Abstract
Background: The influence of age-dependent changes on fractional flow reserve (FFR) or instantaneous wave-free ratio (iFR) and the response to pharmacological hyperaemia has not been investigated.
Aims: We investigated the impact of age on these indices.
Methods: This is a post hoc analysis of the ADVISE II trial, including a total of 690 pressure recordings (in 591 patients). Age-dependent correlations with FFR and iFR were calculated and adjusted for stenosis severity. Patients were stratified into three age terciles. The hyperaemic response to adenosine, calculated as the difference between resting and hyperaemic pressure ratios, and the prevalence of FFR-iFR discordance were assessed.
Results: Age correlated positively with FFR (r=0.08, 95% CI: 0.01 to 0.15, p=0.015), but not with iFR (r=–0.03, 95% CI: –0.11 to 0.04, p=0.411). The hyperaemic response to adenosine decreased with patient age (0.12±0.07, 0.11±0.06, 0.09±0.05, for the 1st [33-58 years], 2nd [59-69 years] and 3rd [70-94 years] age tertiles, respectively, p<0.001) and showed significant correlation with age (r=–0.14, 95% CI: –0.21 to –0.06, p<0.001). The proportion of patients with FFR ≤0.80+iFR >0.89 discordance doubled in the first age tercile (14.1% vs 7.1% vs 7.0%, p=0.005).
Conclusions: The hyperaemic response of the microcirculation to adenosine administration is age dependent. FFR values increase with patient age, while iFR values remain constant across the age spectrum. These findings contribute to explaining differences observed in functional stenosis classification with hyperaemic and non-hyperaemic coronary indices.
Introduction
As a result of shifting demographics, the proportion of elderly patients in whom coronary revascularisation is considered has increased considerably over the last two decades. Currently, both fractional flow reserve (FFR) and instantaneous wave-free ratio (iFR) are recommended by societal guidelines to manage percutaneous coronary interventions (PCI). However, there is growing evidence that the boundary conditions for these pressure-derived measurements are not similar between young and old individuals: experimental coronary perfusion studies found that ageing induces several structural and functional changes in the microcirculatory and epicardial domains, as shown by important differences in hyperaemic flow and myocardial perfusion reserve after vasodilator administration1,2. Furthermore, recent research has shown the fundamental role of microcirculation homeostasis in the vasodilatory response to pharmacological hyperaemia3,4.
Of note, the influence of patient age on invasive functional coronary physiology has yet to be addressed. The purpose of our study was to investigate the impact of ageing in pressure-derived coronary physiology indices with focus on hyperaemic and non-hyperaemic indices and to address its influence on FFR and iFR binary classification discordance.
Methods
STUDY POPULATION
This is a post hoc analysis of the ADVISE II study, a prospective, international, multicentre, controlled, core laboratory-based study of 591 patients and 690 lesions, that aimed to assess the diagnostic value of iFR to characterise, without pharmacologically induced hyperaemia, coronary stenosis severity as determined by FFR5. Briefly, this trial enrolled patients with stable angina or acute coronary syndromes (ACS) who had coronary stenosis (at least 40% diameter lesion by visual assessment) in one or more major epicardial vessels or its branches, suitable for PCI. In patients with ACS, only non-infarct-related vessels were interrogated during the first 48 hours following admission. The detailed inclusion and exclusion criteria were provided in a Supplementary Appendix published along with the original study5. A list of ADVISE II investigators and participating centres is provided in Supplementary Appendix 1. The study protocol was reviewed and approved by the local ethics committees.
INTRACORONARY PHYSIOLOGY
Patients underwent wire-based recordings of aortic (Pa) and intracoronary distal (Pd) pressures. FFR was obtained and calculated after inducing hyperaemia with intravenous adenosine perfusion at 140 mcg/kg/min for a minimum of two minutes. Haemodynamic severity was defined as FFR ≤0.80. All the pressure recordings were analysed by an independent core laboratory and iFR was calculated as the Pd/Pa ratio before hyperaemia induction in the time period between 25% into diastole and 5 ms before diastole ending.
RELATIONSHIP BETWEEN AGE AND PRESSURE-DERIVED INDICES
Patients were stratified into three groups based on age terciles. All correlations between intracoronary physiology indices and age were addressed. The respective prevalence of FFR-iFR discordance, defined as FFR ≤0.80+iFR>0.89 and FFR >0.80+iFR ≤0.89, were calculated and compared between groups. The difference between resting Pd/Pa and FFR was used as an indicator of the vasodilator reserve within each age tercile.
STATISTICAL ANALYSIS
Continuous variables with normal distribution were expressed as mean and standard deviation. Categorical variables were expressed as absolute counts and respective percentages. The 95% confidence intervals (CIs) of the means of continuous variables and percentages of categorical variables were calculated with t-tests and Clopper-Pearson (exact) approaches, respectively. Correlations between coronary physiology indices and age were adjusted for several potential confounders, including visual lesion severity, interrogated target vessel with proximal left anterior descending (LAD) artery lesion, presence of hypertension, diabetes, renal failure, number of vessels interrogated per patient and patients presenting with an ACS. The t-test was used to compare variables with normal. The one-way ANOVA test and Tukey’s post hoc analysis were used to compare mean FFR and iFR values, and the chi-square test was used to compare prevalences between different groups. Logistic regression analysis was applied to relate a broad range of admission parameters to predict FFR-iFR discordance. Generalised estimating equations (GEE) were then used to correct for possible unknown effects between more than one vessel interrogated per patient. Statistical analysis was performed using commercially available software (SPSS, Version 23.0 [IBM Corp., Armonk, NY, USA] and Stata 13.2 [StataCorp, College Station, TX, USA]). Statistical significance was defined as a bilateral p-value <0.05.
Results
STUDY POPULATION
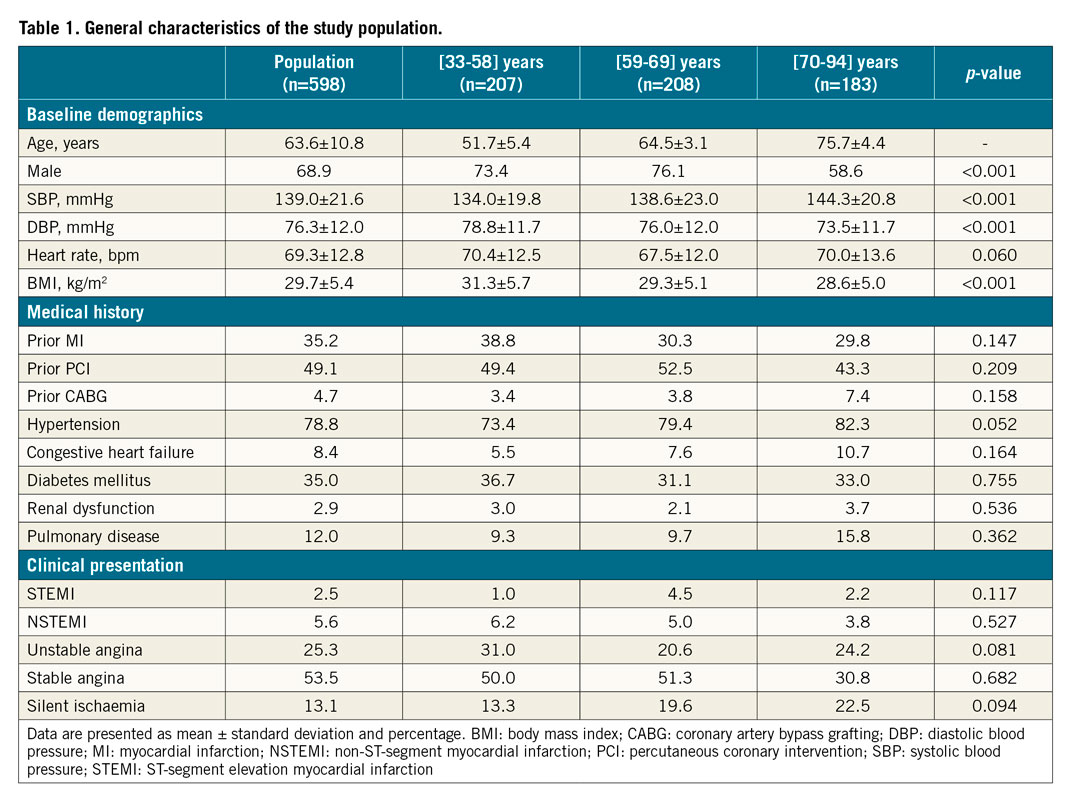
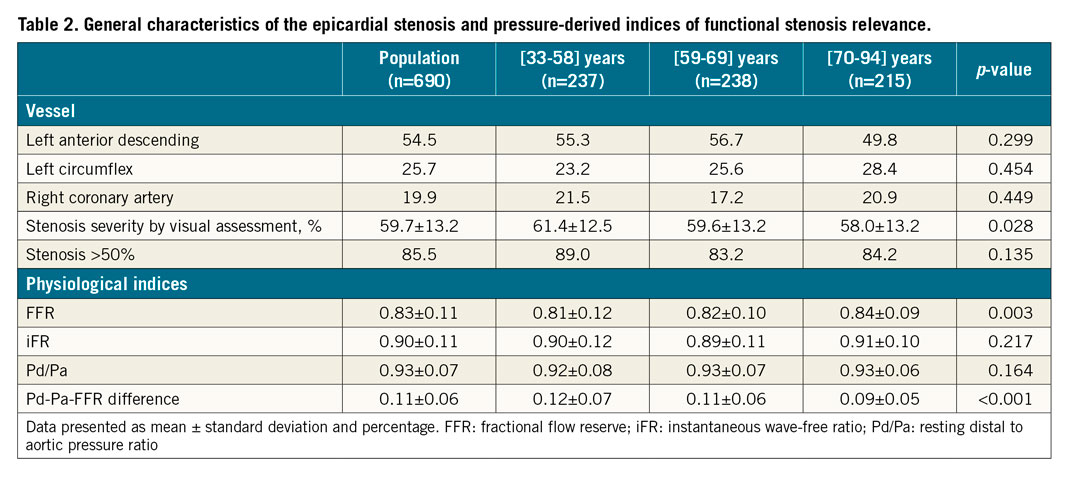
Clinical and angiographic characteristics of the study population are shown in Table 1. Stratification of the total population into terciles of age resulted in the following groups – 1st tercile: 33-58 years; 2nd tercile: 59-69 years; and 3rd tercile: 70-94 years. Importantly, there were no significant differences among the groups regarding the interrogated coronary artery. However, stenosis severity by visual assessment was significantly lower in older patients (61.4±12.5% vs 59.6±14.8% vs 50.8±12.8%, respectively, for the 1st, 2nd and 3rd age terciles; p=0.028) (Table 2).
HAEMODYNAMIC PARAMETERS
The interrogated vessel population (n=690) comprised intermediate angiographic (diameter stenosis by visual assessment: 59.7±13.2%) and physiological severity (FFR 0.83±0.11 and iFR 0.90±0.11), representing the most frequent scenario in everyday practice when using FFR and iFR, namely for establishing the functional relevance of intermediate coronary stenoses. A good linear correlation between both indices was found in the total population (r=0.81, 95% CI: 0.78 to 0.83, p<0.001). The linear regressions for FFR and iFR are presented in Supplementary Table 1. Globally, FFR and iFR results were discordant in 121 (17.5%) lesions, including 67 (9.7%) lesions with an FFR ≤0.80+iFR >0.89 and 54 (7.8% lesions with an FFR >0.80+iFR ≤0.89 (Table 2).
EFFECT OF AGE ON PRESSURE-BASED FUNCTIONAL INDICES
We found a weak positive correlation between age and FFR values (r=0.08, 95% CI: 0.01 to 0.15, p=0.015) (Figure 1A), but not with iFR (r= –0.03, 95% CI: –0.11 to 0.04, p=0.411) (Figure 1B). A significant increase in FFR values was noted in patients older than 70 years (p=0.003), while mean iFR values did not differ significantly between age terciles (p=0.217) (Table 2). The Central illustration shows the agreement/discordance relationship between FFR and iFR, in terms of functional stenosis relevance, per age stratum. The first tercile had a twofold increase in the prevalence of discordance due to abnormal FFR (14.8% vs 7.1% vs 7.0%, for the 1st, 2nd and 3rd terciles, respectively; p=0.005) (Table 2). Interestingly, no significant differences were noted in the prevalence of discordance due to abnormal iFR across the three age groups, although a non-significant trend towards increment with age was noted (5.5% vs 8.1% vs 10.2%, for the 1st, 2nd and 3rd terciles, respectively; p=0.171) (Table 2, Supplementary Figure 1, Supplementary Figure 2). This relationship persisted even when considering only “grey-zone” iFR values (0.86-0.93) (Supplementary Table 2, Supplementary Figure 3).
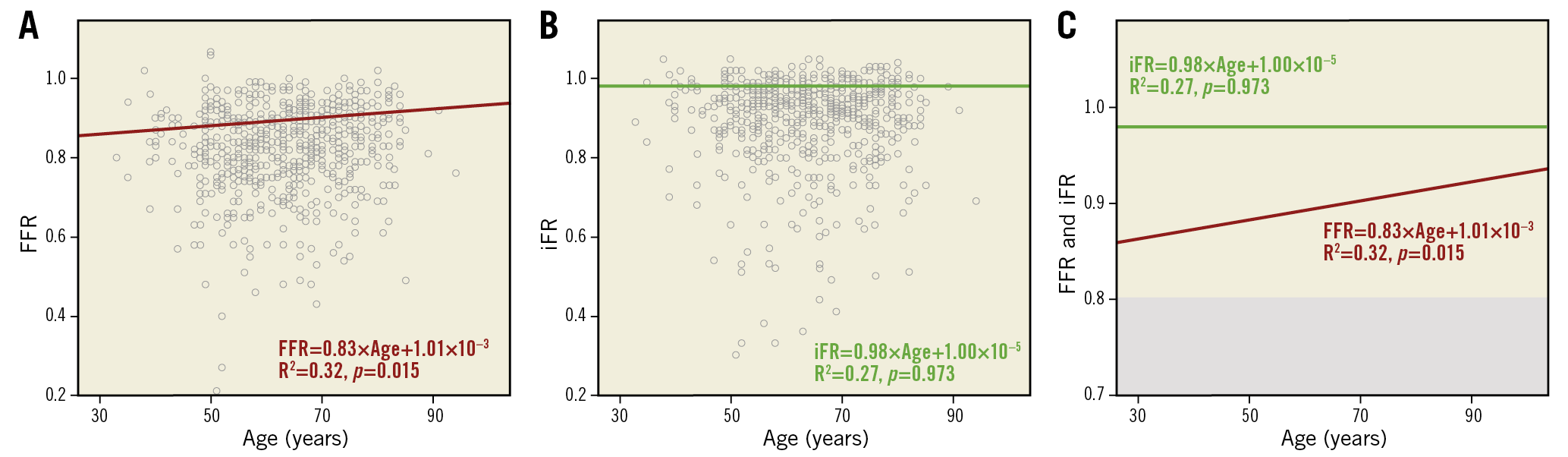
Figure 1. Age correlation with physiologic pressure indices. A) Age correlation with FFR. B) Age correlation with iFR. C) Combined regression lines from panels A and B.
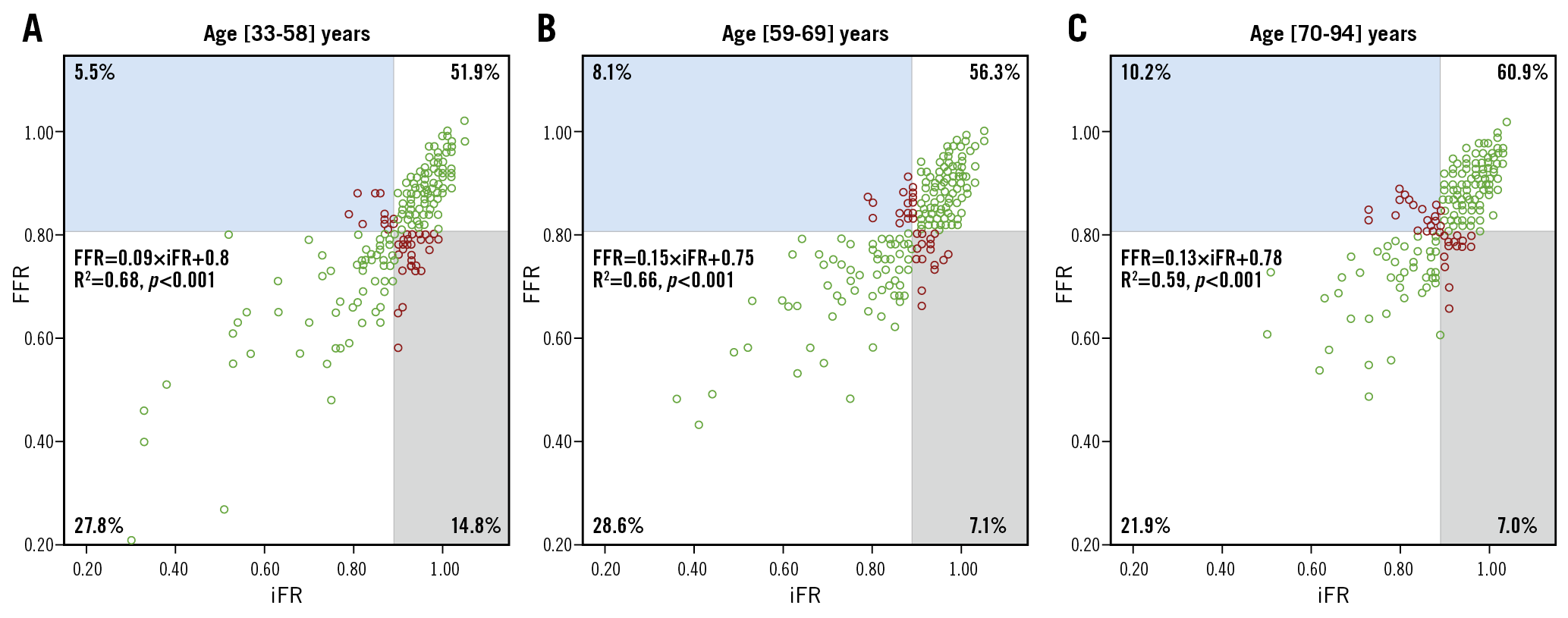
Central illustration. Concordant and discordant FFR and iFR groups in terms of functional stenosis classification and according to age tertiles. FFR-iFR scatter plots for each age stratum. A) [33-58] years. B) [59-69] years. C) [70-94] years. Percentages of cases in concordant (white) and discordant (grey and blue) groups are shown as figures within each quadrant. Discordant values are shown as red circles.
AGEING AND HYPERAEMIC RESPONSES TO ADENOSINE ADMINISTRATION
We used the difference between resting Pd/Pa and FFR as an index of the hyperaemic response to adenosine, or hyperaemic reserve, within each age tercile. A significant decrease in the hyperaemic response to adenosine with age was noted (0.12±0.07 vs 0.11±0.06 vs 0.09±0.05, for the 1st, 2nd and 3rd terciles, respectively, p<0.001). The difference between resting Pd/Pa and FFR showed a significant negative correlation with age (r= –0.14, 95% CI: –0.21 to –0.06, p<0.001), while resting Pd/Pa did not (r= –0.02, 95% CI: –0.09 to 0.06, p=0.662). This relationship was independent of visual stenosis severity (Supplementary Figure 4, Supplementary Figure 5). Figure 2 is a combined graph showing the age-associated decrease in vasodilatory response overlapped with the percentage of discordant FFR/iFR cases due to abnormal FFR values, suggesting a potential mechanism of differences in adenosine response for the observed age-related discrepancy between both indices. A similar representation regarding discordance due to abnormal iFR is provided in Supplementary Figure 1-Supplementary Figure 3.
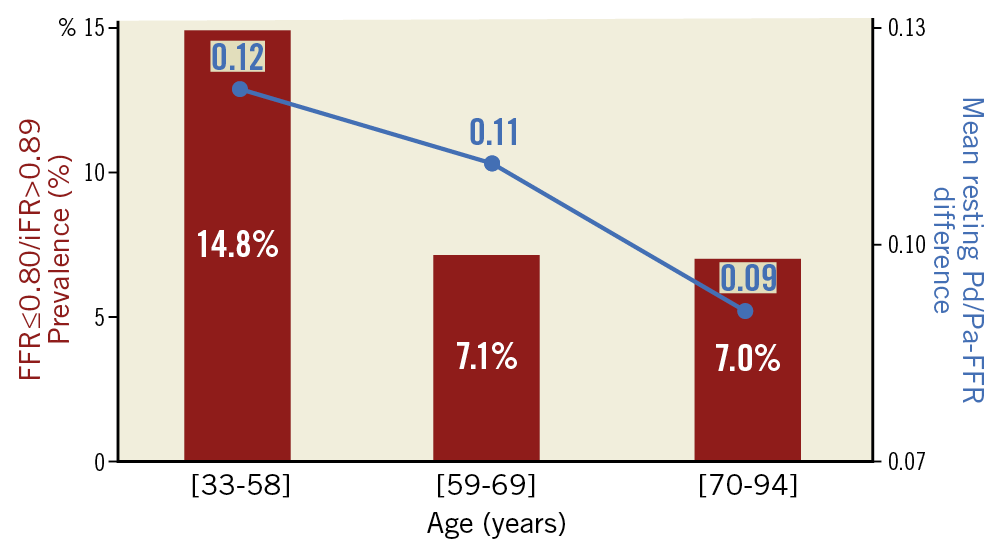
Figure 2. Relationship between FFR-iFR discordance, vasodilatory response to adenosine and patient age. For each age tertile, the proportion of cases with FFR ≤0.80+iFR >0.89 values (red columns), combined with the difference between resting Pd/Pa and FFR (blue dots interconnected with blue lines), the latter serving as a metric of the vasodilatory response to adenosine.
FACTORS INFLUENCING FFR-iFR DISCORDANCE
The results from the univariate analysis and GEE binary logistic model to identify predictors of discrepancy between dichotomous FFR and iFR classification (FFR ≤0.80+iFR >0.89 and FFR >0.80+iFR ≤0.89), presented in Supplementary Table 3-Supplementary Table 5, indicate a significant and independent association between younger age (OR 0.97, 95% CI: 0.95-0.99, p=0.016) and FFR ≤0.80+iFR >0.89 discordance, despite the increased visual lesion severity in this group (OR 1.03, 95% CI: 1.01-1.05, p=0.001). Figure 3 illustrates the marginal effects plots of age on the probability of both types of FFR-iFR discordance adjusted for epicardial coronary stenosis severity, showing that the probability of discordance due to abnormal FFR increases as age decreases. Conversely, the probability of discordance due to abnormal iFR increases with increasing age, thus showing that, under the same epicardial stenosis severity, age is a major determinant of discordance between hyperaemic and non-hyperaemic indices.
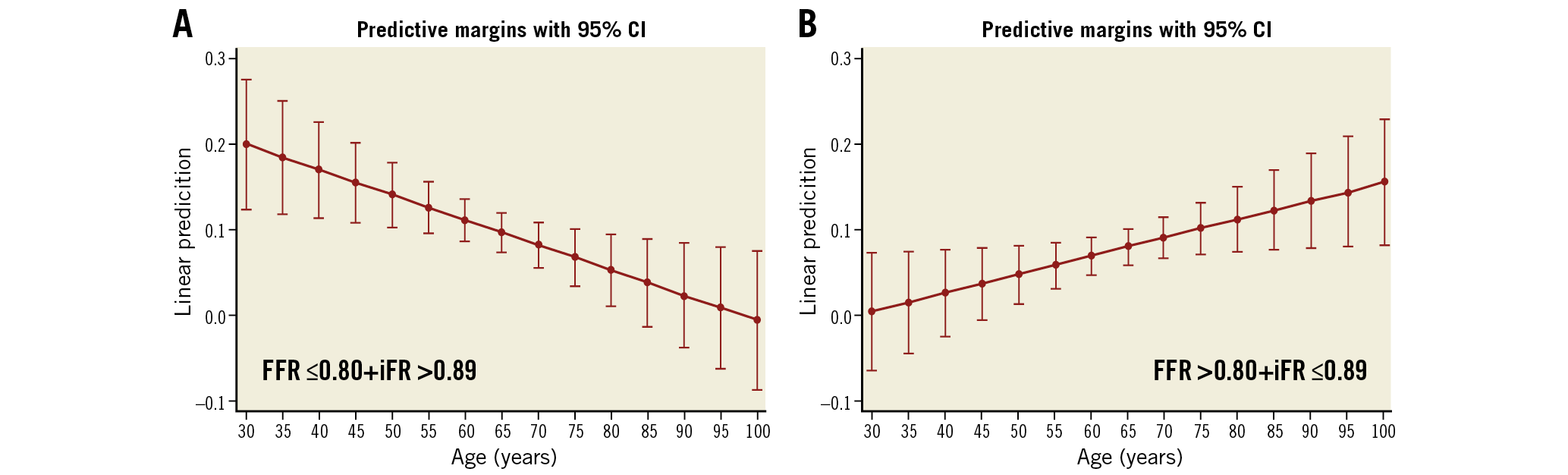
Figure 3. Marginal effects plots of age and type of FFR-iFR discordance with 95% confidence intervals. A) Results for the FFR ≤0.80+iFR >0.89 group. B) Results for the FFR >0.80+iFR ≤0.89 group.
Discussion
Our findings suggest that older age is associated with a significant increase in FFR values, which appears to be linked to a decreased hyperaemic response to adenosine administration. Conversely, iFR values are not influenced by patient age, presumably due to its non-hyperaemic nature. These findings have potential implications in the interpretation of the results of hyperaemic and non-hyperaemic pressure indices in different age strata.
As a result of shifting patient demographics, the reported mean ages in contemporary trials using intracoronary physiology are, on average, more than five years higher than in the pivotal DEFER trial6. As this demographic trend is likely to continue, and since there is a paucity of data on the effect of ageing on physiological indices used routinely in clinical practice, we focused our research on the influence of age on the values of both hyperaemic and non-hyperaemic indices of functional stenosis severity.
We hypothesise that the age-FFR dependency phenomenon is largely caused by an age-related impairment of the vasodilatory capacity of the coronary microcirculation. Ageing induces structural and functional changes in the microcirculation that may explain the diminishing pharmacological hyperaemic response in older subjects3,7,8,9,10, with baseline and hyperaemic myocardial blood flow remaining unchanged up to 60 years of age, but decreasing sharply beyond that age1,2. The age-related patterns of atherosclerosis accounting for differences in coronary haemorrheology are another potential contributing mechanism11. On average, focal stenoses and thin-cap fibroatheromas are more frequent in younger individuals, while diffuse narrowing and vessel calcification occur more frequently in the elderly. As pressure loss due to turbulence or flow separation increases during hyperaemia12, differences in stenosis geometry related with ageing might also contribute to our findings, with focal stenosis generating larger translesional pressure gradients during hyperaemia than diffuse stenoses. In that regard, non-hyperaemic indices might reflect in a more balanced way the contribution of friction and turbulence to flow energy loss in stenotic vessels in the elderly. This hypothesis is supported by the influence of focal and diffuse patterns of epicardial disease on the discrepancy between FFR and iFR values13. Finally, a third mechanism might be that the hyperaemic effect of adenosine on the coronary microcirculation varies with age, as a consequence of age-related changes in cardiac adenosine receptor expression or sympathetic drive14,15,16.
Age also modifies the relative contribution of epicardial stenoses and microcirculatory disease to abnormal coronary haemodynamics in patients with atherosclerotic disease3. A decrease in the proportion of patients with abnormal FFR and normal CFR values with ageing was found. Mirroring that finding, we now describe a decrease in the proportion of patients with an abnormal FFR despite a normal iFR with increasing age. Other authors have previously identified age as one of the factors associated with FFR-iFR discrepancy, although a detailed analysis of the relationship between ageing and such a discrepancy was not performed17,18. In this regard, we used the resting Pd/Pa-FFR difference as a surrogate for vasodilator reserve and microcirculation function since other, better, dedicated indices, such as hyperaemic microvascular resistance or index of microcirculatory resistance, were not performed in the ADVISE II trial. Interestingly, a sub-analysis of the FAME trial documented that higher FFR values occurred in patients >65 years old19.
An explanation of why flow- and iFR-based correlations with FFR resemble each other can be found in previous studies showing that iFR correlates better with flow indices than FFR, from the standpoint either of intracoronary Doppler measurements20, or of 13N-ammonia positron emission tomography21. These findings are also supported by a previous work from our group investigating dichotomous classification of stenosis severity based on FFR and Pd/Pa, in which patients with abnormal FFR but non-ischaemic Pd/Pa values (defined as Pd/Pa >0.91) were significantly younger than any of the other three groups generated by dichotomous classification of both indices22.
The clinical implications of all the points discussed above trigger the important question of whether revascularisation is required in younger patients with stenoses showing an FFR ≤0.80 with non-ischaemic iFR values. Flow-based studies have shown that, on average, myocardial blood supply was preserved in patients with discordant FFR/iFR due to abnormal FFR value and, therefore, iFR values may reflect better the need for revascularisation in the younger age stratum that has a higher prevalence of this type of discordance between FFR and iFR. A patient-pooled analysis of two large randomised trials has shown that, indeed, revascularisation is more frequent when FFR is used in decision making, compared with iFR23. We can hypothesise that the higher rate of revascularisation deferral with iFR was related to the findings of our investigation. More research will be needed to understand the clinical implications of these findings, as evidence addressing this key aspect is lacking. For example, a stratified analysis of the FAME trial did not show a statistically significant difference in events between FFR-guided and angio-guided revascularisation for patients >65 years or ≤65 years; however, no firm conclusions can be drawn due to lack of statistical power and the lack of a comparator iFR arm19.
Overall, the clinical consequences of the discussed dependence of FFR on patient age might result either from an excess of unneeded PCI procedures, or from omission of revascularisation in large myocardial territories. Current clinical practice guidelines recommend both FFR and iFR in routine clinical practice, a fact that is tied to decision making on revascularisation in millions of patients worldwide. As reported previously, the overall effect of age in FFR is small (approximately 1%)24. However, as its contribution to FFR-iFR discrepancy is clinically significant, we strongly believe that further investigations on this phenomenon should be undertaken to optimise the benefits of physiology-guided revascularisation.
Limitations
Our study is limited in that it is a retrospective subgroup analysis of the ADVISE II study. Therefore, our conclusions are mainly hypothesis-generating rather than hypothesis testing. Nevertheless, there was a clear biological and clinical rationale for performing this analysis, as the microcirculatory and epicardial modifications associated with age had been described previously. Another limitation might be lack of invasive coronary flow data, which would explain the differences in coronary flow and vasodilatory capacity such as resistive reserve ratio across age.
Conclusions
Ageing is associated with a lower vasodilatory response of the microcirculation to adenosine administration, causing age-related modification of FFR values that is not observed with iFR. This fact influences the degree of concordance between hyperaemic and non-hyperaemic indices in terms of functional stenosis classification. Further research is needed to clarify the adenosine responses in different age groups.
|
Impact on daily practice FFR values increase with age and this appears to be associated with an age-related decrease in the hyperaemic response of the microcirculation to adenosine. iFR values are not influenced by patient age. The discrepancy between FFR and iFR in terms of stenosis classification is age-related. |
Funding
The ADVISE II study was funded by Volcano Corporation and all analysis was independently performed by the core laboratory (Cardialysis). The authors of this study are solely responsible for the design and conduct, all analysis, manuscript drafting and editing, and are responsible for its final contents.
Conflict of interest statement
J.M. Lee has received a research grant from Abbott Vascular and Philips Volcano. T. van de Hoef is a consultant for Philips. J. Davies holds IP pertaining to iFR technology and is also a consultant and recipient of research funding from Philips Volcano. P. Serruys has received consulting fees from Abbott and Philips. M. Echavarria-Pinto has received speaker fees from Boston Scientific. S. Baptista has received personal fees from Abbott, Boston Scientific, and HeartFlow. H. Samady was a consultant and participated in steering committees for studies sponsored by Philips Volcano and Abbott Vascular, has received institutional grants from Medtronic, Philips and Abbott Vascular, and is also a shareholder in Covanos Inc and SIG. A. Lerman serves as a consultant to Philips Volcano. H. Mejía-Renteria served as speaker at educational events organised by Abbott, Boston Scientific and Philips Healthcare. J. Escaned has served as consultant and speaker at educational events organised by Abbott and Boston Scientific. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.