Abstract
Aims: The provisional strategy (PS) is an accepted modality of treatment in coronary bifurcation interventions, though, after main vessel (MV) stenting, the assessment of the side branch (SB) becomes more difficult. In bifurcation interventions, the major advantage of fractional flow reserve (FFR) is the avoidance of the need for SB intervention. However, SB access with a pressure wire after MV stenting may be difficult, sometimes impossible. The objective of this paper was to evaluate the feasibility and safety of physiologic assessment of SB lesions using FFR with the jailed pressure wire (JPW) in patients undergoing the PS. Although the JPW technique is theoretically possible in the PS, there is no information available on the use of this technique.
Methods and results: We retrospectively evaluated 11 patients who were treated with the JPW technique at a single centre. Procedures were successfully accomplished in all cases without complications, such as damage of the pressure sensor, failure to measure FFR value, removing the polymer coating, and entrapment or fracture of the JPW.
Conclusions: In conclusion, our limited experience suggests that the JPW technique in the PS may be a safe and technically feasible approach. This technical report details the JPW technique in patients undergoing the PS.
Introduction
The provisional strategy (PS) is an accepted modality of treatment in bifurcation interventions. However, after main vessel (MV) stenting, the assessment of side branch (SB) ostial lesions becomes more difficult because of vessel overlap, angulations, stent struts across the branch and image foreshortening. Dedicated QCA analysis systems for bifurcations have been developed to try to overcome the limitations of conventional angiography1. The fractional flow reserve (FFR) technique is emerging as a feasible option in bifurcation interventions and is being used increasingly in the PS2. The major advantage of FFR is the avoidance of the need for SB intervention. However, SB access with a pressure wire after MV stenting may be difficult, sometimes impossible. In that regard, the SB FFR evaluation usually prolongs the procedure, and the procedure may lead to complications, such as dissections and the need for additional stenting due to difficult wiring2. The objective of this paper was to evaluate the feasibility and safety of physiologic assessment of SB lesions using FFR with the jailed pressure wire (JPW) in patients undergoing the PS.
Description
The PressureWire™ Certus FFR measurement system (St. Jude Medical, Minneapolis, MN, USA) has an advanced generation technical design, featuring numerous enhancements and delivering handling performance that closely resembles standard 0.014” guidewires.
Technical specifications
Distal coating: Hydrophilic
Distal design: Polymer sleeve
Proximal coating: PTFE
Proximal connector design: Hydrophobic
Length: 175/300 cm
Diameter: 0.014”
Indications for use
FFR has been well validated in multivessel disease, left main disease, ostial lesions, serial lesions, diffuse disease, acute coronary syndromes and post-stent assessment.
Tips and tricks for use
A pressure wire is a delicate instrument. Therefore, we should advance or withdraw a pressure wire slowly. Excessive manipulation when the sensor element or tip of the pressure wire is located in a sharp bend may cause damage or tip fracture. Torquing a pressure wire against resistance may cause damage and/or fracture, which may lead to a portion of the pressure wire separating from the tip.
Intracoronary nitroglycerine is injected at a dose of 100-200 μg into the coronary artery before FFR measurements. Maximal hyperaemia is induced by an intracoronary bolus administration (80-100 μg) of adenosine3. Lesions with an FFR ≤0.80 are considered to have functionally significant SB stenosis, and SB balloon dilatation or SB stenting is allowed only for these lesions.
With the catheter outside the ostium of the vessel, equalisation of pressures of the catheter and the pressure wire is verified. The pressure wire is advanced into the SB with the pressure sensor placed at least 5 mm beyond the SB ostium. After wiring of the MV, a stent is positioned in the MV together with the pressure wire in the SB.
After MV stenting, the first FFR evaluation is done and, if the first level is higher than 0.80 in the SB, no further SB intervention is performed (Figure 1A, Figure 1B). The JPW behind the MV stent struts is carefully pulled back and FFR is measured at the MV to evaluate the influence of the proximal lesion. Finally, the pressure wire is brought back near the distal tip of the guiding catheter and equalisation of catheter and pressure wire is verified.
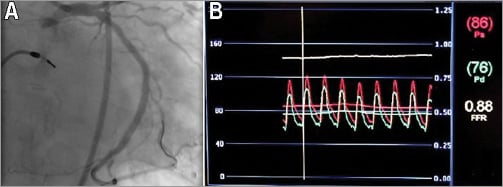
Figure 1. An example of the jailed pressure wire technique in coronary bifurcation interventions. A) Angiography showed a significant lesion at the SB ostium after MV stenting. B) FFR measurement indicated the lesion at the SB ostium was functionally insignificant.
After MV stenting, in the first measurement, if FFR is ≤0.80, the SB is rewired with a third guidewire without removing the JPW. Then, a size-matched balloon is advanced over the third wire and inflated to dilate the SB ostium. FFR is re-evaluated and, if the FFR level is higher than 0.80, the JPW is removed carefully with the third wire left in the SB. A size-matched balloon is advanced in the MV and the previously used SB balloon is loaded into the SB. Finally, kissing balloon inflation is performed at the bifurcation (Figure 2A-Figure 2G). After SB ballooning, if the FFR level is ≤0.80, SB stenting is performed with the TAP-stenting technique.
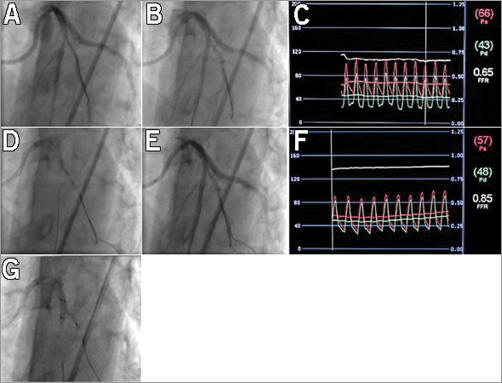
Figure 2. An example of the jailed pressure wire technique in coronary bifurcation interventions. A) Advancing the pressure wire into the SB. B) Angiography demonstrated a significant SB ostial lesion after MV stenting. C) FFR measurement (0.65) of the SB after MV stenting. D) Wiring of the SB with a third guidewire and balloon dilatation over the same guidewire while pressure wire is kept in the jailed position. E) Angiography after balloon dilatation. F) FFR measurement of the SB after balloon dilatation. G) Final kissing balloon.
Clinical experience
We retrospectively evaluated 11 patients who were treated with the JPW technique in the PS from October 1, 2012, to January 22, 2013, at a single centre. In this period, a total of 34 patients underwent stenting for coronary bifurcation lesions. All patients had a bifurcation lesion greater than 50% as defined by the Medina classification system4. Those candidates with an SB diameter of less than 2 mm, a >5 mm lesion length of the SB ostium by visual estimation, and a TIMI flow grade ≤2 in the SB flow after MV stenting, a significant distal lesion within the SB (>50%), a significant lesion within the MV proximal to the stented segment, in-stent restenosis and a contraindication to adenosine were not considered for the PS with this approach. Because of the influence of a significant lesion within the MV proximal to the SB, we did not measure the FFR value in the SB before treating the MV.
The mean age was 66.9±11.5 years. Procedural success was 100%. The main clinical, angiographic and procedural characteristics of the treated patients are reported in Table 1 and Table 2. Most lesions were located in the LAD-diagonal bifurcation (73%). Only one patient had a distal bifurcation angle greater than 70°. Before the intervention, mean percent stenosis, reference vessel diameter, and lesion length of the SB were 40.7±22.6%, 2.24±0.20 mm, and 2.95±0.74 mm, respectively. After MV stenting, the percent stenosis of the SB lesion was increased from 40.7±22.6% to 60.18±26.7% and six SB lesions were angiographically significant (>70%). However, only four of them had FFR ≤0.80, while the others had FFR >0.80.
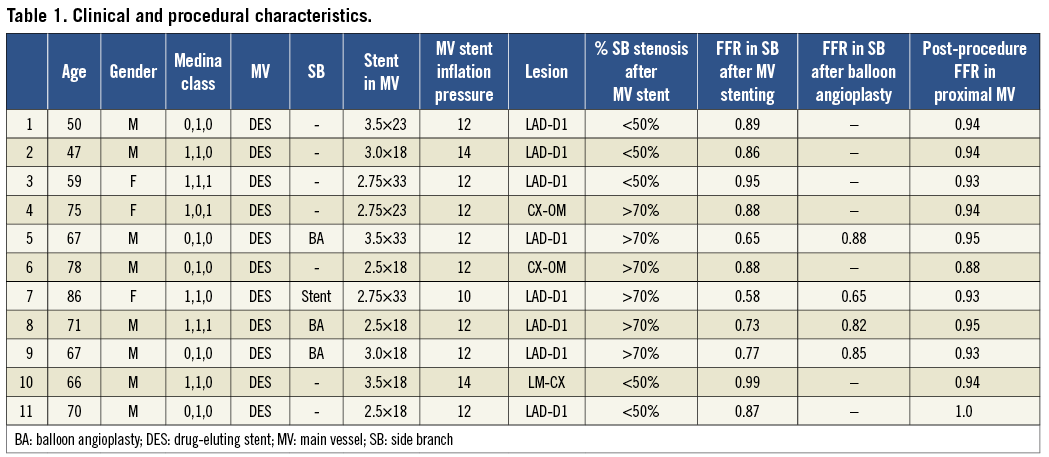
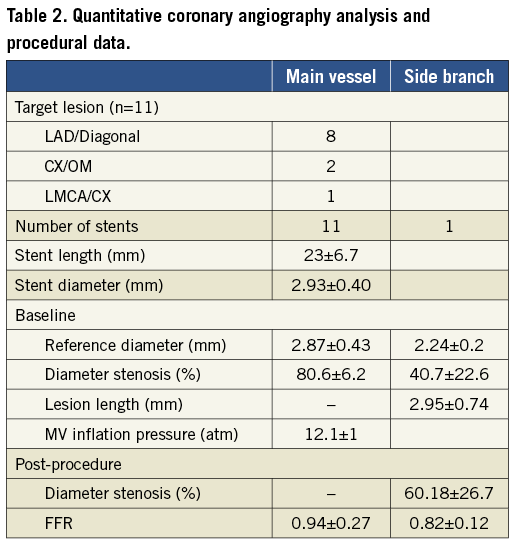
After MV stenting, the mean FFR measured in the SBs was 0.82±0.12, and four lesions were functionally significant (mean FFR: 0.6±0.08, range 0.58 to 0.77). All of them with FFR ≤0.80 had >70% coronary stenosis. The lesions with FFR ≤0.80 underwent SB intervention with balloon inflation over the third guidewire. In these patients, SB rewiring was successfully performed with a third guidewire without removing the JPW. In three of them, FFR was significantly increased from 0.71±0.06 to 0.85±0.03 after SB balloon inflation, and the JPW was removed carefully with the third wire left in the SB. Finally, kissing balloon inflation was performed at the bifurcation. However, one patient still had FFR ≤0.80 after SB balloon inflation. In this case, after removing the JPW, a stent was implanted in the SB using the TAP-stenting technique. No difficulty was experienced in removing the JPW from the SB in cases which underwent SB intervention.
In 7/11 patients, a satisfactory FFR level (>0.80 ) was maintained after MV stenting so that the JPW wire was removed without the need for SB intervention. In all patients, mean FFR measured in the MV proximal to jailed side branches was 0.94±0.27 (range, 0.86 to 1.0) at the end of the procedure. We did not encounter difficulty in removing the JPW. Procedures were successfully accomplished in all cases without complications, such as damage of the pressure sensor, failure to measure FFR value, removing the polymer coating, and entrapment or fracture of the JPW.
Discussion
The main finding of the present small study is that the JPW technique in the PS of bifurcation lesions is safe and technically feasible. The JPW may be removed with a degree of difficulty which is comparable to that encountered during jailed standard floppy wire removal. Nevertheless, if difficulty is encountered in removing the JPW, we should not use force in order to avoid pressure wire fracture/damage/rupture. A rescue ballooning with a low-profile balloon over the JPW may facilitate removal of the wire.
We do not have experience in the application of this technique in utilising another commercially available pressure wire. In conclusion, our limited experience suggests that the JPW technique in the PS may be a feasible approach. However, before starting larger studies it would be necessary to have input from engineers, ideally with tests in vitro, to support the feasibility of the JPW.
| Impact on daily practice The fractional flow reserve (FFR) technique is emerging as a feasible option in bifurcation interventions and is being used increasingly in the provisional strategy. However, side branch (SB) access with a pressure wire after main vessel stenting may be difficult, sometimes impossible. In that regard, the SB FFR evaluation usually prolongs the procedure, and the procedure may lead to complications, such as dissections and the need for additional stenting due to difficult wiring. Although not primarily designed for jailing, the jailed pressure wire technique in bifurcation lesions may offer a less invasive alternative to conventional procedure by avoiding SB rewiring and interventions, and may shorten the procedure time in daily practice. |
Conflict of interest statement
The authors have no conflicts of interest to declare.

