Abstract
Aims: The aim of this study was to determine the accuracy of the intracoronary electrocardiogram (icECG) to detect ischaemia during bifurcation lesion percutaneous coronary intervention (PCI) with fractional flow reserve (FFR) as a reference.
Methods and results: Patients with significant bifurcation lesions defined as FFR ≤0.80 were included. FFR and icECG were performed in the main vessel (MV) and side branch (SB) before and after provisional stenting. icECG was recorded with an uninsulated proximal wire end connected to a unipolar lead. The diagnostic accuracy of the icECG for the detection of ischaemia in the SB after MV stenting was determined with FFR as a reference. Overall, 37 patients were included. Seventeen bifurcations had an SB FFR ≤0.80 after MV stenting and 20 patients had an ST-segment elevation on the icECG. There was significant correlation between SB FFR and ST-segment elevation on the icECG (r=–0.533, p<0.001). The diagnostic accuracy of icECG ST-elevation to detect functionally significant SB stenosis revealed an AUC of 0.71 (95% CI: 0.64-0.80) with a sensitivity of 88% and specificity of 75% with a positive predictive value of 75% and negative predictive value of 88%. Neither SB FFR nor icECG correlated with SB percent diameter stenosis after MV stenting.
Conclusions: Intracoronary ECG has a good ability to predict functionally significant stenosis at the SB after MV stenting during bifurcation PCI. This method provides a novel strategy to assess the significance of an SB lesion without the need of a pressure wire. ClinicalTrials.gov Identifier: NCT01724957
Abbreviations
AUC: area under the curve
ECG: electrocardiogram
icECG: intracoronary electrocardiogram
FFR: fractional flow reserve
MV: main vessel
PCI: percutaneous coronary intervention
QCA: quantitative coronary angiography
SB: side branch
Introduction
Significant progress has been made in recent years in the interventional treatment of coronary bifurcation lesions1. Provisional stenting has been recommended as the default strategy by the European Bifurcation Club2. Nevertheless, we do not have a firm criterion as to which side branch (SB) should be treated after main vessel stenting (e.g., SB stenosis in patients with periprocedural symptoms) and the implication for prognosis. It is now widely accepted that measurements of fractional flow reserve (FFR) can identify haemodynamically significant lesions that require revascularisation3-12. The studies investigating FFR in coronary bifurcations have demonstrated a large discrepancy between the angiographic and functional assessments, particularly in the investigation of SB stenosis after main vessel (MV) stenting4-10,12. FFR is not always possible to measure, even in highly selected cases13. In addition to difficulties in stent crossing, a pressure wire can be damaged if it is jailed14,15. The cost of the pressure wire is an additional consideration that must be taken into account as a disadvantage for the patient. There are also methodological problems of using FFR for the assessment of acutely occurring SB ostial stenosis after MV stenting in coronary bifurcations13,17. It is possible that, despite significant FFR values (≤0.80), there is enough flow to the myocardium. The converse may also be true, that, above the cut-off of 0.80, the absolute flow may not be satisfactory, causing ischaemia. In the first case, there is an increased risk of complications because of unnecessary intervention, and in the latter there is a risk of leaving a significant stenosis untreated13. Hence, there is a niche for additional methods to assess the repercussions of coronary lesions.
The intracoronary electrocardiogram (icECG) is an established method for monitoring ischaemia during percutaneous coronary intervention (PCI)18-24. It provides an opportunity to detect ischaemia in its early stages, when changes on surface electrocardiogram or angina are not yet prominent. Since SB stenosis can occur acutely after stenting of the main vessel (MV) and consequently cause ischaemia, icECG can be recorded from the end of the guidewire during PCI. This is a similar rationale to the physiological assessment of coronary stenosis25. However, data on the accuracy of icECG during bifurcation PCI are scarce. The aim of this study was to determine the accuracy of icECG to detect ischaemia in the SB after MV stenting with FFR as a reference.
Methods
PATIENT SELECTION
Patients with stable or unstable angina were included. The inclusion criterion was angiographic bifurcation lesions in a native coronary artery with a diameter ≥2.5 mm and ≤4.5 mm and an SB diameter ≥2.0 mm. We excluded patients with ST-segment elevation myocardial infarction and those with non-cardiac comorbid conditions with a life expectancy of less than one year. In addition, patients with left main coronary artery stenosis, total occlusion, lesion of interest located at an infarct-related artery, subjects with LVEF <30%, subjects with a moderate or severe degree of valvular heart disease or primary cardiomyopathy and patients with bundle branch blocks, and atrial fibrillation/flutter with no identifiable isoelectric line were excluded. The local ethics committee approved the study.
DEFINITION OF ENDPOINTS
An ST-segment elevation >1 mm on the icECG was defined as significant ischaemia based on the correlation with clinical events observed in previous studies24. An FFR value of ≤0.80 was defined as a functionally significant lesion. Post-procedural myocardial infarction was defined according to the third universal definition26. A 12-lead ECG was obtained before and both one and 24 hours after the procedure.
PROCEDURES
PCI was performed according to the current guidelines. Provisional stenting was the default strategy in all patients. Two guidewires were inserted into the distal MB and the SB. Initial FFR was measured using the PrimeWire® or PrimeWire Prestige® (Volcano Corp., San Diego, CA, USA). Intracoronary ECG was recorded by connecting the uninsulated end of a commercial PCI wire (i.e., Runthrough® [Terumo Corp., Tokyo, Japan]; BMW Universal II [Abbott Vascular, Santa Clara, CA, USA]; or SION [Asahi Intecc, Aichi, Japan]) with alligator clips to the V-lead of the ECG recorder of the haemodynamic recording station. After MV stenting, the icECG from the MV and SB was recorded and FFR in the MV and SB was measured accordingly. After completion of the procedure, a final icECG from the distal MB (5 mm distal to the implanted stent and at the terminal part of the vessel), as well as from the SB (10 mm from the ostium) was recorded. If icECG ST-segment elevation occurred in any of the MB regions it was marked as MB elevation. The proximal end of the radiopaque part of the wire was placed 5 mm below the ostium of the SB, thus covering an area with a length of at least 35 mm, which is a significant part of the side branches. Of note, a more distal placement of the wire usually results in anchoring of the wire tip into myocardium, which makes the icECG uninterpretable. For all FFR measurements, intracoronary adenosine was given in increasing doses of 60 mcg, 120 mcg, and 240 mcg. Predilatation of the MV was mandatory. Final kissing balloon inflation (KBI) or sequential balloon inflation was performed at the discretion of the operator. It was recommended that in case of SB icECG ST-elevation a balloon dilatation of the SB be performed. Also, SB stenting was recommended in the case of flow less than TIMI 3, when the visual diameter stenosis was >70% at the SB ostium and when the patient was symptomatic (i.e., chest pain) despite a balloon dilatation. If none of the abovementioned criteria was present, the FFR value was used for decision making. All lesions were stented with second-generation DES. Angiographic success was defined as end-procedural MV percent diameter stenosis (%DS) <20% and SB stenosis <70% without significant dissection and flow impairment2. Procedural success included angiographic success in the absence of in-hospital MACE (death, stroke and myocardial infarction). The procedural steps are presented in Figure 1.
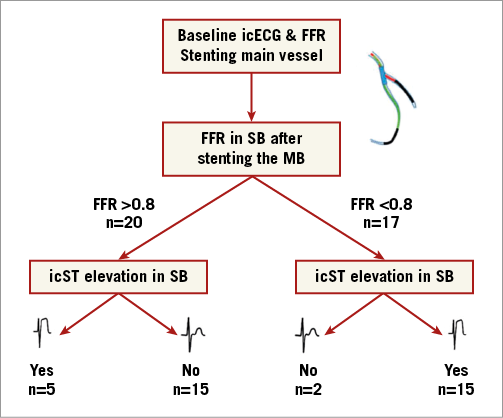
Figure 1. Schema of procedure steps.
INTRACORONARY ECG ANALYSIS
The analysis of icECG has been described previously24. Briefly, the absolute ST-segment shift in the icECG lead and surface leads I, II, and aVF was determined before PCI, at the end of the coronary balloon inflation (for SB, MB predilatation and/or post-dilatation, stent implantation) and at the end of the procedure. The recorded intracoronary and surface lead ECGs, with simultaneously recorded aortic blood pressure curves, were printed and analysed consecutively. The paper speed was 50 mm/s and ECG amplitude was calibrated at 10 mm/mV. The points at the beginning of the QRS complex, the end of the QRS complex and the end of the T-wave were connected and constituted the isoelectric line. If some hallmark points were not distinct, definition of the isoelectric line was based on two hallmark points; the ST-segment shift was calculated as the distance of the corresponding point from the isoelectric line in a perpendicular direction. The ST-segment elevation at the end of first balloon inflation was accepted as the maximum icECG ST-segment elevation in the main and side branches, recorded 20 to 30 seconds after the beginning of vessel occlusion.
ANGIOGRAPHIC ANALYSIS
Dedicated bifurcation quantitative coronary angiography (QCA) analysis was performed according to the recommendations of the consensus on QCA methods for bifurcation lesions from the European Bifurcation Club27. True bifurcation lesions were defined as lesions with a visual percent diameter stenosis (%DS) >50% at the SB. The minimal luminal diameter (MLD), reference vessel diameter (RVD) and %DS were measured for every segment of the bifurcation (i.e., proximal and distal MV and SB) pre and post intervention. All analyses were performed by an independent core lab (Cardialysis BV, Rotterdam, the Netherlands) using a two-dimensional analysis (CAAS software, version 7.3; Pie Medical Imaging, Maastricht, the Netherlands).
STATISTICAL ANALYSIS
Continuous variables are presented as mean±standard deviation. Categorical variables are presented as counts and/or percentages. The difference between the groups was examined using paired or unpaired t-tests as appropriate. Otherwise, the Wilcoxon signed-rank test and Mann-Whitney U tests were used. Chi-square tests were applied for qualitative data. The area under the receiver operating characteristic curve (AUC) was used to assess the diagnostic accuracy of the test. A Spearman correlation plot was created for the comparison of simultaneous changes in icECG and FFR values. For this proof of concept study, no sample size calculation was performed.
Results
A total of 73 patients were screened; six patients were excluded, because of incomplete data recordings during initial FFR, and 30 patients were excluded because of a lack of functionally significant stenosis in the main vessel. Finally, 37 patients were included based on the presence of functionally significant lesions. Table 1 and Table 2 show the clinical and angiographic characteristics of patients with and without functionally significant lesions.
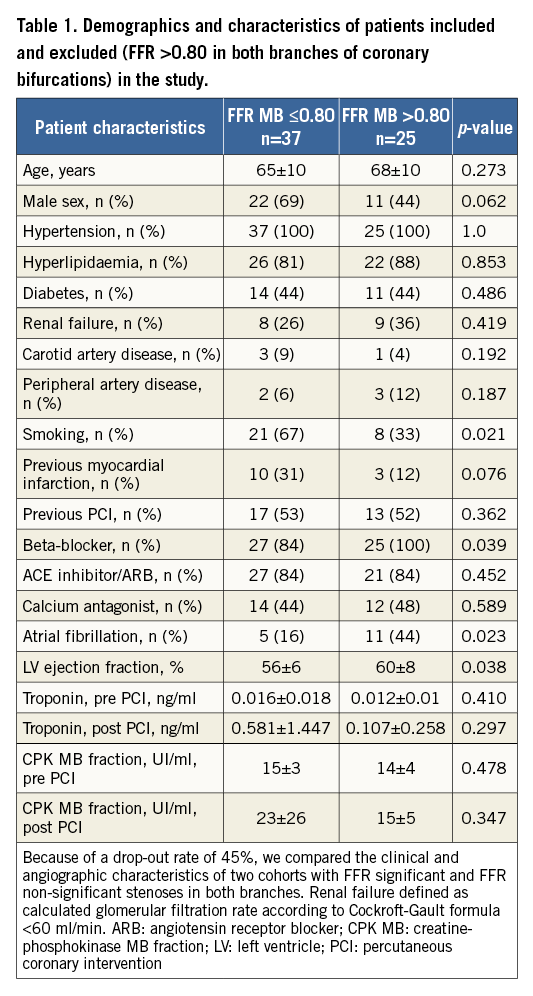
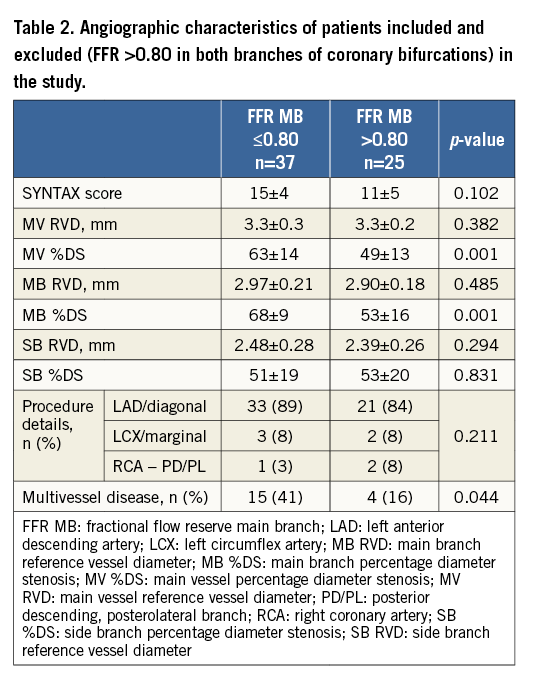
Demographic characteristics for the patients included in the final analysis are presented in Table 3, stratified according to the FFR at the SB after main vessel stenting. Table 4 shows the dedicated QCA analysis pre and post intervention. Examples of all possible combinations between FFR and icECG after stenting the MV are presented in Figure 2. Seventeen patients had an SB FFR ≤0.80 after MV stenting and 20 patients had an ST-segment elevation on icECG. All patients with an SB icECG elevation underwent SB stenting. Of the patients with an FFR ≤0.80, only two did not have an ST-segment elevation on icECG; nonetheless, these patients had an FFR >0.75 (i.e., 0.77 and 0.78). The diagnostic accuracy of icECG ST-elevation to detect functionally significant SB stenosis after stenting revealed an AUC of 0.71 (95% CI: 0.64-0.80) with a s(Figure 3).
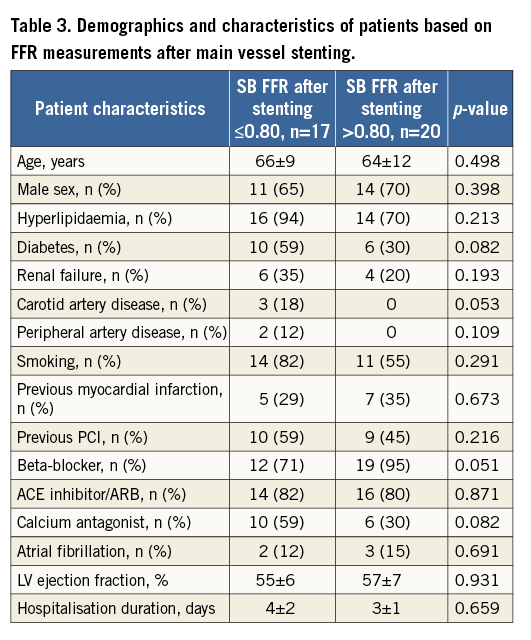
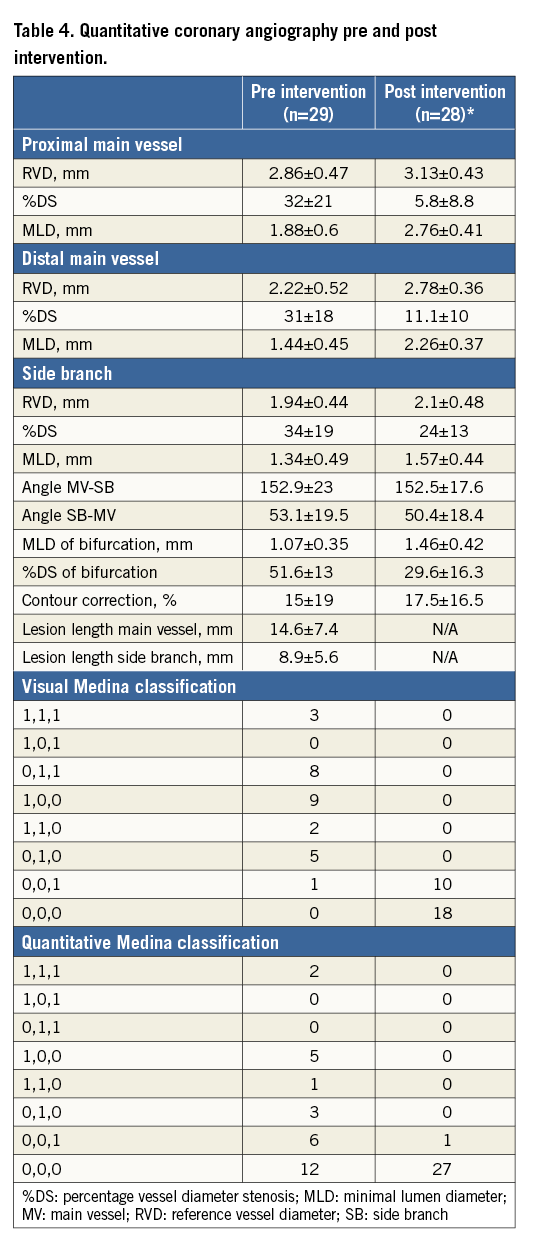
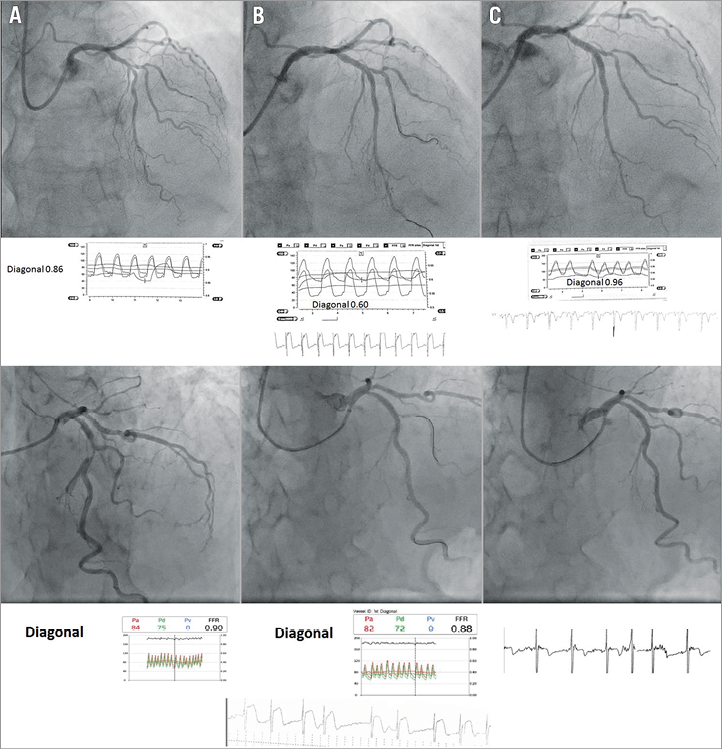
Figure 2. Some observed combinations of FFR in side branches after stenting and changes on SB icECG – both icECG and FFR positive (upper pictures) and icECG positive and FFR negative (lower pictures). A) Before PCI. B) After stent placement in the MV. C) Final result.
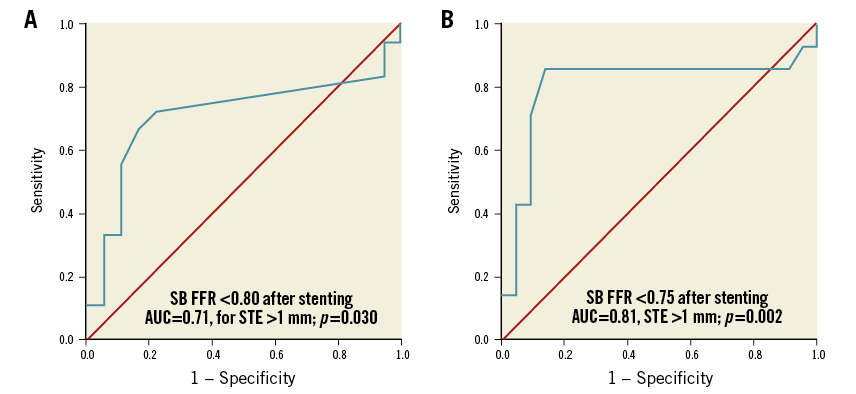
Figure 3. ROC curves for the accuracy of icECG to predict functionally significant stenosis on the basis of FFR <0.8 (A) and FFR <0.75 (B).
There was a significant correlation between absolute measures of SB FFR after stenting and ST-segment elevation in millimetres on icECG (r=–0.533, p<0.001) (Figure 4A). Similarly, there was a significant difference of median SB FFR values in groups with and without icECG ST-elevation (Figure 4B). Neither icECG ST-elevation nor FFR in the SB after MV stenting correlated significantly with %DS at the SB; however, there was significant correlation of both parameters with %DS at the SB post procedure (SB icECG ST-segment elevation: r=–0.396, p=0.025, SB FFR: r=0.369, p=0.038). Maximum SB icECG ST-segment elevation during first balloon implantation or during stent implantation correlated with both FFR and icECG ST-elevation (SB icECG ST-segment elevation: r=0.798, p<0.001, SB FFR: r=–0.455, p=0.020).
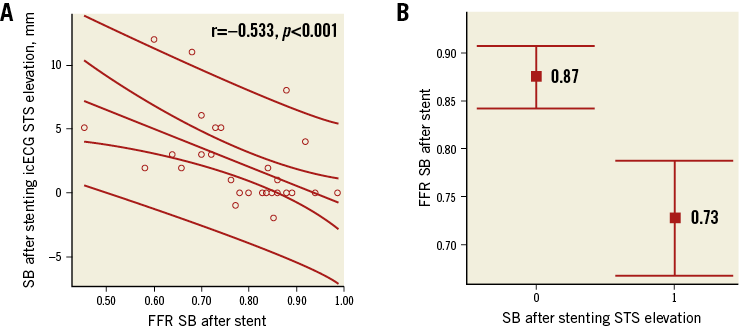
Figure 4. Fractional flow reserve and icECG findings. A) Correlation between FFR in the SB after stenting and icECG STS elevation. B) Difference in FFR values in patients with and without STS elevation on icECG. STS: ST-segment
At six-month follow-up, the death rate was 5.4% (2/37). One patient died of a brain haemorrhage two months after the procedure, and the second in a crash accident four months after the PCI. The periprocedural MI rate was 8.1% (3/37). All other patients had no major adverse events.
Discussion
The main findings of this study can be summarised as follows. 1) icECG has a good diagnostic accuracy to detect haemodynamically significant stenosis at the SB after MV stenting with FFR as reference during bifurcation PCI. 2) There was a significant correlation between FFR and icECG ST-elevation at the SB after MV stenting, which provides a link between a direct measure of ischaemia (icECG changes) and the flow-limiting capacity of stenosis (FFR).
This is the first study assessing FFR and icECG simultaneously in patients treated with PCI in bifurcation lesions. The stenosis occurring at the SB ostium after MV stenting is similar to the stenosis created in experimental animal studies25,28,29. Since ischaemia is one of the most potent vasodilators, it is not surprising that ischaemic changes on icECG correlated well with FFR values. It is also interesting that both FFR ≤0.80 and icECG ST-elevation correlated significantly with maximum ST-segment elevation on icECG during balloon inflation in ischaemia-producing lesions despite the restoration of flow to the vessel. There were five patients without haemodynamically significant FFR changes (FFR >0.80), but with ST-segment elevation on icECG, all in the distal region of the SB. It could be hypothesised that this was the result of distal embolisation to the SB during PCI.
In this study, 41% of the screened patients were excluded due to FFR >0.80 in the MV despite an angiographically significant stenosis. This calls for a reappraisal of the design of future bifurcation studies to include the use of FFR as an inclusion criterion, thereby increasing the benefit of PCI. Based on these findings, FFR assessment (at least in the MV) should be performed before initiating a bifurcation intervention. In addition, the accuracy of icECG observed in this study supports the concept of monitoring ischaemia using the same wires used in daily practice during PCI. It is an easy and inexpensive approach to detect ischaemia which could guide the strategy during bifurcation PCI. Nevertheless, these results require further validation.
Limitations
The main limitation of this study is the small number of patients included. This was due to absence of functionally significant stenosis in almost half of the patients screened. Therefore, our study is hypothesis-generating and provides a basis for future larger studies on icECG.
Conclusions
Intracoronary ECG has a good ability to predict functionally significant stenosis at the SB after MV stenting during bifurcation PCI. This method provides a novel strategy to assess the significance of an SB lesion without the need for a pressure wire. Future studies are needed to confirm this finding and to assess the impact of icECG changes on clinical outcomes.
| Impact on daily practice The use of intracoronary ECG (icECG) might be useful in assessing significant lesions during bifurcation PCI. This novel and inexpensive approach could guide bifurcation PCI without the need for a pressure wire or adenosine. |
Guest Editor
This paper was guest edited by Adrian Banning, MB, BS, FRCP, MD; Oxford Heart Centre, Oxford University Hospital, Oxford, United Kingdom.
Funding
The study was investigator initiated, funded from the local hospital (“Alexandrovska” University Hospital, Sofia, Bulgaria).
Conflict of interest statement
P. Serruys is a member of the International Advisory Board for Abbott Vascular. The other authors have no conflicts of interest to declare. The Guest Editor has no conflicts of interest to declare.