Abstract
Coronary bifurcation lesions (CBLs) represent a common and challenging subset of coronary artery disease requiring percutaneous coronary intervention (PCI). While drug-eluting stents (DES) remain the cornerstone of treatment, their use is associated with risks such as restenosis, thrombosis, side branch (SB) jailing and the need for prolonged dual antiplatelet therapy. Drug-coated balloons (DCBs) have emerged as a promising alternative, delivering antiproliferative drugs without permanent implants, thereby reducing the risk of late complications and preserving native vessel geometry. This review explores the role of DCBs in CBL management, particularly for SB treatment within the provisional stenting strategy. Evidence from clinical studies indicates that DCBs significantly reduce late lumen loss and restenosis in the SB compared to plain balloon angioplasty, while simplifying PCI procedures and avoiding extensive stenting. Furthermore, hybrid/blended strategies combining DCBs with DES have shown superior clinical and angiographic outcomes in true CBLs compared to DES-only approaches. Despite their potential, the adoption of DCBs faces challenges, including the need for optimal lesion preparation and a lack of standardised procedural techniques. Existing randomised controlled trials are limited by small sample sizes, design heterogeneity, inclusion of bare metal stents either as comparators or as part of the treatment strategy, and inconsistent use of key procedural steps such as proximal optimisation technique and kissing balloon inflation. This manuscript aims to provide interventional cardiologists with practical guidance for managing CBLs, focusing on the effective integration of DCBs into standalone and hybrid strategies. By emphasising procedural optimisation and complication reduction, this review seeks to promote more standardised and reproducible approaches in clinical practice.
Coronary bifurcation lesions (CBLs) are frequently encountered in routine clinical practice, accounting for approximately 20% of percutaneous coronary interventions (PCI)1. Bifurcation PCI are associated with lower procedural success rates and worse clinical outcomes compared to PCI in lesions without a bifurcation. Despite advancements in new-generation drug-eluting stents (DES), the use of permanent metallic implants comes with some potential drawbacks. On one hand, the requirement for prolonged dual antiplatelet therapy (DAPT) can pose risks, particularly in elderly patients and those deemed at high bleeding risk (HBR)2. On the other hand, a constant risk of long-term stent-related complications (i.e., in-stent restenosis, stent thrombosis, and neoatherosclerosis) with an incidence rate of approximately 2-3% per stent per year has been described with current-era devices3. Drug-coated balloons (DCBs) offer theoretical advantages in the setting of bifurcations when integrated into a single-stent provisional approach or as a standalone treatment. These include targeted antiproliferative drug delivery to the side branch (SB), reduced risk of neocarina and stent thrombosis due to the absence of stent struts, and avoidance of issues like stent malapposition and polymer deformation, which may impair the antiproliferative drug delivery2. However, evidence supporting the use of DCBs in the context of CBLs remains limited and primarily focuses on their application for SB treatment. Furthermore, the use of DCBs for de novo lesions, including bifurcations, is not yet endorsed in current European and American guidelines4. This review aims to provide a practical overview of the DCB-based PCI techniques for CBLs.
DCB technologies and armamentarium
DCBs mainly differ in the type of antiproliferative drug eluted (i.e., paclitaxel [PTX] vs -limus) and in the coating (excipient) used to facilitate optimal drug release into the vessel wall. A detailed description of the technologies available for DCBs is beyond the scope of the present review, but some information is available in Supplementary Appendix 1. Pivotal clinical trials have demonstrated angiographic non-inferiority of certain -limus technologies compared to PTX-eluting counterparts, while others have shown inferiority, in both cases of in-stent restenosis (ISR) and de novo lesions5. A recent meta-analysis including 1,861 patients showed angiographic superiority of PTX-coated balloons (PCBs; late lumen loss [LLL] –0.11 mm, 95% confidence interval [CI]: –0.23 to 0.02), while there was no significant difference in target lesion failure (TLF; odds ratio [OR] 1.01, 95% CI: 0.75-1.35)6. Old-generation PCBs faced limitations in navigability. New-generation and -limus-based devices are designed to provide enhanced navigability and performance. This is of particular importance in the setting of CBLs, where SB recrossing through main vessel (MV) struts can be challenging with bulky, old-generation devices. By avoiding vessel caging, DCBs have been linked to the possibility of positive vessel remodelling. Paclitaxel, especially, has been seen to lead to an increased diameter in about 60% of the cases in de novo lesions, while the same phenomenon occurs to a lesser degree (about 30% of the cases) with sirolimus. In CBLs, the positive remodelling effect may be attenuated when a DCB is applied to the SB in the setting of provisional MV stenting. This is likely due to the presence of a jailed SB, where the mechanical constraint and altered vessel substrate resulting from stent struts across the SB ostium may limit the extent of positive vessel remodelling typically induced by the antiproliferative drug.
Rationale and advantages of DCB use in coronary bifurcations
The major advantages of DCBs are (1) homogeneous drug transfer to the vessel wall, with a rapid release of high concentrations of the drug that are sustained in the vessel wall for weeks; (2) the absence of inflammatory polymers and permanent implants, which reduces potential triggers for neoatherosclerosis and late thrombosis occurrence (e.g., metallic neocarina); (3) the absence of permanent implants, which spares the side branch from permanent jailing, preserves the native arterial geometry, and maintains physiological vasomotion; and (4) the possibility of DAPT de-escalation, both in terms of duration and P2Y12 inhibition intensity. According to the European Society of Cardiology and the European Bifurcation Club (EBC), the provisional stepwise approach, starting with the implantation of a stent in the MV across the SB, is considered the default strategy for CBLs78. The EBC recommends a “KISS” (keep it simple and safe) principle, which involves limiting the number of stents used. MV-only stenting is recommended in most cases with provisional SB stenting, whereas a two-stent approach should be reserved for patients with complex lesions involving large and diseased SBs7. The EBC has emphasised DCBs as an area of interest in this scenario, recognising them as a valuable option to preserve a provisional strategy, particularly when the anatomy is suitable (e.g., in Medina 0,0,1 classification). Moreover, the international DCB consensus group has further endorsed the role of DCBs in CBLs2. Therefore, in the setting of CBLs, DCBs offer the following potential advantages. Firstly, DCBs potentially increase the success of a provisional strategy, as compared to plain old balloon angioplasty (POBA)9. Secondly, DCBs reduce PCI complexity by respecting the original anatomy of the carina and reducing the need for a two-stent approach, and therefore the incidence of device-related failure. Thirdly, DCBs allow for the possibility of late lumen enlargement10. Lastly, SBs are often small vessels (with a diameter ≤2.75 mm), but subtending a non-negligible area of the myocardium, and importantly, DCBs have been repeatedly demonstrated to be non-inferior to DES in the treatment of small vessels11121314.
How to use DCBs in coronary bifurcations
Before antiproliferative drug delivery to the treated segment, proper lesion preparation is key. Following relevant SB wire protection in accordance with EBC recommendations (reference vessel diameter ≥2.0 mm, >10% of the myocardium supply, ≥73 mm SB length)15, accurate predilatation towards the MV and/or SB (if diseased) should be performed using a semi- or non-compliant (NC) balloon with a balloon-to-artery ratio of 1:12. In the case of expansion failure of a standard balloon, high-pressure NC balloons, cutting, and/or scoring balloons should be used. In case of severe calcification, calcium debulking strategies (i.e., rotational atherectomy/intravascular lithotripsy) are recommended. For an isolated SB stenosis (Medina 0,0,1), a scoring/cutting balloon is preferable to ensure a good predilatation result with controlled dissection and minimal recoil. SB predilatation before MV stenting is generally not recommended but may be useful in case of severe calcification, angulated side branch stenosis, difficult SB wiring, or compromised SB flow after wiring15. While it can help to maintain SB flow after MV stent implantation and facilitate rewiring by increasing the ostial SB lumen, it also increases the risk of SB dissection and may complicate further intervention16. DCB sizing should be performed at a balloon-to-vessel ratio of 0.8-1:1, with a recommended inflation time of at least 30-60 s to allow proper release of the drug, while inflating at low pressures (6-10 atm). Such pressures should not be exceeded, as the mechanical expansive properties of DCBs can pose a risk of dissection. Although strong scientific evidence to support specific and standardised cutoffs is currently lacking, according to the consensus documents from the International DCB Consensus Group and the DCB Academic Research Consortium, a residual stenosis <30% (by visual estimation; <40% by quantitative coronary angiography) is considered acceptable following DCB therapy application, as well as non-flow-limiting dissections (not associated with Thrombolysis in Myocardial Infarction <3, prolonged electrocardiographic changes or angina)24. The role of physiological assessment or intravascular imaging in deciding to apply bailout stenting or not is still under debate, and a common expert consensus is not available yet. However, during provisional stenting, assessment of the jailed SB should be considered in cases of ostial “pinching” to determine the necessity of additional SB intervention17. Periprocedural measurements showing normal fractional flow reserve (FFR) or instantaneous wave-free ratio (iFR) in the jailed SB have been linked to favourable functional outcomes at follow-up, supporting a conservative management approach. Overall, functional evaluation of the jailed SB has been shown to reduce the need for SB stenting during provisional strategies18.
Leave nothing behind
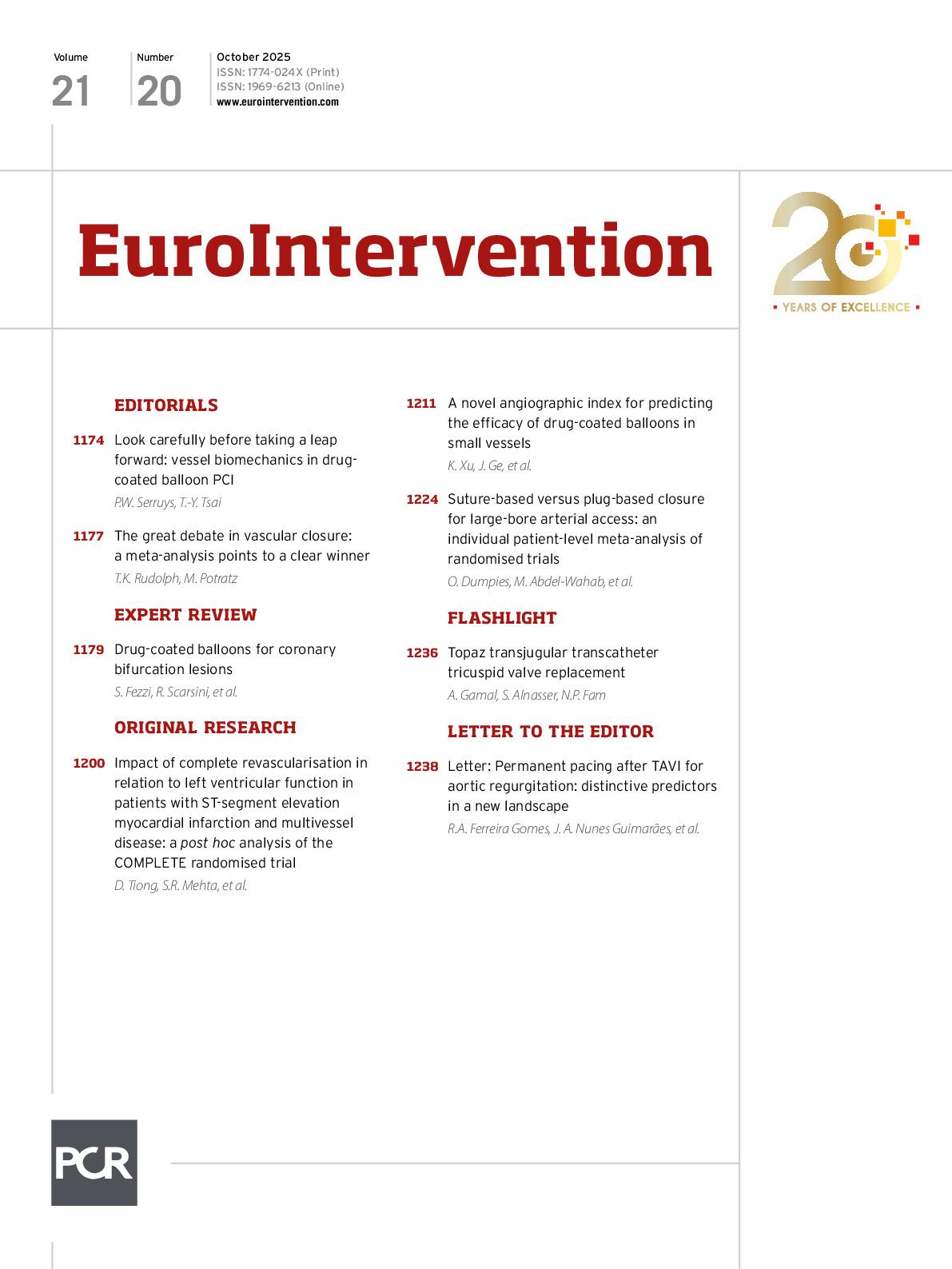
A DCB-only approach to CBLs is appealing, as it theoretically avoids carina shift. The “leave nothing behind” strategy theoretically applies to the entire spectrum of CBLs if the predilatation result is satisfactory. However, evidence supporting the use of a DCB-only approach in de novo lesions, beyond small vessels, remains limited. Further studies are needed, particularly in large-calibre vessels and left main disease. In case of Medina 0,0,1 CBLs with an isolated SB lesion, a simple approach with SB-only treatment can be considered, leaving the MV untouched (Figure 1, Figure 2A). In case of a disease-free SB (Medina 1,1,0; 0,1,0; 1,0,0), a DCB treatment of the MV across the SB should be considered (Figure 1). In this approach, the ostium of a small, diseased SB may improve during follow-up. In case of true CBLs (Medina 1,1,1; 1,0,1; 0,1,1), sequential DCB dilatation is recommended, starting in the SB and then in the MV (Figure 2B, Figure 2C, Figure 3). Kissing DCB inflation should be avoided: firstly, this may increase the risk of dissections and perforation in the proximal MV not protected by a stent; secondly, it requires prolonged time in the blood with drug loss; and lastly, the proximal interaction between the two balloons does not enable proper concentric coverage of the vessel, with suboptimal drug delivery to the vessel wall19. 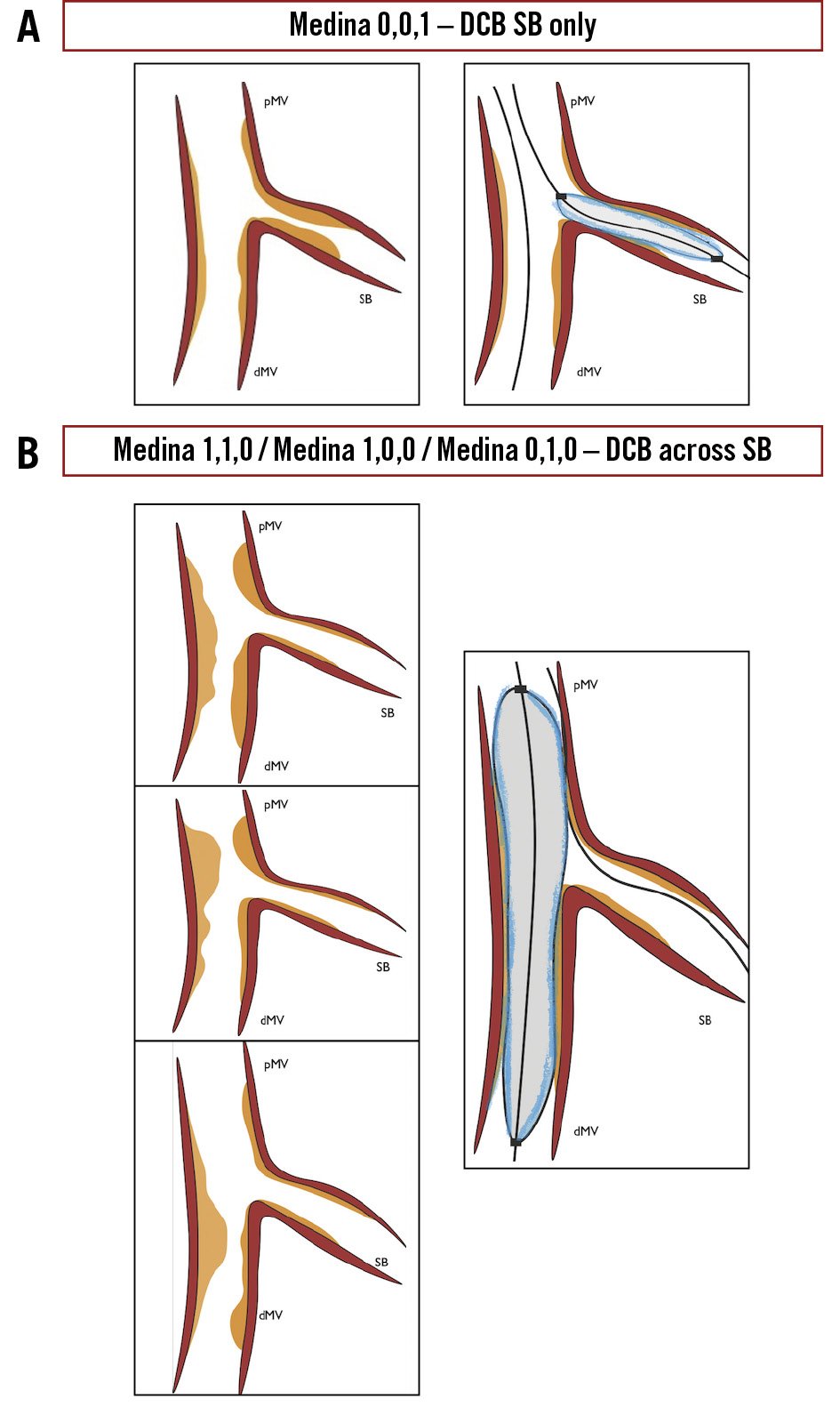
Figure 1. Coronary bifurcation treatment with DCB only. A) DCB in the SB only is the preferred strategy in an isolated SB stenosis (Medina 0,0,1). Following MV and SB wiring and adequate lesion preparation (scoring and cutting balloons preferred), DCB inflation is applied specifically to the SB, extending the DCB 2 mm into the MV to ensure proper drug concentration in the ostium. B) DCB-only in the MV (DCB across the SB) is the approach that should be used for more complex lesions where both the MV and a small SB are involved. Following lesion preparation, DCB inflation is applied across the SB. DCB-only in both the MV and SB: sequential treatment of the SB first, then the MV with a DCB. In most cases, KBI is avoided. DCB: drug-coated balloon; dMV: distal main vessel; KBI: kissing balloon inflation; MV: main vessel; pMV: proximal main vessel; SB: side branch
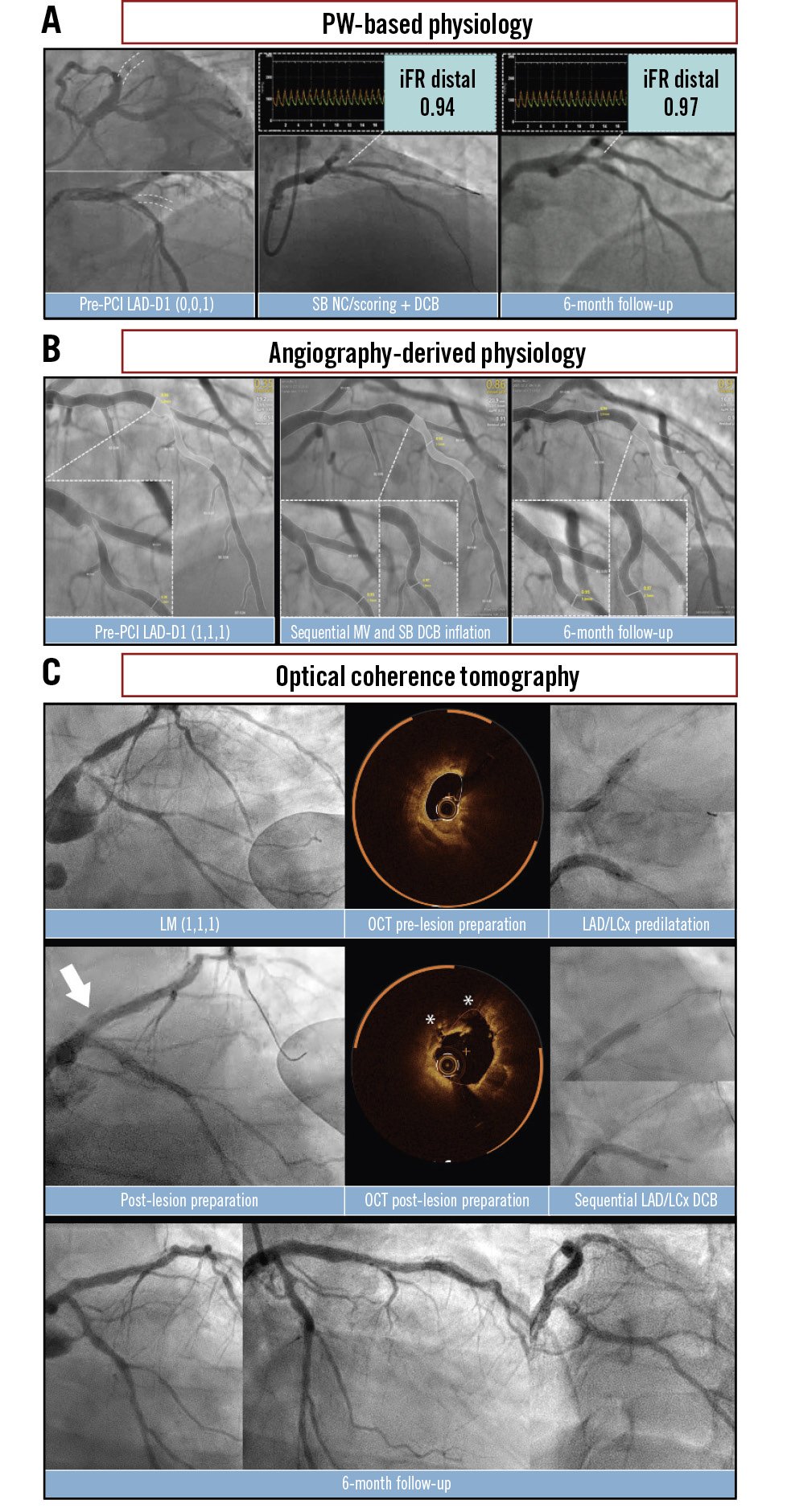
Figure 2. Coronary physiology and intravascular imaging guidance for a DCB-only approach. A) A case of LAD-D1 CBL (Medina 0,0,1). After wiring both the MV and SB, lesion preparation was performed using a combination of non-compliant and scoring balloons. A 2.5×20 mm sirolimus-coated DCB was inflated in the SB to ensure optimal drug delivery at the ostium. Final physiological assessment with iFR showed a non-ischaemic value (iFR 0.94), which was further confirmed at follow-up (iFR 0.97). B) A case of LAD-D1 CBL (Medina 1,1,1), showing ischaemic values of single-view Murray law-based quantitative flow ratio in both the MV (μFR 0.35) and SB (μFR 0.74). Following successful wiring of both the MV and SB, lesion preparation was performed using a KBI technique with non-compliant balloons. Sequential inflations of paclitaxel-coated DCBs were then carried out in the MV (3.5×30 mm) and SB (2.5×20 mm), resulting in a favourable angiographic and functional outcome, with postprocedural μFR values of 0.86 in the MV and 0.97 in the SB. These results were further confirmed at elective follow-up (μFR 0.91 and 0.93, respectively). C) A case of a calcified left main coronary bifurcation lesion (Medina 1,1,1). OCT revealed circumferential calcium requiring plaque modification. Lesion preparation was performed using orbital atherectomy, followed by non-compliant and cutting balloons. After lesion preparation, OCT confirmed effective calcium modification with visible fractures (asterisks). Sequential inflations of paclitaxel-coated DCBs were then performed in the MV (3.5×15 mm) and SB (3.0×20 mm), resulting in favourable angiographic and OCT outcomes. Elective follow-up confirmed healing of dissections and positive vessel remodelling in both the LCx and LAD. CBL: coronary bifurcation lesion; D1: first diagonal branch; DCB: drug-coated balloon; iFR: instantaneous wave-free ratio; KBI: kissing balloon inflation; LAD: left anterior descending artery; LCx: left circumflex artery; LM: left main; MV: main vessel; NC: non-compliant; OCT: optical coherence tomography; PCI: percutaneous coronary intervention; PW: pressure wire; SB: side branch; μFR: Murray law-based quantitative flow ratio
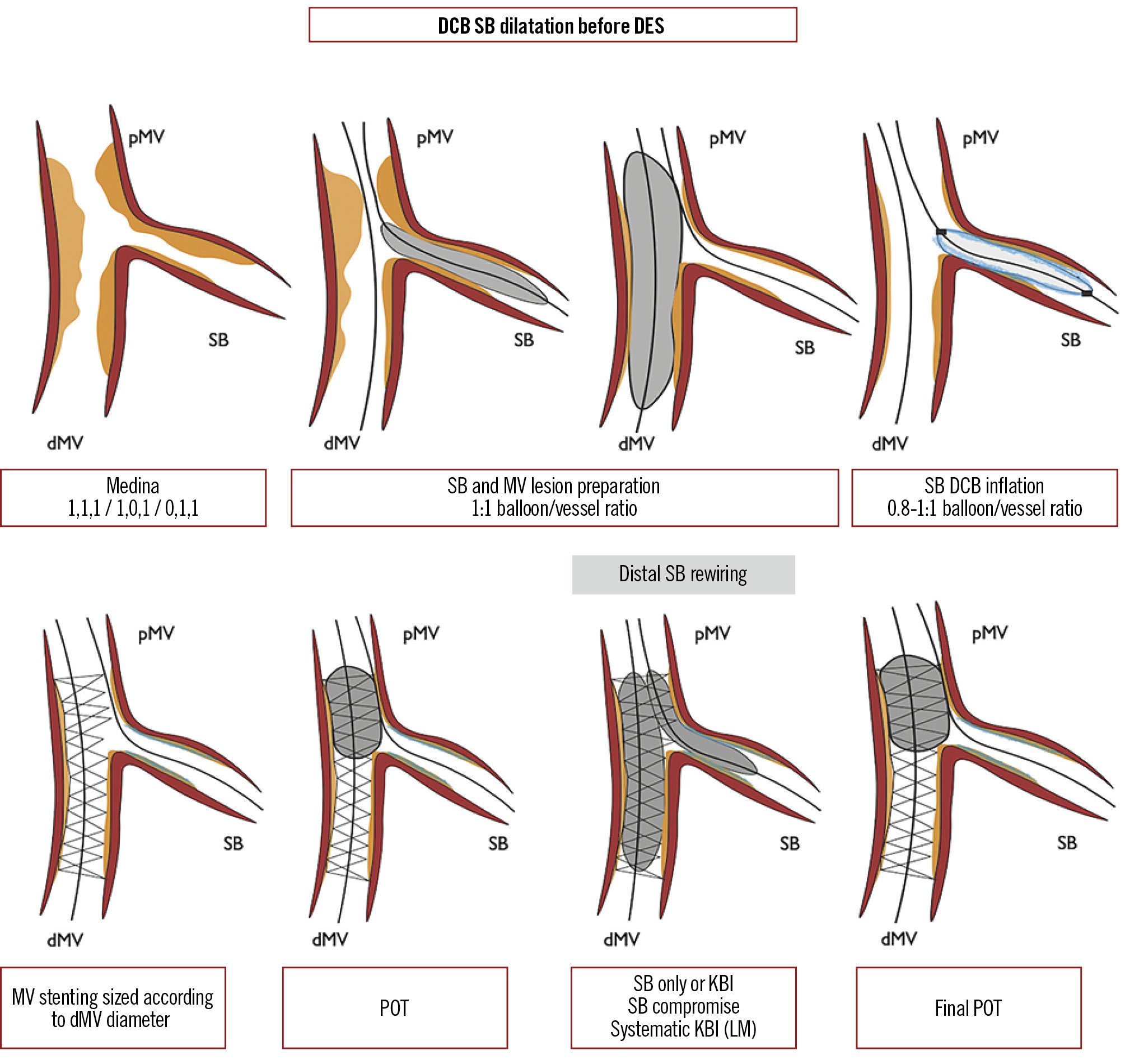
Figure 3. Side branch treatment with a DCB before provisional DES implantation. In case of a true CBL, DCB inflation towards the SB is performed after lesion preparation in both branches and followed by provisional DES implantation towards the MV. POT is then performed. In case of a suboptimal result (i.e., SB compromise) or a need for systematic KBI (i.e., left main bifurcation), SB distal rewiring is performed, followed by either POT-side-POT or KBI and final POT. CBL: coronary bifurcation lesion; DCB: drug-coated balloon; DES: drug-eluting stent; dMV: distal main vessel; KBI: kissing balloon inflation; LM: left main; MV: main vessel; pMV: proximal main vessel; POT: proximal optimisation technique; SB: side branch
Blended approach
The blended/hybrid approach to CBLs inherently integrates the use of DCBs in the provisional DES implantation philosophy, allowing for a reduction in the overall stent burden and providing angiographic and clinical advantages compared to POBA alone. SB treatment with a DCB can be delivered either before or after DES implantation across the SB. In the former case, a DCB is first applied to the side branch, followed by DES implantation in the main vessel, after which the mandatory proximal optimisation technique (POT) is performed (Figure 3, Figure 4A). In case of a suboptimal SB result, the procedure may be continued either with kissing balloon inflation (KBI) and re-POT or POT-side-POT inflations. Theoretically, these further inflations might interact with the antiproliferative drug that has already been delivered to the SB. In the latter case, DCB treatment is performed as a final step following DES implantation across the SB, POT, SB rewiring and dilatation, DCB application to the SB, followed by optional KBI and mandatory final re-POT (Figure 4B, Figure 5). It has been postulated that such an approach might be associated with suboptimal drug delivery, as the interaction with the DCB and stent struts might lead to drug loss and hamper proper drug delivery to the SB. Furthermore, the deliverability of cutting or scoring balloons, which is inherently limited because of their device profile and mechanical characteristics, is further compromised in the setting of a jailed SB, potentially affecting adequate lesion preparation. It should be noted that the timing and sequence for DCB use in bifurcation PCI remain topics of ongoing debate, as robust evidence to guide these decisions is currently limited. Current recommendations are largely based on expert opinion and clinical experience, emphasising the need for further large prospective randomised studies to establish more definitive guidance.
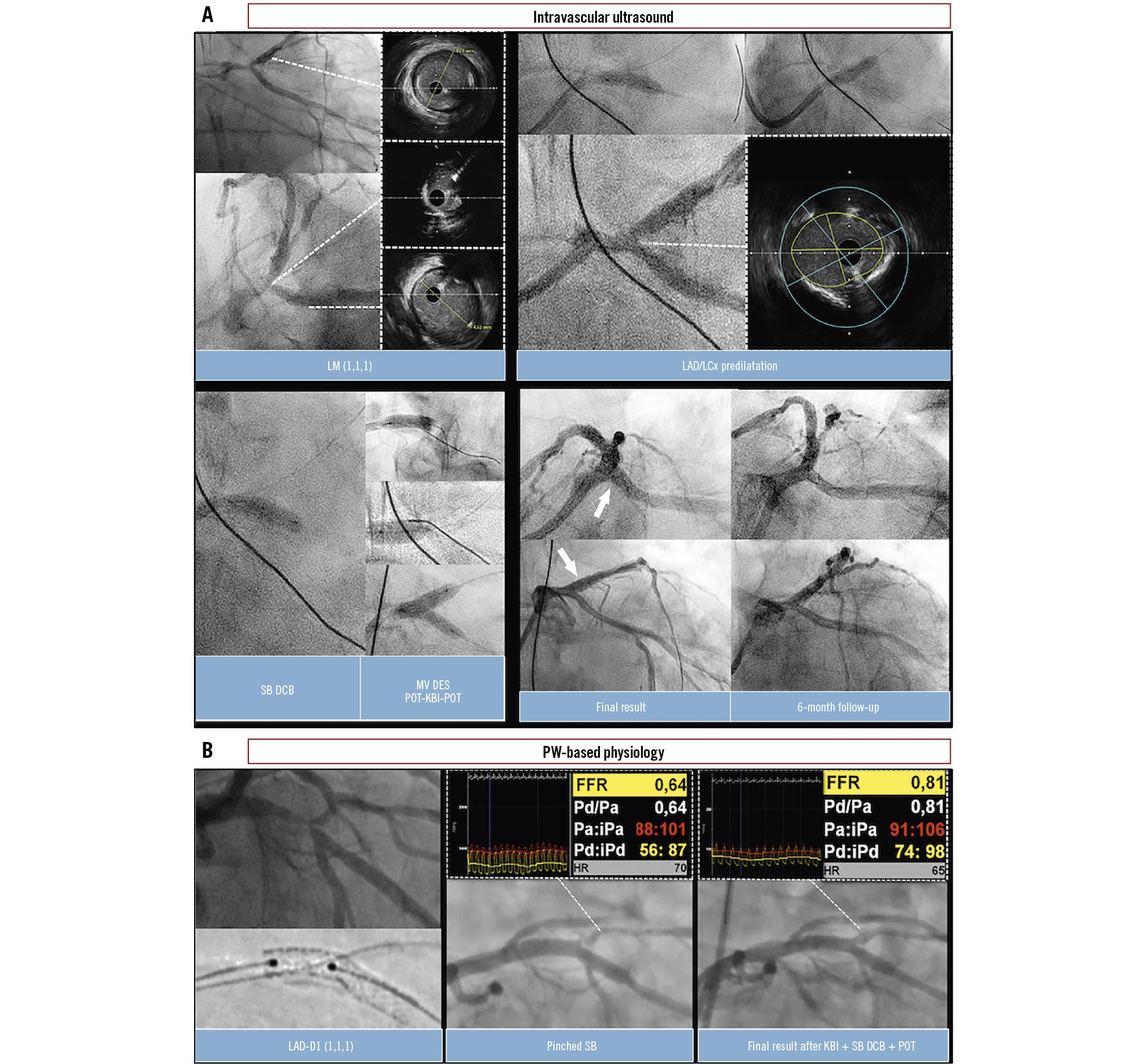
Figure 4. Coronary physiology and intravascular imaging guidance for a DCB/DES blended approach. A) A case of LM CBL (Medina 1,1,1). IVUS initially revealed a significant stenosis at the ostium of the LCx. Lesion preparation was performed using a 4.0 mm cutting balloon to predilatate the LAD, LCx, and LM. Following predilatation, the IVUS result in the LCx was deemed satisfactory, with restored flow and less than 30% recoil. However, IVUS assessment indicated unacceptable recoil in the LM segment. A 4.0×15 mm paclitaxel-coated DCB was first applied to the LCx for 30 seconds. Subsequently, a provisional DES implantation (5.0×16 mm) was performed from the LM ostium into the LAD. POT was then performed using a 5.5×6 mm NC balloon, followed by KBI (4.0 mm in the LAD, 3.5 mm in the LCx) and final POT. The final angiographic and IVUS results were satisfactory, showing minimal lumen areas of 14 mm² in the LAD, 7.7 mm² in the LCx, and 19.5 mm² in the LM. Three-month follow-up angiography confirmed a durable and favourable result of this blended approach. B) A case of LAD-D1 CBL (Medina 1,1,1). Following lesion preparation of the MV with NC balloons, a DES (3.5×22 mm) was implanted across the D1 using a provisional approach. POT was then performed with a 4.0×8 mm NC balloon. Subsequent angiography revealed a pinched SB with ischaemic FFR values (FFR 0.64) in the D1. After rewiring the SB, KBI was performed using 3.0 mm and 2.5 mm NC balloons, followed by inflation of a paclitaxel-coated DCB (2.5×20 mm) in the SB and the mandatory final re-POT. This strategy resulted in a favourable angiographic outcome and marked functional improvement, with FFR increasing to 0.81. CBL: coronary bifurcation lesion; D1: first diagonal branch; DCB: drug-coated balloon; DES: drug-eluting stent; FFR: fractional flow reserve; IVUS: intravascular ultrasound; KBI: kissing balloon inflation; LAD: left anterior descending artery; LCx: left circumflex artery; LM: left main; MV: main vessel; NC: non-compliant balloon; POT: proximal optimisation technique; PW: pressure wire; SB: side branch
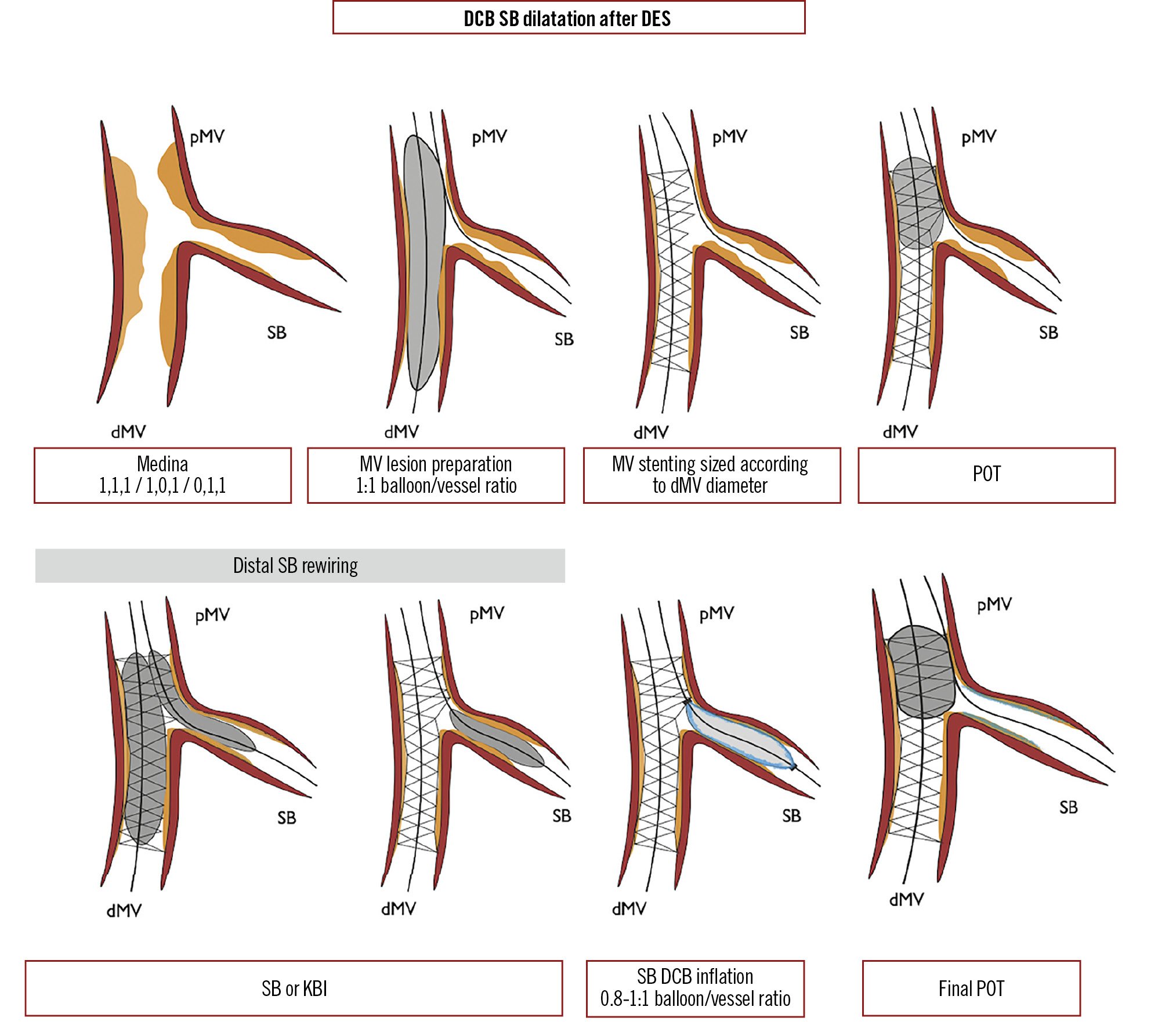
Figure 5. Side branch treatment with a DCB after provisional DES implantation. In case of a true CBL, DCB inflation towards the SB is performed as a final step following provisional DES implantation across the SB, POT, and SB dilatation to prepare the lesion and open the struts for the DCB. Final POT is mandatory. CBL: coronary bifurcation lesion; DCB: drug-coated balloon; DES: drug-eluting stent; dMV: distal main vessel; KBI: kissing balloon inflation; pMV: proximal main vessel; POT: proximal optimisation technique; SB: side branch
Available evidence
DCB to the main vessel (DCB-only strategy)
Few, relatively small studies have investigated the use of DCBs in the treatment of the MV. In a prospective, observational, single-centre study, Schulz et al20 investigated the feasibility and early safety of a DCB-only (PTX; SeQuent Please [B. Braun]) approach in the management of CBLs. Thirty-nine patients with de novo CBLs and an SB ≥2 mm were included; one-third of these cases were left main (LM) bifurcations. Low rates of 4-month angiographic restenosis (3.3% in the SB and 6.7% in the MV) and of major adverse cardiac events (MACE; 7.7%) were observed. Bruch et al21, in an observational, multicentre registry, assessed the feasibility of a DCB-only strategy (PTX; SeQuent Please) in the treatment of CBLs of any Medina class with an SB >2 mm. Almost half of all treated bifurcations were Medina type 1,1,1, followed by Medina type 0,1,1. Bailout stenting with a bare metal stent (BMS) was performed in the MV and/or the SB in case of flow-limiting dissections and/or excessive angiographic acute recoil. Overall, 127 patients were enrolled (130 lesions): 53.8% underwent a DCB-only strategy; in 34.6%, one BMS was implanted in the MV; in 8.5%, a BMS was implanted in the SB; and in 3.1%, two stents (MV and SB) were implanted. At 9 months, the target lesion revascularisation (TLR) rate was 4.6% in the absence of any thrombotic events in the treated vessels, with a MACE rate of 6.2%. PCB inflation in the MV appears to induce beneficial late luminal enlargement, as it does in the SB ostium, as shown using optical coherence tomography (OCT)22. Ke et al randomised 60 patients with true bifurcation lesions either to a standard two-stent strategy or DCB-only strategy (PTX; SeQuent Please)23. LLL at 12 months was significantly lower with the DCB-only approach both in the MV and the SB (0.05±0.24 mm vs 0.25±0.35 mm; p=0.013 and –0.02±0.19 mm vs 0.11±0.15 mm; p=0.005, respectively), displaying positive remodelling in the SB. In the recent CAGE-FREE 1 randomised clinical trial, DES implantation proved superior to DCB-only PCI (PTX-coated Swide DCB [Shenqi Medical]) for non-complex lesions in an all-comers population. Notably, in subgroup analyses of non-true bifurcations and small vessels, both treatment strategies showed comparable outcomes24.
DCB to the side branch
Several studies investigated the feasibility and safety of DCBs used for SB treatment in the context of provisional MV stenting. The superiority of DCBs compared to POBA for SB treatment in the context of provisional MV stenting has been confirmed by two meta-analyses2526. In particular, Zheng et al26 included 934 patients from 10 studies (five randomised controlled trials [RCTs]), showing that DCB treatment of the SB is associated with lower LLL, smaller diameter stenosis and a lower rate of binary restenosis at the elective angiographic follow-up, as compared to POBA. The rate of MACE was significantly lower in the DCB group at 9 months (OR 0.21, 95% CI: 0.05-0.84; p=0.03) and 12 months (OR 0.45, 95% CI: 0.22-0.90; p=0.02). However, DCB treatment was not associated with a reduced incidence of TLF. Notably, several studies providing preliminary evidence in favour of DCB treatment of the SB are hampered by the combined implantation of a BMS to the MV. These data are reported in detail in Supplementary Appendix 1. A comprehensive overview of the angiographic outcomes of SB treatment with DCBs as compared to POBA is summarised in Figure 6. 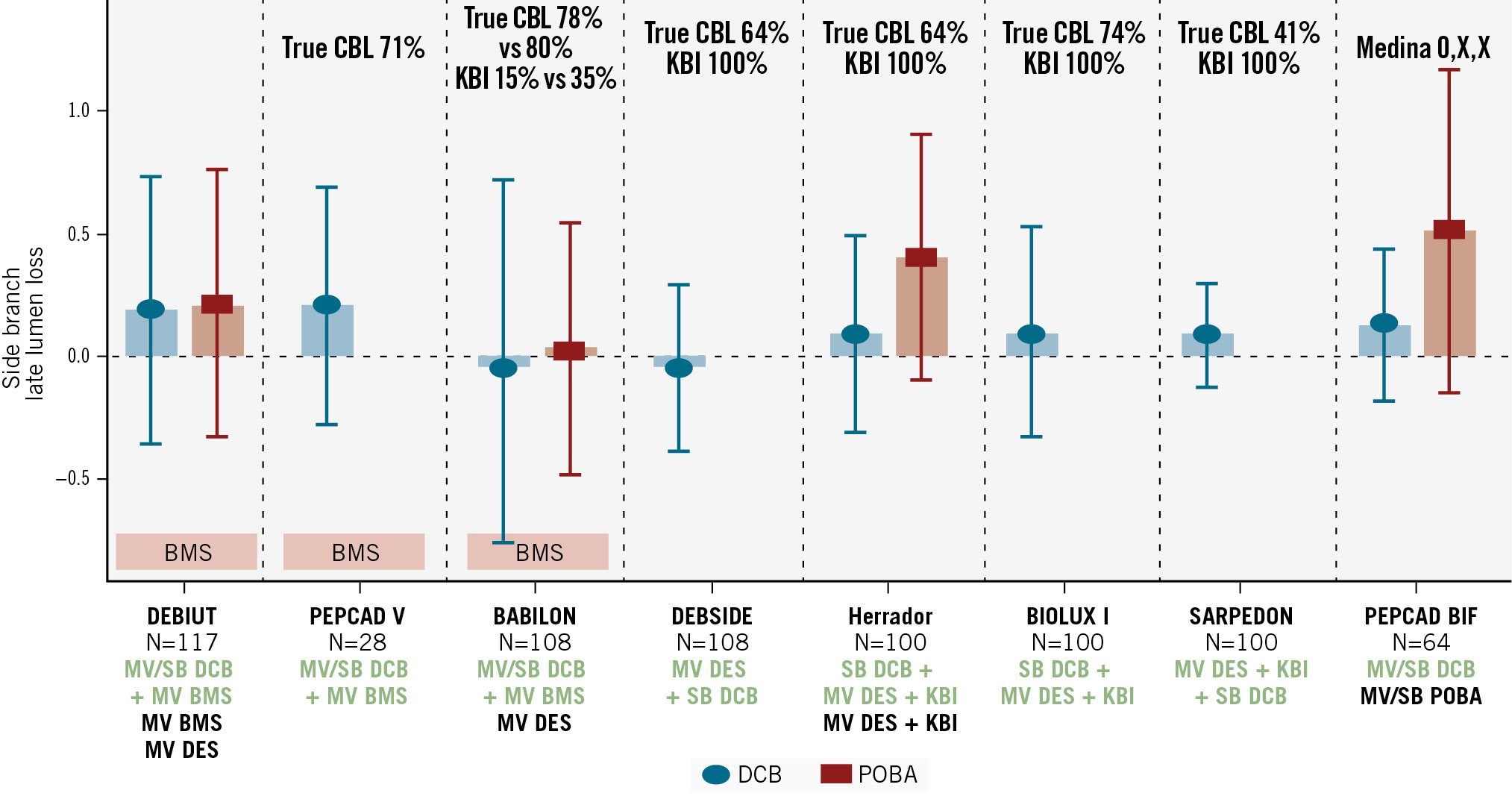
Figure 6. Angiographic outcomes of SB treatment with DCBs as compared to POBA. Angiographic late lumen loss of the side branch following DCB (blue) or POBA (red) treatment in randomised clinical trials and registries. The rate of true CBL and KBI is reported at the top. The number of patients included, the DCB strategy adopted (green), and the comparator (black) are reported at the bottom. DEBIUT, PEPCAD V, and BABILON combined the use of DCBs and BMS, with DCB inflation both towards the SB and the MV before stent implantation in the MV. BMS: bare metal stent; CBL: coronary bifurcation lesion; DCB: drug-coated balloon; DES: drug-eluting stent; KBI: kissing balloon inflation; MV: main vessel; POBA: plain old balloon angioplasty; SB: side branch
DCB to the SB before provisional stent implantation IN the MV
In the pilot, single-arm, observational DEBSIDE trial27 (n=52 patients), DCB dilatation (PTX; Danubio [Minvasys]) of the SB was performed first, followed by a DES towards the MV and final kissing balloon with plain old balloons. Based on a population of 52 patients, such an approach was seen to be feasible and safe, with a negative LLL (–0.04±0.34 mm) and no restenosis in the SB at the elective angiographic follow-up at 6 months. The incidence of TLR was 10% in the MV and 2% in the SB. A similar approach was evaluated in the single-arm, observational BIOLUX-I28 trial that included 35 patients with CBLs. SB dilatation with a DCB (PTX; Pantera Lux [Biotronik]), performed before MV stenting, was associated with good angiographic LLL (at 9 months 0.10±0.43 mm) and clinical results (12-month vessel-oriented composite endpoint 2.9%). The limitation of the DEBSIDE and BIOLUX-I studies was that there was no control treatment (i.e., POBA or DES in the SB).
DCB to the SB after provisional stent implantation IN the MV
Herrador et al29, in a prospective, observational, non-randomised study including 100 patients, compared treatment of the SB with a DCB (PTX; SeQuent Please) or with POBA, after DES implantation in the MV. The use of a DCB in the SB was associated with better angiographic outcomes, in terms of LLL (0.09±0.40 mm vs 0.40±0.50 mm; p=0.01) and a lower incidence of restenosis (7% vs 20%; p=0.08) at 12 months. This was confirmed in the single-arm, observational SARPEDON30 study and further in the PEPCAD-BIF31, BEYOND32 and in the recent large DCB-BIF33 RCTs. In the SARPEDON30 study, 64 patients were randomised to either a DCB (PTX; SeQuent Please) or POBA treatment of the SB after DES implantation to the MV. The study included only CBLs without disease in the proximal MV (Medina 0; X; X) and mainly included small vessels (mean reference vessel diameter 2.4 mm). DCB treatment in the SB was associated with superior angiographic results at 9 months, both in terms of LLL (0.13±0.31 vs 0.51±0.66; p=0.045) and ISR occurrence (6% vs 26%; p=0.045) as compared to POBA. The multicentre BEYOND32 1:1 RCT (n=222 patients) demonstrated that SB dilatation with DCB (PTX; Bingo [Yinyi Biotech]) after MV provisional stenting in non-left main CBL was associated with superior angiographic results at 9 months (degree of stenosis 28.7±18.7% vs 40±19%; p=0.001), but comparable clinical outcomes (MACE rate 0.9% vs 3.7%; p=0.16) as compared to POBA alone. The blended use of DCBs and DES in the setting of de novo LM true CBLs is particularly intriguing. In a recent real-world multicentre, propensity-matched study including 597 patients, the blended use of a DES+DCB was associated with lower rates of clinically driven TLR (2.91% vs 9.42%; p=0.007), TLF (9.60% vs 17.14%; p=0.026), and stent thrombosis (0.00% vs 2.89%; p=0.030) at 2 years, as compared to a DES-only strategy (provisional stenting or two-stent strategies)34. The recent DCB-BIF trial33 is the largest RCT assessing the clinical performance of SB treatment with DCB in comparison to non-compliant balloons, in true non-complex bifurcation lesions undergoing provisional stenting. Overall, 784 patients with true coronary bifurcation lesions were enrolled and randomised to DCBs (n=391) or NC balloons (n=393). DCB treatment demonstrated superiority compared to non-compliant balloon POBA, by reducing the risk of MACE at 12 months (7.2% vs 12.5%, hazard ratio 0.56, 95% CI: 0.35-0.88; p=0.013), primarily attributed to a reduction in myocardial infarction. No significant differences were observed between groups in procedural success, crossover to a two-stent strategy, all-cause mortality, revascularisation, or stent thrombosis. Interestingly, despite this difference in MI, TLR rates remained similar between the groups. Upon critical review, the higher number of MIs in the non-compliant POBA arm may be attributed to early, predominantly periprocedural events that did not lead to revascularisation. Secondly, the observed benefit of DCBs may stem not only from the pharmacological action of paclitaxel but also from longer balloon inflations, which may reduce acute recoil, dissection, adjunctive procedures, and late restenosis. Despite several limitations related to heterogeneity in terms of study design, inclusion/exclusion criteria, type of DCBs and DES used, the available evidence supports the use of DCBs in the setting of provisional stenting of CBLs when a balloon dilatation of the SB is planned (i.e., kissing balloon, POT-side-POT). In the setting of LM PCI, the available evidence is still limited. Liu et al retrospectively enrolled 100 patients with true LM bifurcation lesions that were divided into two DES groups (both MV and SB) as well as a DES in MV and DCB in SB group35. At the elective angiographic follow-up, the minimal lumen diameter in the left circumflex coronary artery (LCx) ostium was higher in the DES+DCB group than in the two DES groups. LLL was lower in the LCx ostium in the DES+DCB group than in the two DES groups (p<0.05). The incidence of MACE was similar in the two groups. In a substudy of the HYPER trial, 50 patients with true CBLs were treated with the hybrid strategy (i.e., DES in MV and DCB in SB) suggesting that such a blended/hybrid strategy is a safe and effective alternative to two stents in true CBLs36. A comprehensive overview of the available studies on DCB treatment for CBLs is provided in Table 1, while ongoing clinical trials are reported in Table 2.
Table 1. Randomised clinical trials and registries on the use of DCBs in CBLs.
| Study name, year | Study reference | Design | DCB | Comp | n | Inclusion | DCB treatment strategy | Predilatation, % | Intravascular imaging, % | KBI, % | POT, % | Bailout stenting | Primary endpoint | Angiographic follow-up (p-value)* | MACE (p-value) | TLR (p-value) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DEBIUT, 2012 | NCT00857441 | 1:1:1 RCTOpen-label, superiorityMulticentreCore labCECProvisional TArms:MV DCB+BMS and SB DCBMV BMS+POBA SBMV DES+POBA SB | DIORa | PES | 117 | CCS, UA, ischaemiaDe novo (DS 50-100%)RVD>2.5 mm in MV>2 mm in SB |
Direct DCB dilatation in MV and SB | - | - | 100 | - | 10 vs 5 vs 5 (0.68) | 6M LLL | 6MMV LLL0.58±0.65 vs 0.60±0.65 vs 0.13±0.45 (0.87)SB LLL0.19±0.55 vs 0.21±0.57 vs 0.11±0.43 (0.92)Restenosis 24 vs 28 vs 15 (0.79) | 12M20 vs 29 vs 17 (0.32) | 12M20 vs 27 vs 15 (NS) |
| BABILON, 2014 | NCT01278186 | 1:1 RCTOpen-label, non-inferiorityMulticentreProvisional TArms:MV DCB+BMS and SB DCBMV DES+POBA SB | SeQuent Pleaseb | EES | 108 | CCS, UA, ischaemiaDe novo (DS 50-100%)RVD>3 mm in MV>2 mm in SB |
Direct DCB dilatation in MV and SB | - | - | 26 | - | 7.8 vs 8.9 (1.0) | 6M LLL | 9MMV LLL0.31±0.48 vs 0.16±0.38 (0.15)SB LLL–0.04±0.76 vs 0.03±0.51 (0.98)Restenosis MV/SB: 13/6 vs 1.8/3.6 (0.027/0.67) | 9M17.3 vs 7.1 (0.11) | 9M15.4 vs 3.6 (0.045) |
| PEPCAD V, 2011 { | 46 | Observational, prospectiveDual centrePilotCore labCECSingle arm:MV DCB+BMS and SB DCB | SeQuent Pleaseb | - | 28 | CCS or UA or ischaemiaDe novo (DS >70% or >50% with ischaemia)RVD2.5-3.8 mm in MV2-3.5 mm in SBLesion length <20 mm |
Direct DCB dilatation in MV and SB | - | - | 8 | - | 14.3 | 9M LLL | 9MMV LLL0.38±0.46SB LLL0.21±0.48Restenosis MV/SB: 3.8/7.7 | 9M10.7 | 9M3.8 |
| Herrador, 2013 | 29 | Comparative, observational, non-randomised cohortSingle centreAutonomous QCAProvisional TArms:MV DES and SB DCBMV DES | SeQuent Pleaseb | TAXUSc | 100 | DS >50% in MV and SBRVD>2.5 mm in MV>2.5 mm in SBSB lesion length <10 mm | Direct DCB dilatation in SB | - | 97 (IVUS) | 100 | - | - | 12M LLL | 12MMV LLL0.49±0.6 vs 0.62±0.7 (0.39)SB LLL0.09±0.4 vs 0.4±0.5 (0.01)Restenosis MV/SB: 12/7 vs 18/20 (0.44/0.08) | 12M11 vs 24 (0.76) | 12M12 vs 20 (0.16) |
| DEBSIDE, 2015 | 27 | ObservationalMulticentreCore labCECProvisional TSingle arm:SB predilatation followed by MV DES and KBI and final SB DCB | DANUBIOd | Nile PAXd | 52 | CCS or UA or ischaemiaRVD2.5-3.5 mm in MV2-3 mm in SBSB lesion length <6 mm | DCB final dilatation in SB (after provisional T) | MV 100 SB 80 | - | 80 | - | Excluded | 6M LLL | 6MMV LLL0.54±0.6SB LLL–0.04±0.34Restenosis MV/SB: 0/0 | 6M10 | 6M8 |
| BIOLUX-I, 2015 | 28 | ProspectiveMulticentrePilotSingle arm:DCB dilatation to SB and DES to MV, final KBI with POBA | Pantera Luxe | - | 35 | DS >50%RVD2-4 mm in MV | DCB for SB treatment after predilatation | MV 97 | - | 100 | - | 11.4 | 9M LLL | 9MMV LLL0.28±0.59SB LLL0.10±0.43Restenosis MV/SB: 0/0 | 12M6 | 12M2.9 |
| SARPEDON, 2015 | 30 | Prospective, observational cohortSingle centreAutonomous QCASingle arm:DCB in SB after provisional DES and KBI | Pantera Luxe | - | 58 | De novo DS >50% in MV or SBRVD>2.25 mm in MV>2 mm in SB | - | - | 8.6 (IVUS) | - | - | Excluded | 6M LLL | 6MMV LLL0.21±0.35SB LLL0.09±0.21Restenosis MV/SB: 4/6 | 12M19 | 12M5.2 |
| Schulz, 2014 | 20 | Prospective, observationalSingle centreSingle arm:DCB in SB, MV, SB/MV | SeQuent Pleaseb | - | 39 | De novo after appropriate predilatation with 0.8/1:1 balloon (DS <30% MV, <75% SB)RVDAny | - | 100 | - | - | - | 12.8 | 4M ISR | 4MRestenosis MV/SB: 6.7/3.3 | 4M7.7 | 4M7.7 |
| PEPCAD-BIF, 2016 | 31 | 1:1 RCTProspectiveMulticentreProvisional DESAfter successful predilatation (recoil <30%, diss <C), randomisation toarms:SB DCBSB POBA | SeQuent Pleaseb | POBA | 64 | CCS or UA, ischaemiaDe novo Medina 0,0,1 or 0,1,1RVD2.0-3.5 mm in SBSB lesion length <10 mm | DCB for SB treatment after predilatation | 100 | - | - | - | 0 | 9M LLL | 9MLLL0.13±0.31 vs 0.51±0.66 (0.045)ISR6 vs 26 (0.045) | - | - |
| Okutsu, 2022 | 47 | ObservationalSingle centreDirect coronary atherectomy+DCBLM 59%Autonomous QCA/IVUS/OCT | SeQuent Pleaseb | - | 25 | De novo true CBLs of proximal left coronaryRVD>3 mm in MV>2 mm in SB | - | - | 96 (OCT) | - | - | 5 | In-hospital MACE | 3MLLL0.2±0.6 | 0 | 0 |
| DCA/DCB, 2020 | 48 | Retrospective registryMulticentreDirect coronary atherectomy+DCB in bifurcationLM 81% | SeQuent Pleaseb | - | 129 | Major CBLs (SB >2 mm) suitable for DCA deliveryRVD>2 mm in SB | - | - | - | - | - | - | 12M TVF | 6-15MLLL0.29±0.51ISR2.3 | 12MTVF10.9 | 12M3.1 |
| Study name, year | Study reference | Design | DCB | Comp | n | Inclusion | DCB treatment strategy | Predilatation, % | Intravascular imaging, % | KBI, % | POT, % | Bailout stenting | Primary endpoint | Angiographic follow-up (p-value)* | MACE (p-value) | TLR (p-value) |
| BEYOND, 2020 | 32 | Prospective RCTMulticentreDCB vs POBA in non-LM bifurcations after provisional with DES in MV (1:1 randomisation after predilatation)Arms:SB DCBSB POBA | Bingo PCBf | POBA | 222 | CCS or UA, ischaemia, old MIDe novo CBLs with SB DS >70%, <50% after predilatationRVD1.25-5 mm in SBLesion length <40 mm | DCB for SB treatment after predilatation | MV 93.2 SB 82.9 | - | 100 | - | 0 | 9M DS | 9MDS28.7±18.7 vs 40±19 (0.001 superiority) | 9M0.9 vs 3.7 (0.16) | - |
| Ke et al, 2023 | 23 | RCTSingle centreTrue CBLsArms:DCB-only PCITwo DES | SeQuent Pleaseb | DES | 60 | De novo true CBLs Medina type 1,1,1; 0,1 1; 1,0,1RVD>2.25 mm in SB | DCB-only strategy for true CBLs after predilatation | 100 | - | 63 | - | 0 | 12M LLL | 12MMV LLL0.05±0.24 vs 0.25±0.35(0.013)SB LLL–0.02±0.19 vs 0.11±0.15 (0.005) | 0 | 12M10% |
| SPARTAN-LMS, Gunawardena et al, 2023 | 49 | Retrospective, propensity-matchedSingle centreDCB-only vs DES in LM | SeQuent Pleaseb | DES | 148 | Primary lesion treated in the LM | DCB-only strategy for LM | - | 64.9 (OCT/IVUS) | - | - | 1 | All-cause mortality | - | - | 34M7.3 vs 8.3 (0.86) |
| Uskela et al, 2023 | 50 | RetrospectiveSingle centreSingle arm:DCB-only in LM | Paclitaxel DCB | - | 66 | - | - | - | - | - | - | - | 12M MACE | - | 12M24 | 12M6 |
| Liu et al, 2022 | 51 | RetrospectiveSingle centreLM PCIArms: DES in MV + DCB in SB 2 DES strategy | Bingofpaclitaxel+iohexol matrix | DES | 85 | LM >50% DS | SB DCB (LCx) in the treatment of left main bifurcation lesions | 100 | 28 (IVUS) | 100 | 100 | - | 12M MACE | LLL DES+DCB vs 2DESLM 0.09 vs 0.17 (0.037)LAD 0.16 vs 0.16 (0.385)LCx –0.17 vs 0.43 (0.001) | 12M10 | 12M9 |
| Her et al, 2016 | 22 | ProspectiveSingle centreSingle arm:DCB-only in isolated SB | SeQuent Pleaseb | - | 16 | - | - | - | - | - | - | - | 9M SB ostial lumen area (OCT) | - | - | - |
| Vaquerizo et al, 2016 | 52 | ProspectiveSingle centreSingle arm:DCB-only in isolated SB | DIORa | - | 49 | CCS with ischaemiaDe novo Medina 0,0,1RVD>2 mm in SB | DCB for SB treatment after predilatation | 100 | - | - | - | 14.3 | 12M MACE | 7-8MLLL0.32±0.73 | 12M16 | 12M14 |
| Bruch et al, 2016 | 21 | ProspectiveMulticentreSingle arm:DCB-only vs DCB+BMS | SeQuent Pleaseb | BMS | 127 | CCS and ischaemia, UAAny MedinaRVD>2 mm in SB | DCB treatment after predilatation | MV 86.9SB 73.8 | - | - | - | 46 | 9M TLR | 9MISR4.5 vs 5.5 | 9M6.6 vs 6.1 | 9M4.5 vs 3.6 |
| EASTBOURNE-BIF, 2024 | NCT03085823 | SubstudyProspective, observationalMulticentreSingle arm:DES in MV and DCB in SB or DCB-only | MagicTouchg sirolimus+ phospholipid |
- | 194 | Bifurcation lesion from EASTBOURNE registry | DCB for SB treatment after predilatation | - | - | - | - | 19 | 12M TLR | - | 12M8.8 | 12M4.2 |
| Kasbaoui et al, 2023 | 53 | Prospective, observationalSingle centreSingle arm:DES in MV and DCB in SB | AGENTc paclitaxel+acetyl tributyl citrate | - | 45 | ACS or CCS with ischaemiaDe novo true CBLMedina 1,1,1; 0,1,1RVD2-3.5 mm in SB | DCB for SB treatment after predilatation | - | - | - | - | 11.1 | 6M TLF | 6MISR2.2 | - | 6M2.2 |
| Ikuta et al, 2022 | 54 | Prospective, observationalMulticentreSingle arm:DES in MV and DCB in SB | SeQuent Pleaseb paclitaxel +iobromide |
- | 138 | - | DCB for SB before MV stenting | - | - | - | - | - | 12M ISR | 12MSB LLL–0.14±0.43ISR8 | 12M2.9 | 12M3.6 |
| Pan et al, 2022 | 34 | Retrospective, propensity-matched, observationalSingle centreDES in LM bifurcationArms:Hybrid (DCB + DES) DES-only strategy (provisional stenting or two-stent strategies) |
SeQuent Pleaseb paclitaxel +iobromide |
597 | CCS or UADe novo coronary lesions (diameter stenosis >50%) at the LM bifurcation Medina 1,0,1; 0,1,1; or 1,1,1RVD>2.0 mm in SB | DCB for SB treatment after predilatation | 100 | 43 (IVUS) | 95 | - | 3.5 | 24M TLF | 12MMV LLL0.25±0.48 vs 0.22±0.42 (NS)SB LLL0.13±0.42 vs 0.42±0.62 (0.001) | - | 12M2.9 vs 9.4 (0.007) | |
| Liu et al,2022 | 35 | Retrospective, observationalSingle centreLM PCIArms:DES in MV and DCB in SBTwo DES | Bingof | 2-stent strategy | 100 | True LM bifurcation | DCB for SB treatment after predilatation | 100 | 28 (IVUS) | 100 | - | - | 6M LLL | 6MSB LLL–0.17 vs 0.43 (0.001)SB ISR7 vs 30 (0.093) | 6MNo difference | 6M6 vs 12 (0.485) |
| DCB-BIF, 2025 | 33 | 1:1 RCTOpen-label superiorityMulticentreCore labCECDe novo true CBLsMedina 1,1,1; 0,1,1; or 1,0,1DCB vs POBA for SB in provisional strategy with DES to MVArms:DCBNC balloon POBA | PCB | POBA | 784 | CCS or ACSRVD>2.5 mm in MV>2.5 mm in SBLesion length <10 mm | DCB for SB treatment after predilatation | MV 96.4 SB 18.5 | 27 (OCT/IVUS) | 97 | 86 vs 89 | 3.8 vs 3.3 | 12M MACE | - | 12M7.2 vs 12.5 (0.013) | 12M1.3 vs 1.5 (NS) |
| *LLL given in mm; restenosis and diameter stenosis given as %. aEurocor Tech; bB. Braun; cBoston Scientific; dMinvasys; eBiotronik; fYinyi Biotech; gConcept Medical. ACS: acute coronary syndrome; BMS: bare metal stent; CBL: coronary bifurcation lesion; CCS: chronic coronary syndrome; CEC: clinical events committee; comp: comparator; DCA: direct coronary atherectomy; DCB: drug-coated balloon; DES: drug-eluting stent; diss: dissection; DS: diameter stenosis; EES: everolimus-eluting stent; ISR: in-stent restenosis; IVUS: intravascular ultrasound; KBI: kissing balloon inflation; LAD: left anterior descending coronary artery; LCx: left circumflex coronary artery; LLL: late lumen loss; LM: left main; M: month; MACE: major adverse cardiac events; MI: myocardial infarction; MV: main vessel; NC: non-compliant; NS: non-significant; OCT: optical coherence tomography; PCB: paclitaxel-coated balloon; PCI: percutaneous coronary intervention; PES: paclitaxel-eluting stent; POBA: plain old balloon angioplasty; POT: proximal optimisation technique; QCA: quantitative coronary angiography; RCT: randomised controlled trial; RVD: reference vessel diameter; SB: side branch; TLF: target lesion failure; TLR: target lesion revascularisation; TVF: target vessel failure; UA: unstable angina | ||||||||||||||||
Table 2. Ongoing clinical trials on the use of DCBs in CBLs.
| Identifier (ClinicalTrials.gov) | Status | Study title | Study design | Inclusion criteria | Exclusion criteria | Outcomes | Reference vessel | DCB | DES | Target sample size | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|
| NCT05222061 | Unknown | A Study of Drug Coated Balloon For Treating the Side Branch in Complex Bifurcation Lesions (STENT-FREE) | Prospective, single blinded, randomised (DCB vs balloon) | True bifurcations (1,1,1; 0,1,1; 1,0,1), MV diameter >2.5 mm Ischaemic symptoms, ischaemia | STEMI <72H, cardiogenic shock, CTO, >2 other lesions to be treated, SS <32, LM, ISR, LVEF <30% | 12M LLL for MV and SB 3, 6, 12M MACE, death, ST, ISR, TLR, TVR, angina, angio success (DS residual <30% TIMI 3), fluoroscopy time | MV >2.5 mm | Any | No DES | 80 | 12M |
| NCT04896177 | Recruiting | Sirolimus DCB in Coronary Bifurcation Lesions | Prospective, randomised (sirolimus vs paclitaxel), non-inferiority, open label | De novo bifurcation with SB DS >70%, no expectation to implant stent to SB, no DCB to MV Evidence of ischaemia Residual stenosis <50% in SB after pretreatment and TIMI 3 | Shock, SVHD, haemorrhagic diathesis, STEMI <7D, NYHA IV, HTx, creatinine >3, life expectancy <12M, ISR, LM | 9M DS in target lesion branch Success rate; 9M ISR, LLL; 1, 6, 12, 24M TLR, TVR, TLF | RVD 2.0-4.0 mm | Shenzhen Salubris SCB vs Yinyi Biotech | No DES | 280 | 24M |
| NCT03820622 | Unknown | The Safety and Efficacy of DIOR Balloon in Coronary Bifurcation Lesions (BEYOND-II) | Prospective multicentre, randomised (DIORa vs BINGOb PCB), open label, non-inferiority | Stable/UA, old MI, no contraindication to CABG One or two true bifurcations (1,1,1; 1,0,1; 0,1,1) in different epicardial vessels Residual MV >70% or 50% with symptoms and SB >50% (visual estimation), MV <20% after stent while SB >70% after stent | MI <1W, shock, NYHA III-IV, LVEF <35%, GFR <30 mL/min/1.73 m², haemorrhagic diathesis, PCI or PAD <12M, allergies, life expectancy <12M MV or non-target lesion LM or 3VD, SB is triple bifurcation, MV within 3 mm from ostium, SB disease >26 mm or a stenosis >90% is <5 mm, SB aneurysm, CTO, moderate-severe calcification Residual DS <50% TIMI 3, no angio complications and no dissections type C-F | 9M LLL Device success, clinical success; 1, 6, 9, 12M DOCE, POCE, death, MI, TLR, TVR, LLL of SB, MLD of SB, ABR | SB RVD 2.5-4 mm and length <26 mm | DIORa paclitaxel vs BINGOb paclitaxel | No DES | 220 | 12M |
| NCT04403048 | Not yet recruiting | Drug Coated Balloon for Side Branch Treatment vs. Conventional Approach in True Bifurcation Coronary Disease: PRO-DAVID | Prospective, randomised (standard provisional vs DCB provisional), parallel, open label | CCS, UA, NSTEMI suitable for PCI, in CCS ischaemia De novo bifurcation involving side branch (1,1,1; 1,0,1; 0,1,1), SB RVD ≥2.5 mm and lesion length >5 mm, LM SB DS >70%, non-LM SB DS >90%, SB length ≥73 mm In LAD-D, SnuHscore ≥2 | STEMI <72H, CTO, SS >32, TIA/stroke <6M, LVEF <30%, shock, SVHD, creatinine >2, allergies Thrombus, severe calcification, ostial, graft, CTO, ISR or restenosis <4 mm, previous stent <15 mm from lesion | 12M MACE 12-36M MACE, angiographic success, procedural success, 12M lesion thrombosis, 9M LLL, bailout stenting or inadequate predilatation, fluoroscopy time/dose, contrast, 6-9M rate of lumen gain >20% | SB RVD ≥2.5 mm, SB length >5 mm | Any | Any | 800 | 36M |
| NCT04641468 | Unknown | Clinical Efficacy and Safety of a Prospective, Multicenter Drug Coated Balloon for Left Main Artery Disease in China | Prospective, open label, observational (DCB alone combined with retracted DES if necessary) | De novo lesion with myocardial ischaemia, LM bifurcation 0,1,0; 0,0,1, DS >70% or <30% in distal LM (visual estimation), RVD 2-4 mm | Shock, haemodynamic instability, LVEF <35%, allergies, stents implanted in LM, GFR <30 mL/min/1.73 m², life expectancy <12M | 12M MACE 12M TLR, revascularisation | RVD 2-4mm | Any | Any | 30 | 12M |
| NCT04753827 | Completed | "L-Sandwich" Strategy in the True Coronary Bifurcation Lesions | Prospective, randomised (strategy 1=2 DES bifurcation-culotte/DK crush, 2=DES MV+DCB SB, 3=DES MV, DES SB >5 mm from ostium, DCB ostium), open label, parallel assignment | Bifurcation with SB disease >25 mm | SB <2.5 mm Shock, life expectancy <12M, allergies, severe calcification | 6M LLL (MV or SB) 6M TLF | SB >2.5 mm | Any | Any | 90 | 6M |
| NCT04242134 | Active, not recruiting | Drug-coating Balloon Angioplasties for True Coronary Bifurcation Lesions | Prospective, 1:1 randomised (DCB provisional=NC SB dilatation, DCB dilatation SB, KB with NC, POT vs provisional DES), parallel, single blinded | CCS with ischaemia, UA, MI >7D Bifurcation 0,1,1; 1,0,1; 1,1,1, RVD ≥2.5 mm in MV and SB (visual estimation), DS ≥50%, SB lesion <10 mm, ostium SB DS >70% after stenting | STEMI <7D, allergies, life expectancy <12M, ISR, CTO, severe calcification | 12M MACE 12M all-cause death, CD, MI, TLR/TVR, ST Angiographic success, procedural success, crossover | RVD ≥2.5 MV and SB | Paclitaxel DCB | Any | 784 | 12M |
| NCT04918615 | Active, not recruiting | Compare Sirolimus Coated Balloon Catheter With Paclitaxel Coated Balloon Catheter in De Novo Coronary Bifurcated Lesions (PROMISE-BIF) | Prospective, multicentre, randomised (DCB vs DCB in the treatment of SB in bifurcation) non-inferiority | SB with de novo lesion ≥70% with no expected stent implantation No DCB on main vessel (KB before DCB) Residual stenosis after predilatation ≤30% (TIMI 3) | SB severely calcified and not properly predilated ISR Dissection type ≥C after predilatation/KB or restenosis >30% LVEF <30%, GFR <30 ml/min/1.73 m² | 9M DS% side branch 9M LLL SB, immediate success; 1, 6, 12, 24M DOCE, POCE, TLR, TVR, MI, ST | SB 2.0-4.0 mm; LL ≤40 mm | Sirolimusd vs Paclitaxelb | No DES | 234 | 24M |
| NCT04842838 | Not yet recruiting | Comparative Clinical Study of Drug coating Balloon Strategy and Drug-eluting Stent Strategy (Kissing-DCB) | Prospective, randomised (DCB vs DES), parallel assignment, single blinded | Evidence of ischaemia Bifurcation (1,1,1; 1,0,1; 0,1,1) MV RVD 2.5-4 mm, SB ≥2 mm, MV DS ≥70% and SB ≥50% After predilatation, DS <30%, dissection type A-C | MV or SB require more than one device More than 1 non-target lesion requiring intervention Distance between non-target and target <10 mm LM bifurcation ISR or severe calcification STEMI or NSTEMI <7D Shock, LVEF <35%, GFR <30 mL/min/1.73 m2, allergies | 12M TLF, NACE Technical success, procedural time, 1, 6, 24, 36M TLF, TLR, TVR BARC 2-5, ST | MV RVD 2.5-4 mm, SB RVD ≥2 | Any | Any | 1,000 | 12M |
| NCT03223974 | COMPLETED | Clinical Trial on Safety and Efficacy of Drug-coated Balloon in Treatment of Coronary Bifurcation Lesions (BJDCB-BIF) | Prospective, randomised clinical trial (DCB vs DES) | CCS, UA or MI >7D Bifurcation (0,1,1-1,1,1-1,0,1), MV RVD 2.5-3.5 mm and length <30 mm, SB RVD 2-3 mm and length <22 mm. DS >70% or 50% with ischaemia After predilatation, no dissection type C-F, DS <30%, TIMI 3 Distance with residual stenosis to be treated >10 mm Only one DCB or DES to be used for MV and SB | MI <7D, LVEF <30, NYHA III-IV, SVHD, life expectancy <12M, allergies, severe liver or renal failure, stroke <6M, GI bleeding Thrombosis, graft, CTO, LM or 3VD to treat | 9M LLL 1, 6, 9, 12, 24M DOCE, and ischaemia-driven revascularisation | MV RVD 2.5-3.5 and length <30 mm SB RVD 2-3 and length <22 mm | Any | Any | 80 | 24M |
| NCT01009996 | Withdrawn (funding issues) | Efficacy Study of Kissing Drug-Eluting Balloons in Coronary Bifurcation Lesions (KISSING DEBBIE) | Observational cohort prospective | De novo bifurcation RVD 2.25-4.0 mm | LM, MI <48H | 9M LLL Procedural success, 9M ISR, 3, 6, 9, 12M MACE | RVD 2.25-4.00 mm | Any | Any | - | 12M |
| NCT05731687 | Recruiting | Bifurcation PCI With a Hybrid Strategy With Drug Eluting Balloons Versus a Stepwise Provisional Two-stent Strategy (Hybrid DEB) | Randomised controlled trial and registry | Significant de novo bifurcation lesion (MV and SB diameter ≥2.5 mm, DS of the MV ≥70% and of the SB ≥50% or in intermediate stenosis FFR ≤0.80 or iFR ≤0.89) Stable coronary artery disease or stabilised acute coronary syndrome Age ≥18 years Acceptable candidate for treatment with a DES | Unstable clinical condition Previous PCI with stent implantation in the target lesion(s) Known comorbidity with a life expectancy of <2 years Active bleeding requiring medical attentions (BARC >2 at index PCI) Pregnancy Unable to provide consent for any other reason Participation in another stent or drug trial Known hypersensitivity or allergy to aspirin, clopidogrel, ticagrelor, prasugrel, cobalt chromium, sirolimus, excipients with phospholipid or related origins | Composite of all-cause death, periprocedural or spontaneous MI, TVR Procedural success, MACE, TVF, major bleeding, contrast volume used, probable and definite ST, major intraprocedural complications, radiation exposure, procedural time, procedural costs, percentage of stent expansion in proximal and distal MV and SB, final minimal lumen and stent area after stenting, dissections | MV and SB diameter ≥2.5 mm | Concept Medical | Supraflexe | - | 12M |
| NCT06166459 | Not yet recruiting | Yao Strategy for the Treatment of de Novo Medina 0,1,0 or 0,0,1 Bifurcation Lesion | Single group assignment, open label | Subjects 18-80 years old De novo native lesion, Medina type 0,1,0/0,0,1 bifurcation lesion Reference diameter of the target vessel 2.75-4.00 mm, length <40 mm Subjects willing to participate in the study, sign informed consent form, and accept clinical follow-up | DS of adjacent branch vessel ostium ≥50% STEMI Stents implanted within 10 mm proximal or distal to the target lesion Aneurysm within 10 mm proximal or distal to the target lesion Target vessel distortion or severe calcification lesion, so balloon catheter fails to pass Previous CABG Evidence for extensive thrombus within target vessel Evidence of heart failure by at least one of the following: (a) most recent LVEF ≤35%, or (b) current heart failure defined as dyspnoea at rest (NYHA Class IV assessed day of procedure), or (c) Killip class ≥2 (post-STEMI patients) Life expectancy of ≤1 year Stroke, peptic ulcer, or gastrointestinal bleeding within the past 6 months Severe renal failure (eGFR <30 ml/min/1.73 m2), failure to comply with angiography conditions Intolerance to aspirin and/or clopidogrel or ticagrelor or has contraindications Intolerance or allergy to heparin, contrast agent Patients participating in the clinical trial of another drug or device without reaching the time limit of primary endpoint Not applicable to be enrolled by investigators due to other reasons | 9M LLL 12M MACE | Diameter of the target vessel 2.75-4.00 mm, length <40 mm | Any | Any | 200 | 12M |
| NCT06045039 | Recruiting | Clinical Efficacy of Stent-balloon-stent (SBS) Technique in the Treatment of Coronary Bifurcation Lesions | Prospective, cohort | Myocardial ischaemia, such as coronary angiography, including patients with stable angina pectoris, unstable angina pectoris, asymptomatic myocardial ischaemia and acute MI (>24 hours). All bifurcation lesions Medina 1,1,1 or 0,1,1 with an RVD in the SB ≥2.5 mm by visual estimation and had to meet DEFINITION criteria of complex bifurcations Tolerate long-term antiplatelet therapy | Severe surgical contraindications Life expectancy <12M Previously undergone stent implantation or surgical CABG for related lesions Severe hepatorenal insufficiency Heart failure patients with NYHA Class ≥III Scheduled for surgery requiring antiplatelet medication interruption within 6 months Need for chronic oral anticoagulation Any clinical condition that may interfere with medication compliance or long-term follow-up Pregnant or breastfeeding women | Target lesion failure rate Cardiac death 3-12M TVMI 6-12M Clinically driven TLR 6-12M Minimum lumen area and lumen stenosis rate 6-12M | RVD in the SB ≥2.5 mm | Any | - | 200 | 12M |
| NCT02276846 | Unknown | Palpitate-Eluting Balloon Angioplasty in the Treatment of Coronary Bifurcation Lesion Evaluated by OCT (PEBCBLO) | Prospective, observational (efficacy of PCB SeQuent Pleasec in SB after MV treatment with EXCEL stent) | CCS or UA or documented ischaemia De novo bifurcation with DS >70% in both branches or >50% if ischaemia | MI <48H, NYHA IV, shock, SVHD, life expectancy <12M, stroke <6M, GFR <30 mL/min/1.73 m², post-transplantation, thrombus, multilesion treatment outside bifurcation Previous stent <15 mm lesion, DES <9M/BMS <3M, graft, CTO, ISR, allergies | 9M LLL 9M MACE, procedural success | LAD/LCx RVD 2.5-4.0 mm, length <30 mm D1/D2 OM RVD 2.0-3.5 mm, length <30 mm | SeQuent Neoc | EXCELf | 30 | 9M |
| aBy Eurocor Tech; bby Yinyi Biotech; cby B. Braun; dby MicroPort; eby SMT; fby JW Medical Systems. 3VD: three-vessel disease; ABR: angiographic binary restenosis; BARC: Bleeding Academic Research Consortium; BMS: bare metal stent; CABG: coronary artery bypass graft surgery; CBL: coronary bifurcation lesion; CCS: chronic coronary syndrome; CD: cardiovascular death; CTO: chronic total occlusion; D: day; D1: first diagonal branch; D2: second diagonal branch; DCB: drug-coated balloon; DEB: drug-eluting balloon; DES: drug-eluting stent; DOCE: device-oriented composite endpoint; DS: diameter stenosis; eGFR: estimated glomerular filtration rate; FFR: fractional flow reserve; GFR: glomerular filtration rate; GI: gastrointestinal; HTx: heart transplantation; iFR: instantaneous wave-free ratio; ISR: in-stent restenosis; KB: kissing balloon; LAD: left anterior descending artery; LCx: left circumflex artery; LLL: late lumen loss; LM: left main; LVEF: left ventricular ejection fraction; M: month; MACE: major adverse cardiovascular events; MI: myocardial infarction; MLD: minimal lumen diameter; MV: main vessel; NACE: net adverse clinical events; NC: non-compliant; NSTEMI: non-ST-elevation myocardial infarction; NYHA: New York Heart Association; OCT: optical coherence tomography; OM: obtuse marginal; PAD: peripheral artery disease; PCI: percutaneous coronary intervention; POCE: patient-oriented composite endpoint; POT: proximal optimisation technique; RVD: reference vessel diameter; SB: side branch; SCB: sirolimus-coated balloon; SNuH: size, number, highest; SS: SYNTAX score. ST: stent thrombosis; STEMI: ST-segment elevation myocardial infarction; SVHD: single ventricle heart disease; TIA: transient ischaemic attack; TIMI: Thrombolysis in Myocardial Infarction; TLF: target lesion failure; TLR: target lesion revascularisation; TVF: target vessel failure; TVMI: target vessel myocardial infarction; TVR: target vessel revascularisation; UA: unstable angina; W: week | |||||||||||
Specific subsettings
Acute coronary syndromes
Preliminary data suggest that a DCB-only strategy may be feasible and safe in selected patients with acute coronary syndromes (ACS). Subgroup analyses of large trials and observational registries have shown that, when used after proper lesion preparation, DCBs yield comparable outcomes to DES37. In bifurcation settings, DCB use has mainly involved the MV, with limited data specifically addressing SB treatment. Given the potential issues related to thrombus burden and drug delivery, further research is needed to define the optimal use of DCBs in bifurcated lesions during ACS.
Diabetes mellitus
Diabetic patients often present with complex, diffuse disease and higher restenosis risk, especially in small vessels and bifurcations. Although no RCTs have specifically investigated DCB use in bifurcation PCI in diabetic patients, the stent-sparing nature of DCBs and their favourable outcomes in small vessels suggest they could be beneficial in this high-risk population. Dedicated studies are needed to confirm this hypothesis.
High bleeding risk
DCB-based strategies are particularly appealing in HBR patients due to the potential for stent-free revascularisation and DAPT de-escalation3839. In bifurcation lesions, using DCBs in the SB or within hybrid strategies can help minimise stent length and reduce the bleeding risk associated with prolonged DAPT. Observational data and the recent REC-CAGEFREE II trial40 support the safety of abbreviated antiplatelet regimens following DCB treatment, although their applicability specifically to bifurcated anatomy remains to be fully validated.
Intracoronary imaging and physiology for DCB-based PCI in CBLs
Intracoronary imaging (ICI) provides a more detailed assessment of vessel size, plaque composition, morphology, and characteristics, thereby enabling optimised lesion preparation, as compared to angiography alone. Although current guidelines recommend the use of ICI (Class I, Level of Evidence A recommendation) in complex DES-based PCI41, its role in DCB PCI has been underevaluated until recently. OCT is often preferred because of its high resolution, especially in detecting subtle dissections, thrombus, or incomplete lesion preparation, while IVUS allows for accurate measurement of the vessel wall and plaque burden4. The ULTIMATE III trial recently demonstrated improved angiographic outcomes with IVUS-guided DCB PCI compared to angiographic guidance alone, resulting in improved acute gain and reduced 7-month LLL (–0.10±0.34 mm vs 0.03±0.52 mm; p=0.025) and improved minimal lumen diameter and diameter stenosis42. Furthermore, recent evidence suggests that medial dissections are needed for better outcomes after DCB-only PCI, probably due to the effect of dissection per se on vascular remodelling and because they might facilitate better drug transfer to the vessel wall43. In the setting of CBLs, intracoronary imaging and coronary physiology can assist in refining the Medina classification and in guiding the decision to perform bailout stenting when residual stenosis or angiographic dissections are present. Although specific thresholds (e.g., minimal lumen area or dissection severity) for bailout stenting after DCB treatment are yet to be established, ICI can provide valuable guidance in borderline or ambiguous cases. SB ostial narrowing frequently appears to be angiographically significant after MV stenting, yet functional assessment often shows no ischaemia. Physiological tools such as FFR or non-hyperaemic pressure ratios (NHPRs) can help identify functionally non-significant lesions and support SB deferral. In a pivotal study by Koo et al, FFR assessment of jailed SB lesions following MV stenting revealed that many angiographically significant stenoses were not haemodynamically relevant, thus supporting a physiology-guided approach to avoid unnecessary interventions44. To date, no prospective, dedicated clinical studies have assessed the role of invasive, pressure wire or angiography-based coronary physiology in guiding DCB treatment. Retrospective observational data suggest that a distal coronary-to-aortic pressure ratio (Pd/Pa) cutoff value of 0.90 may indicate optimal lesion preparation prior to DCB application45.
Conclusions
The use of DCBs for SB treatment of coronary bifurcation lesions is a novel approach, allowing for a reduction in the overall stent burden and fulfiling a provisional approach to CBLs (Central illustration). The blended/hybrid approach, which combines DCBs with DES, has demonstrated promising results in observational and randomised studies. Additionally, the “DCB-only strategy” has proven to be both feasible and safe for SB-only CBLs. DCB treatment appears to be more efficient than POBA to prevent restenosis in the SB. However, it is important to note that, so far, RCTs have used heterogeneous study protocols and techniques, methods, and devices, have rarely included true CBLs, and have been small in terms of sample sizes. 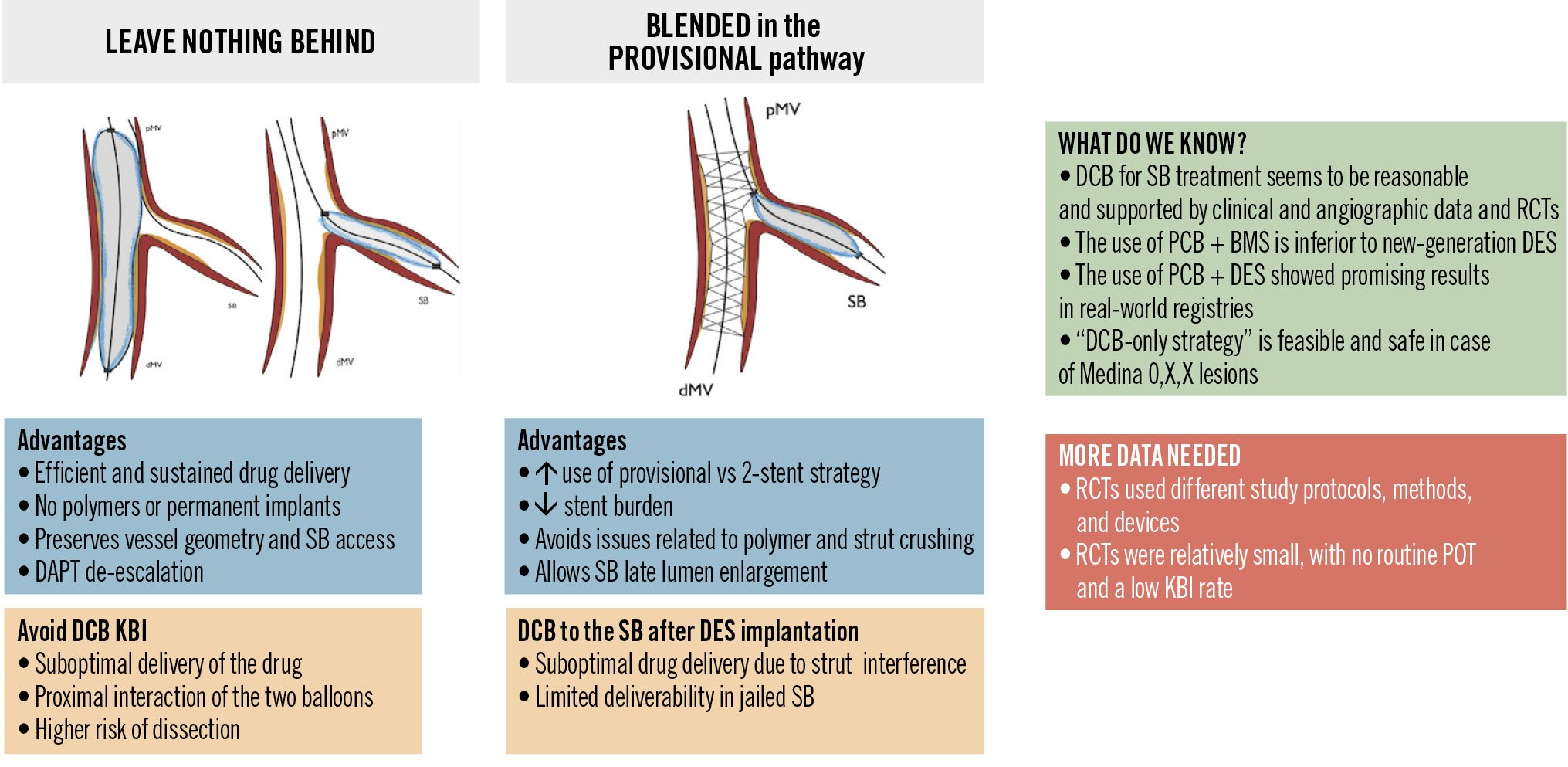
Central illustration. Drug-coated balloons for coronary bifurcation lesions: techniques, advantages, pitfalls, and state-of-the-art. BMS: bare metal stent; DCB: drug-coated balloon; DES: drug-eluting stent; dMV: distal main vessel; KBI: kissing balloon inflation; PCB: paclitaxel-coated balloon; pMV: proximal main vessel; POT: proximal optimisation technique; RCT: randomised controlled trial; SB: side branch
Conflict of interest statement
B. Scheller is a shareholder of InnoRa GmbH. A. Banning reports speaker fees from Abbott; and received a research grant from Boston Scientific. F. Ribichini reports research grants from Philips and Abbott. R. Scarsini reports speaker fees from Abbott; and research grants from Philips and Abbott. S. Fezzi reports consultancy fees from Boston Scientific, Teleflex, and Shockwave Medical. T. Rissanen reports consultancy fees from Boston Scientific, Abbott Laboratories, Cordis, Biotronik, and B. Braun. The other authors have no relevant conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.