Abstract
As bifurcation PCI can often be resource-demanding due to the use of multiple guidewires, balloons and stents, different technical options are sometimes being explored, in different local settings, to meet the need of optimally treating a patient with a bifurcation lesion, while being confronted with limited material resources. Therefore, it seems important to keep a proper balance between what is recognised as the contemporary state of the art, and what is known to be potentially harmful and to be discouraged. Ultimately, the resource-tailored approach to bifurcation PCI may be characterised by the notion of minimum technical requirements for each step of a successful procedure. Hence, this paper describes the logical sequence of steps when performing bifurcation PCI with provisional SB stenting, starting with basic anatomy assessment and ending with the optimisation of MB stenting and the evaluation of the potential need to stent the SB, suggesting, for each step, the minimum technical requirement for a successful intervention.
Abbreviations
DK-crush: double kissing crush
IVUS: intravascular ultrasound
KBI: kissing balloon inflation
MB: main branch
NC: non-compliant
OCT: optical coherence tomography
PCI: percutaneous coronary intervention
POT: proximal optimisation technique
SB: side branch
SC: semi-compliant
TAP: T and small protrusion
Introduction
Percutaneous coronary interventions (PCI) affecting a bifurcation lesion are encountered in 15-20% of cases in daily practice1. The inherent difficulty of bifurcation PCI stems from the fact that stent implantation in the main branch (MB) may lead to acute impairment of coronary blood flow in the side branch (SB). However, the true clinical relevance of an SB is notoriously difficult to standardise. It mostly depends on an operator’s subjective judgement, taking into account individual patient factors, such as SB diameter and length, angle between the SB and MB, the amount of the myocardium subtended by the SB, myocardial viability, collateralising vessels, ischaemic symptoms, comorbidities and left ventricular function1. Apart from the acute risk of periprocedural SB occlusion, bifurcation PCI is associated with an increased risk of long-term stent-related ischaemic adverse events, including stent thrombosis2. Although the optimal technique for bifurcation PCI is still debated, an individualised approach with an initial provisional SB stenting strategy seems to be warranted in the vast majority of patients3,4.
As bifurcation PCI can often be resource-demanding due to the use of multiple guidewires, balloons and stents, it is the aim of this manual to provide step-by-step advice on how potentially to maintain a balance between the evidence-supported technical requirements of optimal bifurcation PCI and parsimonious resource allocation.
How to read this manual
As the course of an intervention is unpredictable in an individual patient, we describe, in a colour-coded algorithm (Figure 1), potential strategies to save resources for each of the procedural steps 2–6 (wiring, predilatation, MB stenting, post MB-stenting optimisation, SB stenting), implying that resource-sparing techniques may be used whenever possible, but in agreement with the existing evidence base. A green coloured spot denotes what is currently appreciated as the recommended approach in bifurcation PCI, whereas an orange spot describes what may be considered a minimum technical requirement for achieving optimal results, and a red spot stands for procedures that cannot be recommended as safe and/or leading to optimal results. The blue arrow sign emphasises key strategic considerations in bifurcation PCI decision making (Figure 1). The suggestions presented are based on the current clinical practice guidelines for bifurcation PCI that recommend main vessel stenting only, with provisional intervention in the SB, as an initial approach in most cases5. Moreover, our proposals on potential strategies to achieve optimal results with limited resources are mainly based on the European Bifurcation Club consensus documents1,6,7.
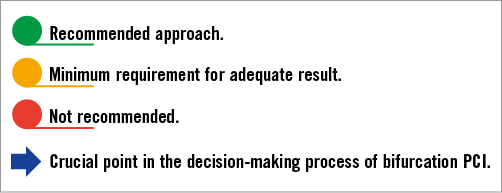
Figure 1. Description of the colour coding.
Although the step-by-step strategies portrayed here to achieve optimal results with limited resources may also foster education in bifurcation PCI, the practical decision making, concerning the safety of the technical minimum in an individual patient, may require advanced knowledge and experience in bifurcation PCI.
![]() Baseline assessment of bifurcation anatomy
Baseline assessment of bifurcation anatomy
Regardless of the stenting technique chosen, the initial step for a successful bifurcation PCI strategy begins with a good understanding of bifurcation anatomy. The main points when assessing bifurcation anatomy may be summarised as follows:
1. Assessment of the three diameters of a bifurcation.
2. Assessment of the lesion length and plaque distribution.
3. Assessment of the bifurcation angle and SB ostium.
![]() When assessing the anatomy, it is important to evaluate whether a lesion fits the concept of a true bifurcation, i.e., if there is a significant narrowing of the lumen in both the MB (proximal and/or distal) and the SB4. This is of practical importance, since intervening on true bifurcations carries an increased risk of SB compromise.
When assessing the anatomy, it is important to evaluate whether a lesion fits the concept of a true bifurcation, i.e., if there is a significant narrowing of the lumen in both the MB (proximal and/or distal) and the SB4. This is of practical importance, since intervening on true bifurcations carries an increased risk of SB compromise.
To achieve the goal of obtaining a correct assessment of the bifurcation site (SB ostium and the bifurcation angle), the operator needs to take into account the foreshortening effect of some angiographic views, by taking images from several different projections, often including non-standard views.
Provisional SB stenting strategy
The provisional single-stent strategy is the currently recommended default strategy for approaching bifurcation PCI5,6. The main postulates of the provisional single-stent strategy are optimal MB stenting and a possibility of subsequent SB stenting only in case of significant flow impairment and/or severe stenosis with haemodynamic relevance for a clinically important myocardial territory8.
![]() When performing bifurcation PCI in general, and in the provisional single-stent strategy in particular, it is imperative to keep in mind that long-term clinical outcomes are mainly dependent on the success of MB stenting. Therefore, optimisation of results in the MB should take priority over “pre-eminence” of the angiographic result in the SB.
When performing bifurcation PCI in general, and in the provisional single-stent strategy in particular, it is imperative to keep in mind that long-term clinical outcomes are mainly dependent on the success of MB stenting. Therefore, optimisation of results in the MB should take priority over “pre-eminence” of the angiographic result in the SB.
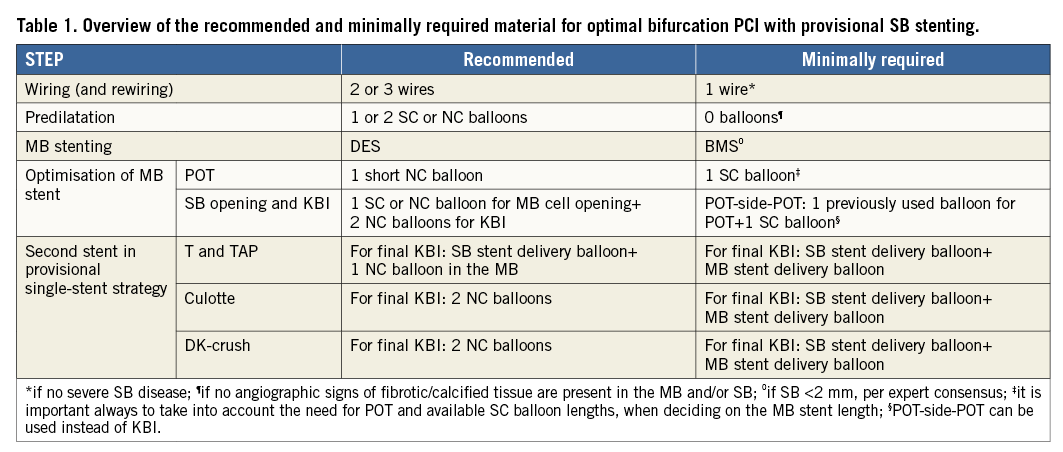
In the following text, steps 2 to 5 describe how to perform MB stenting optimally, while in step 6 we elucidate potential strategies for SB stenting, if deemed necessary (Table 1).
A 6 Fr guide catheter is generally used, although a 7 Fr guiding catheter may be preferred when complex two-stent strategies are planned.
![]() Wiring (and rewiring)
Wiring (and rewiring)
RATIONALE FOR ELECTIVE SB WIRING IN A PROVISIONAL SINGLE-STENT STRATEGY
Periprocedural occlusion of a large SB (>2.5 mm) has been a recognised contributor to impaired post-PCI prognosis, whereas the jailed wire technique has been shown to improve the rates of SB reopening in case of closure9.
The rationale for wiring the SB prior to MB stenting is mainly built upon the following observations:
1. Jailed wire may serve as a marker for rewiring of the SB through the MB stent struts.
2. SB wiring reduces the bifurcation angle, thus setting a more favourable anatomical position for rewiring and advancement of balloons and stents into the SB.
3. Jailed wire may improve SB patency after MB stenting.
4. In case of a clinical urgency and after multiple failed attempts at SB rewiring, a small balloon may be advanced over the jailed wire between the stent and the vessel wall to facilitate acute SB reopening10.
5. Jailed wire may serve as an anchor for deeper intubation of the guiding catheter, thus increasing the support in case of difficult SB balloon crossing.
![]() Elective SB wiring is recommended in all cases where the operator deems the SB clinically important, and always when treating true bifurcation lesions. When using two wires (MB and SB), the most angulated branch should be wired first to avoid wire wrap. Following MB stenting, the SB is rewired with the MB wire (wire exchange) before removing the jailed wire. An additional wire (third wire) could be used for rewiring the SB after MB stenting, if it is important that the MB wire remains in position. SB rewiring is required in case of the need for further intervention (i.e., dissection, flow impairment or severe stenosis >75%)8.
Elective SB wiring is recommended in all cases where the operator deems the SB clinically important, and always when treating true bifurcation lesions. When using two wires (MB and SB), the most angulated branch should be wired first to avoid wire wrap. Following MB stenting, the SB is rewired with the MB wire (wire exchange) before removing the jailed wire. An additional wire (third wire) could be used for rewiring the SB after MB stenting, if it is important that the MB wire remains in position. SB rewiring is required in case of the need for further intervention (i.e., dissection, flow impairment or severe stenosis >75%)8.
Polymer-coated (hydrophilic) guidewires, that are mostly used in cases of challenging SB wiring, can safely be jailed by the MB stent, and may even be more resilient to damage compared to non-polymer-coated wires11.
MINIMUM TECHNICAL REQUIREMENTS
![]() Only one wire (MB wire) may be used in cases of a favourable bifurcation angle (more obtuse angulation) and the absence of severe disease in the SB.
Only one wire (MB wire) may be used in cases of a favourable bifurcation angle (more obtuse angulation) and the absence of severe disease in the SB.
When trying to avoid the use of a third wire, it is advisable to pre-shape the distal tip of the MB wire to match the angulation of the SB and the diameter of the MB (primary and secondary curves on the MB wire, respectively), in order to re-cross the distal strut of the MB stent successfully with the MB wire. Subsequent to MB stent re-crossing with the MB wire, the jailed SB wire is retracted from the SB and outside of the MB stent, and advanced into the distal MB (wire exchange).
![]() It is not recommended to use only one guidewire in case of true bifurcations with severe SB disease or unfavourable SB angulation (difficult rewiring).
It is not recommended to use only one guidewire in case of true bifurcations with severe SB disease or unfavourable SB angulation (difficult rewiring).
![]() Predilatation
Predilatation
RATIONALE FOR MB AND SB PREDILATATION
Optimal lesion preparation in the MB, with adequate balloon predilatation, facilitates stent sizing and MB stent optimisation, and is thus key to obtaining favourable long-term outcomes.
SB ostium predilatation is controversial because of an inherent danger of creating a dissection plane at the SB ostium, which may lead to one or more of the following:
1. Unintended access to the SB through a proximal strut of the MB stent.
2. Increasing the dissection distally in the SB when rewiring.
3. Suboptimal angiographic result in the SB ostium (e.g., haziness) after MB stenting.
Hitherto only one randomised trial has compared SB predilatation vs. no SB predilatation with a provisional single-stent strategy12. This showed higher SB TIMI flow immediately after MB stenting in patients with SB predilatation, albeit with no difference in final TIMI flow in the SB and no difference in clinical outcomes.
![]() MB predilatation should routinely be considered to facilitate optimal MB stent expansion and apposition.
MB predilatation should routinely be considered to facilitate optimal MB stent expansion and apposition.
MINIMUM TECHNICAL REQUIREMENTS
![]() Direct stent implantation, without MB predilatation, may be considered in specific clinical subsets (e.g., acute coronary syndrome [ACS]), where soft lesions can be expected and/or no angiographic signs of fibrotic/calcified tissue are present. A non-compliant (NC) balloon for MB predilatation may be considered if sized to the distal MB diameter (and the same balloon can then be used for MB post-dilatation and/or final kissing balloon inflation [KBI]).
Direct stent implantation, without MB predilatation, may be considered in specific clinical subsets (e.g., acute coronary syndrome [ACS]), where soft lesions can be expected and/or no angiographic signs of fibrotic/calcified tissue are present. A non-compliant (NC) balloon for MB predilatation may be considered if sized to the distal MB diameter (and the same balloon can then be used for MB post-dilatation and/or final kissing balloon inflation [KBI]).
Routine SB predilatation is not mandated by the currently available evidence6,12.
SB predilatation could be performed:
1. If SB access is difficult.
2. In cases of severe and/or calcified SB lesions.
3. If SB flow is compromised after initial wiring.
If SB predilatation is performed, the SB ostium should be carefully assessed before MB stenting and, if needed, switching to a planned two-stent strategy may be necessary.
![]() When performing SB predilatation, it is not recommended to use the same balloon as for the predilatation of the MB, unless the distal MB and SB have comparable diameters.
When performing SB predilatation, it is not recommended to use the same balloon as for the predilatation of the MB, unless the distal MB and SB have comparable diameters.
![]() MB stenting
MB stenting
RATIONALE FOR APPROPRIATE MB STENT SIZING
Appropriate sizing of the MB stent is important for securing favourable long-term outcomes and should mainly allow:
1. Avoiding malapposition in the proximal MB.
2. Scaffolding of the SB ostium.
![]() Drug-eluting stents are recommended for bifurcation PCI.
Drug-eluting stents are recommended for bifurcation PCI.
MB stent diameter should be selected according to the reference diameter of the distal MB.
The MB stent should extend at least 8-10 mm proximal to the carina in order to prevent balloon trauma at the proximal stent edge during the performance of the proximal optimisation technique (POT).
MINIMUM TECHNICAL REQUIREMENTS
![]() The operator must be familiar with design characteristics of the off-the-shelf stent platforms, i.e., the maximum expansion capacity and the stent cell size13, in order to avoid stent distortions and fractures. Oversizing the MB stent (above the reference diameter of the distal MB) may increase the rate of SB occlusion due to carina shift and the risk of distal dissections that would necessitate implantation of further stents in the MB.
The operator must be familiar with design characteristics of the off-the-shelf stent platforms, i.e., the maximum expansion capacity and the stent cell size13, in order to avoid stent distortions and fractures. Oversizing the MB stent (above the reference diameter of the distal MB) may increase the rate of SB occlusion due to carina shift and the risk of distal dissections that would necessitate implantation of further stents in the MB.
If only bare metal stents are available, a provisional single-stent strategy should be performed with meticulous post-stenting optimisation.
![]() Two-stent techniques with bare metal stents are not recommended.
Two-stent techniques with bare metal stents are not recommended.
Closed-cell stent platforms are not recommended for bifurcation PCI with large diameter SBs.
![]() Optimisation after MB stenting
Optimisation after MB stenting
RATIONALE FOR PROXIMAL OPTIMISATION TECHNIQUE (POT)
POT is performed with the aim of achieving the following1,6,14:
1. Correction of malapposition in the proximal MB.
2. Facilitation of the SB rewiring by modifying the orientation of the SB ostium and preventing the guidewire from entering the space between the stent and the vessel wall.
3. Facilitation of SB ostium scaffolding.
4. Restoration of the circularity of the proximal vessel.
![]() POT should be performed routinely after MB stenting to correct for stent undersizing in the proximal MB.
POT should be performed routinely after MB stenting to correct for stent undersizing in the proximal MB.
A short NC balloon, 0.5-1.0 mm larger than the MB stent diameter (depending on the “step-down” diameter of the distal MB), is recommended for performing POT, by positioning the distal marker of the balloon in front of the carina and the proximal marker inside the proximal stented segment (Figure 2).
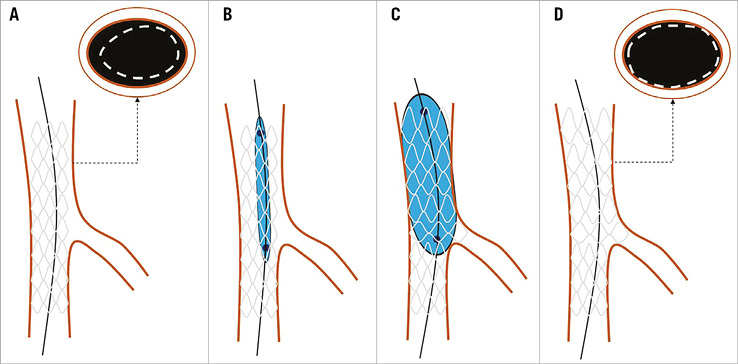
Figure 2. Proximal optimisation technique (POT). A) Stent implantation in the MB sized according to the distal reference (and therefore undersized in the proximal MB, as depicted in the cross-sectional image). B) Positioning of the short NC or SC balloon with the distal marker in front of the carina and the proximal marker inside the proximal stent edge. C) Inflation of the balloon for POT. D) Stent contour in the MB after POT. Note the correction of strut malapposition in the proximal MB segment (cross-sectional images A and D).
MINIMUM TECHNICAL REQUIREMENTS
![]() If NC balloons are unavailable, performing POT with a semi-compliant (SC) balloon may be considered, while taking into account the length of the stented proximal MB segment and available SC balloon lengths15. For efficient utilisation of existing resources, MB stent sizing should always anticipate the use of a balloon for POT. Hence, the length of the MB stent should allow for the use of the shortest available balloon on the shelf, in order to perform POT.
If NC balloons are unavailable, performing POT with a semi-compliant (SC) balloon may be considered, while taking into account the length of the stented proximal MB segment and available SC balloon lengths15. For efficient utilisation of existing resources, MB stent sizing should always anticipate the use of a balloon for POT. Hence, the length of the MB stent should allow for the use of the shortest available balloon on the shelf, in order to perform POT.
![]() It is not recommended to post-dilate the MB stent distally to the carina with the balloon sized according to the proximal MB diameter, as this inflation may aggravate carina shift, contributing to SB compromise/occlusion.
It is not recommended to post-dilate the MB stent distally to the carina with the balloon sized according to the proximal MB diameter, as this inflation may aggravate carina shift, contributing to SB compromise/occlusion.
RATIONALE FOR SB OPENING AND KISSING BALLOON INFLATION
According to randomised data16, routine KBI in provisional bifurcation PCI does not improve clinical outcome. However, in case of a severe stenosis of the SB ostium (>75%) or SB flow impairment (TIMI <3), reopening of the SB and KBI may restore normal flow to the myocardium subtended by the SB. By performing KBI, we correct strut malapposition in the proximal MB and achieve a central position of the carina8.
![]() An NC balloon is recommended for SB dilatation and should be sized according to the SB reference diameter to reduce the risk of dissection, after rewiring through the distal stent cell, as close to the carina as possible. An SC balloon may be used for SB dilatation keeping in mind the diameter achieved in the range of inflation pressures.
An NC balloon is recommended for SB dilatation and should be sized according to the SB reference diameter to reduce the risk of dissection, after rewiring through the distal stent cell, as close to the carina as possible. An SC balloon may be used for SB dilatation keeping in mind the diameter achieved in the range of inflation pressures.
KBI is recommended with two NC balloons, sized according to the SB and distal MB, with a short proximal overlap.
MINIMUM TECHNICAL REQUIREMENTS
![]() The balloon used for MB predilatation, if sized according to the distal MB diameter, may be used for KBI.
The balloon used for MB predilatation, if sized according to the distal MB diameter, may be used for KBI.
As an alternative to KBI, POT-side-POT (Figure 3) could be considered.
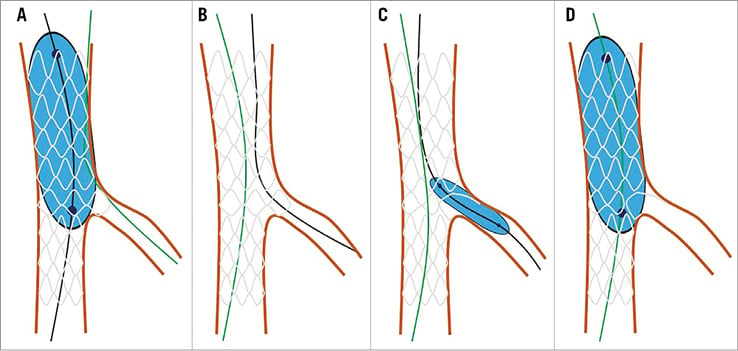
Figure 3. POT-side-POT technique for optimisation in the proximal main branch and the side branch. A) First POT after stenting of the MB, with the jailed guidewire (green) remaining in the SB. B) Exchange of guidewires. First, the guidewire from the MB (black) is placed through the distal stent strut into the SB, and, second, the initially jailed guidewire from the SB (green) is completely retracted outside the stent and, with a loop, placed into the distal MB. C) Dilatation at SB ostium with NC or SC balloon. D) Second or final POT.
The POT-side-POT technique requires performing only one balloon dilatation at a time, as explained below, in a step-by-step manner, thus minimising the material used (e.g., one instead of two inflation devices, only one additional balloon for the SB, instead of two [MB and SB] when performing KBI):
1. First POT after MB stenting with a short NC or SC balloon.
2. Wire exchange.
3. SB dilatation with an NC or SC balloon.
4. Second/final POT with the same short NC or SC balloon as the first POT.
![]() Routine performance of final KBI is not recommended in a single-stent bifurcation PCI, specifically in the absence of a true bifurcation stenosis16.
Routine performance of final KBI is not recommended in a single-stent bifurcation PCI, specifically in the absence of a true bifurcation stenosis16.
![]() Second stent in a provisional single-stent strategy
Second stent in a provisional single-stent strategy
RATIONALE FOR SB STENTING
ÆThe decision to stent the SB is of seminal importance, since an inappropriate implantation technique may jeopardise the result in the MB, which is the main determinant of favourable long-term outcomes. This decision should not be based solely on the angiographic appearance of the SB, but be made in conjunction with clinical and functional parameters, i.e., in case of clinically manifest ischaemia due to SB flow impairment or functional significance of the SB stenosis.
T-stenting and T and small protrusion (TAP)
When SB stenting is decided, the T-stenting technique is commonly recommended17. The stent is positioned at the ostium of the SB without protrusion inside the MB stent. In bifurcations with wide angles (close to 90°), T-stenting provides complete coverage of the SB ostium.
The T and small protrusion (TAP) technique is a modification of the T-stenting technique and is based on an intentional minimal protrusion of the SB stent inside the MB stent. The SB stent is deployed with a non-inflated balloon positioned in the MB across the SB take-off. After SB stent deployment, the SB stent balloon should be pulled back a few mm inside the MB and inflated to flare the protruded part of the SB stent in the MB prior to KBI. After SB stent deployment, KBI is immediately performed with the stent delivery balloon and the balloon already positioned in the MB. The advantages of the TAP technique are compatibility with 6 Fr guiding catheters, full coverage of the side branch ostium and facilitation of KBI18. This technique therefore ensures performance of KBI in all cases. The main drawback is related to the creation of a “metallic neocarina” of variable length, depending on the SB angle18.
![]() T-stenting and TAP are recommended in bifurcations with wide angles (>70°).
T-stenting and TAP are recommended in bifurcations with wide angles (>70°).
In TAP, the operator should try to limit the protrusion of the SB stent inside the MB and reduce the length of the neocarina.
When final POT is performed in TAP, precise balloon positioning is crucial to avoid crushing the metallic neocarina. Stent enhancement software may be used for precise balloon positioning.
MINIMUM TECHNICAL REQUIREMENTS
![]() The balloon used for MB predilatation and/or stent delivery balloons (both sized according to the distal reference diameter) may be used for KBI in T and TAP.
The balloon used for MB predilatation and/or stent delivery balloons (both sized according to the distal reference diameter) may be used for KBI in T and TAP.
![]() T or TAP is not recommended in narrow angle bifurcations.
T or TAP is not recommended in narrow angle bifurcations.
ÆSystematic two-stent strategies are generally performed in true bifurcation lesions with large and diffusely diseased (>5-10 mm) SB or in case of difficult SB wiring6. The most often used elective two-stent techniques are culotte and DK-crush.
Culotte and DK-crush
In narrow angle bifurcations, if SB stenting is needed, either culotte or DK-crush techniques may be utilised1. The culotte technique is better suited for bifurcations with similar diameters of the SB and the distal MB.
Culotte can be performed as an extension of a provisional single-stent strategy, after the SB is rewired, preferably re-crossing through the distal struts, and opening of the MB stent cell by balloon inflation. Then, a second stent is deployed into the SB with minimal overlap with the proximal MB stent and followed by a POT. The procedure is finished with KBI. Culotte can also be performed starting with the SB stenting (“classic” culotte), with the advantage of deploying the first stent in the most angulated vessel first1.
In DK-crush, the SB stent is placed first and then crushed with a balloon in the MB. After the SB stent is crushed and rewired, preferably by a central re-crossing, the first KBI is performed. Then, a second stent is deployed into the MB and the procedure is finished with the second KBI1.
![]() If the bifurcation angle is smaller (less than 70°), either the culotte or the DK-crush technique can be used.
If the bifurcation angle is smaller (less than 70°), either the culotte or the DK-crush technique can be used.
Final KBI is routinely recommended in both strategies.
Stenting the SB first should be considered in case of dissection or difficult SB access.
MINIMUM TECHNICAL REQUIREMENTS
![]() With culotte and DK-crush, stent delivery balloons may be used for final KBI.
With culotte and DK-crush, stent delivery balloons may be used for final KBI.
![]() Final KBI should not be skipped when performing two-stent bifurcation PCI.
Final KBI should not be skipped when performing two-stent bifurcation PCI.
The proposed algorithm for a resource-tailored bifurcation PCI is shown in Figure 4.
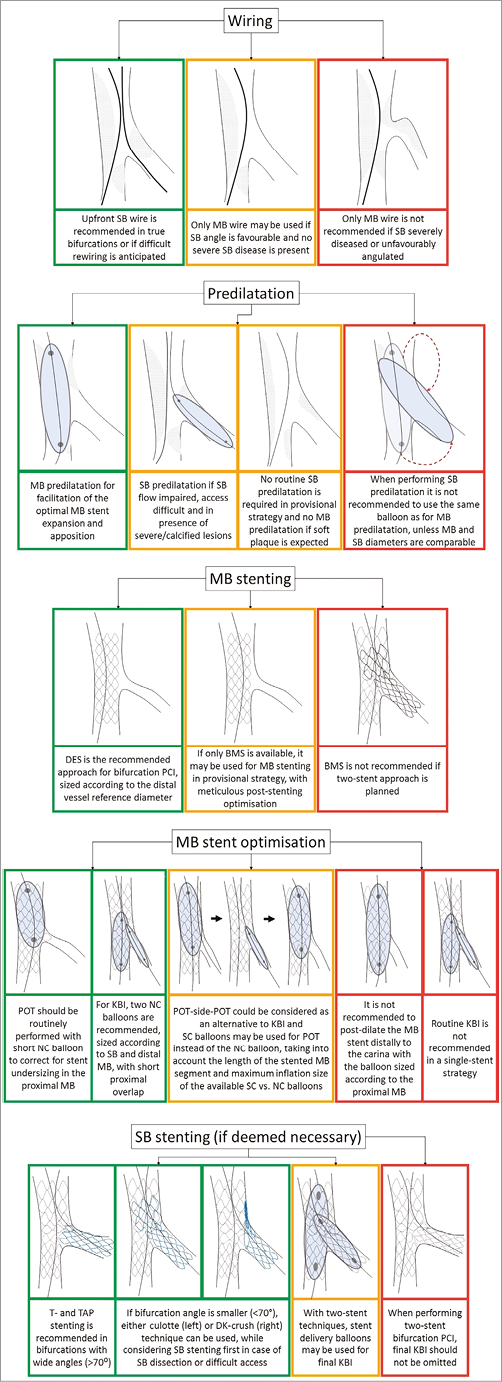
Figure 4. The proposed resource-tailored bifurcation PCI algorithm.
Intracoronary imaging in resource-tailored bifurcation PCI
Although a recent meta-analysis hinted at the favourable effects of intracoronary imaging guidance for bifurcation PCI19, its widespread use is limited by the high cost and the lack of definitive randomised evidence.
![]() In cases of increased procedural complexity (e.g., double stenting), intravascular ultrasound (IVUS) and optical coherence tomography (OCT) may offer additional information, including preprocedural and post-implantation evaluation of the vessel and stent expansion6,7. Moreover, OCT has specifically been shown to provide help in determining the exact wire position after SB rewiring, thus avoiding abluminal rewiring20.
In cases of increased procedural complexity (e.g., double stenting), intravascular ultrasound (IVUS) and optical coherence tomography (OCT) may offer additional information, including preprocedural and post-implantation evaluation of the vessel and stent expansion6,7. Moreover, OCT has specifically been shown to provide help in determining the exact wire position after SB rewiring, thus avoiding abluminal rewiring20.
![]() Intracoronary imaging can be recommended for selected complex interventions, although its routine use in bifurcation PCI is not mandated by the current evidence base6,7.
Intracoronary imaging can be recommended for selected complex interventions, although its routine use in bifurcation PCI is not mandated by the current evidence base6,7.
Conclusion
As scientific progress is not always linear, the broadening evidence base in many areas of modern medicine offers alternative strategies for ultimately achieving optimal disease management. In the field of bifurcation PCI, careful assessment of the underlying anatomy and meticulous planning of the stepwise stenting strategy may allow optimal patient treatment, even when the decision making is decisively shaped by constrained resources. It is imperative primarily to maintain procedural safety, while implementing potentially resource-saving strategies in a structured and step-by-step manner.
| Impact on daily practice Bifurcation PCI may be resource-intensive due to the use of multiple guidewires, balloons, stents and even intracoronary imaging. We propose a structured approach to resource-tailored bifurcation PCI that aims to achieve optimal results, while at the same time saving resources. Thereby, a proper balance between the contemporary state of the art, in terms of evidence-based procedural strategies, and techniques known to be potentially harmful, and therefore to be discouraged, needs to be maintained, as epitomised by the term “minimum technical requirements” to achieve optimal results. |
Conflict of interest statement
W. Wijns reports receiving grants from Terumo, grants and personal fees from MicroPort, grants and personal fees from Abbott– St. Jude, grants and personal fees from Biotronik, during the conduct of the study, and “other” from Argonauts Partners, outside the submitted work. F. Hellig reports receiving personal fees from Boston Scientific, Medtronic, Volcano, and Edwards Lifesciences, outside the submitted work. The other authors have no conflicts of interest to declare.