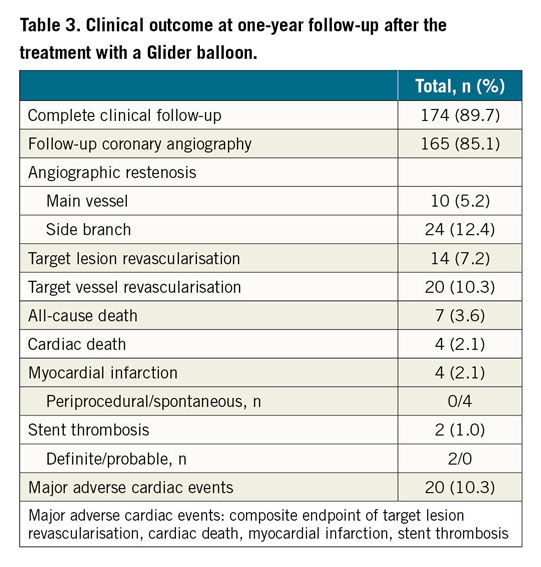
CLINICAL OUTCOME AT ONE-YEAR FOLLOW-UP
One-year clinical follow-up was completed in 174 patients (89.7%), and follow-up angiography was performed in 165 patients (85.1%). MV and SB angiographic restenosis was found in 10 (5.2%) and 24 lesions (12.4%), respectively. Revascularisation of the target lesion and vessel occurred in 14 (7.2%) and 20 patients (10.3%), respectively. Four cardiac and three non-cardiac deaths were documented at the follow-up (Supplementary Appendix 5). Myocardial infarction and stent thrombosis occurred with acceptably low frequency (2.1% and 1.0%, respectively) (Table 3, Supplementary Table 4).
Discussion
BENCH TESTING
Since SB dilation with a regular-length balloon involves the risk of carina shift and stent malapposition in the opposite side of the SB, final KBI is generally regarded as a first-line standard technique for SB dilation1, and re-POT is recommended for their correction in the re-POT sequence1,2,9,10. In the present bench testing, SB dilation with a 4 mm GB precisely positioned at the SB ostium did not present either of these findings, because its ultra-short length provided the following benefits: GB location with no contact of the stent struts at the opposite side of the SB, less stent stretch due to straightening during the balloon inflation and dilation in the limited area of the SB (Figure 1B). More effective reduction of the jailed area was also present in the GB dilation in high-angled bifurcations, while the regular-length balloon inflation induced restriction of the SB ostial dilation13. Balloon overlapping in the KBI induced oval-shaped dilation in the proximal MV, which was likely to result in stent overdilation, while SB dilation with the GB did not induce significant stent deformation (Figure 2B, Supplementary Figure 1B, Moving image 1, Moving image 2), indicating no need for routine performance of re-POT after GB dilation.
CLINICAL STUDY
TECHNICAL SUCCESS OF GB CROSSING
Crossing failure in the present study (primary 6.3%, secondary 2.4%) was acceptably low, which is comparable to a previous multicentre study that showed a rate of 8% for 96 patients12. The GB is a dedicated SB balloon that has special characteristics: ultra-short length, obliquely skived tip and torqueable strong shaft to escape from the obstacle, and long wire port to provide strong pushability11,12. A high success rate of GB crossing into the SB (80–83%) was reported even after failure of a conventional balloon11,12 at higher-angled bifurcations11. In the present study, more GB crossing failure was observed in high-angled LM and two-stenting cases. Once the GB could be advanced in the high-angled bifurcation, more effective removal of the jailed struts was achieved compared to conventional KBI in the bench testing (Supplementary Figure 1B(3)).
CARINA SHIFT
Significant carina shift with luminal narrowing in the distal MV was observed more frequently in the LAD-diagonal bifurcation, which was likely to have rich plaque burden at the opposite side of the SB in the lower-angled bifurcation. All cases were corrected by MV dilation or re-POT, not by final KBI. In such cases, adequate lesion preparation before MV stenting is effective to prevent luminal narrowing. Final KBI using the GB is another option to avoid carina shift, which is available in ≥7 Fr systems. Most of the POT+GB sequence requires only two balloons, which leads to cost savings.
SB DISSECTION
SB dissection is a concern in SB dilation with the ultra-short GB, which is likely to slip distally. One case of spiral dissection from the LCX ostium to its distal part occurred, because the GB was not positioned precisely at the LCX ostium (Supplementary Figure 2). From this case on, we confirmed the position of the GB marker at the SB ostium carefully and did not experience any spiral dissection. Since the ultra-short GB minimised vascular injury, SB stenting was performed in only two cases except for the case with spiral dissection.
ADDITIONAL PROCEDURES
Less requirement of additional procedures after GB dilation is another merit. Simple SB dilation with a regular-length balloon was likely to cause more stent malapposition at the opposite side of the SB and significant carina shift8,13, which required correction by re-POT10 or final KBI; however, these were unlikely to occur in the GB dilation in the present study (5.8%) (Table 2). Stent deformation was likely to occur due to deep engagement of the guiding catheter, retrieval of the jailed wire, insertion of the rewrapped balloons, and the additional procedure itself14. In the present study, the sequence of POT/POT-like inflation followed by GB dilation was a simple procedure with fewer or no complications involving problems with the rewrapped balloon, balloon twisting, and guidewire wrapping, which may occur during final KBI or re-POT. It also provides uniform and predictable lesion dilation regardless of the operator’s experience of complex bifurcation stenting.
CLINICAL OUTCOME AT ONE-YEAR FOLLOW-UP
Clinical follow-up and angiography were completed adequately in a large percentage of cases (>85%). Target lesion revascularisation occurrence was acceptably low at 7.2% even after frequent performance of follow-up angiography, which is comparable to the KBI-treated group in other studies (1.3-17.9%)4,5,6,15,16,17,18. The frequency of MACE was 10.3%, which was also comparable to previous reports (2.1-23.2%)4,5,6,15,16,17,18. These findings indicate the efficacy of the GB treatment with a simple procedure.
Study limitations
There was a lack of experiments for comparisons in the bench testing. The difference between a silicone tube and a human coronary vessel may exaggerate some experimental results. The clinical study was a single-arm observational study of GB dilation in a single centre. A comparison between other SB dilation procedures, such as KBI or re-POT sequence, was not available. Since the study was not a randomised trial, selection of the lesion and the interventional treatment included some bias.
Conclusions
Simple GB dilation after MV stenting provided effective removal of jailed struts at the SB ostium without any significant MV stent deformation in the bench testing. A single-centre observational clinical study also showed that simple GB dilation after adequate expansion of the proximal MV stent provided acceptable acute and long-term results without routine performance of KBI or re-POT.
|
Impact on daily practice In coronary bifurcation stenting, POT followed by 4 mm GB dilation in the SB ostium is a simple procedure without routine performance of re-POT or KBI. It can provide uniform and predictable stent expansion and effective removal of the jailed struts at the SB ostium without an increase in SB stenting. One-year clinical outcome after GB treatment is also comparable to KBI treatment in previous studies. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Three-dimensional micro-focus CT image of the stent (3.5/18 mm XIENCE PRIME) followed by KBI using 3.0 mm and 3.5 mm non-compliant balloons.
Moving image 2. Three-dimensional micro-focus CT image of the stent (3.5/18 mm XIENCE PRIME) with a 3.0 mm GB dilation in the SB.