Abstract
Aims: We sought to assess the reliability of the most frequently used intracoronary physiologic indices (including intravenous adenosine FFR [IV-FFR], intracoronary low-dose adenosine FFR [LD-IC-FFR], intracoronary high-dose adenosine FFR [HD-IC-FFR], Pd/Pa and iFR). We also sought to analyse factors affecting their reproducibility in a real-world patient population.
Methods and results: A total of 91 lesions in 86 consecutive patients were included. Measurements of all physiological indices were repeated within a systematic standardised prospective protocol. All measured indices showed excellent test-retest reliability, with intraclass correlation coefficient (ICC) over 0.96. IV-FFR showed the highest coefficient of variation (CV) values among the studied measurements (Pd/Pa: 0.05; iFR: 0.10; LD-IC-FFR: 0.10; HD-IC-FFR: 0.08; IV-FFR: 0.12). Pd/Pa was significantly less variable than the other indices. On multivariate analysis, female gender, distal lesion location, history of hypertension or kidney failure, as well as presentation as an acute coronary syndrome, were associated with more variability in all physiological intracoronary measurements.
Conclusions: The reliability of most frequently used intracoronary physiologic indices is high. Clinical and anatomic factors significantly influence the reliability of these physiologic indices.
Introduction
Over the last decade, physiological assessment of the haemodynamic impact of a coronary stenosis using pressure wires has become a new paradigm to guide coronary revascularisation1,2. From the pioneers’ early bench development studies to large clinical trials, fractional flow reserve (FFR) has emerged as the most robust coronary physiology index, consistently showing its value to improve patient outcomes when used for selecting lesions for percutaneous coronary interventions (PCI)3-5. FFR is calculated as the ratio of mean distal coronary pressure divided by aortic pressure over the entire cardiac cycle during hyperaemic stimulus. To induce minimum microvascular resistance, FFR should be calculated under conditions of minimal and constant resistance by administrating microvascular vasodilators6. Although continuous intravenous administering of adenosine theoretically provides a more stable and reliable vasodilatation effect, intracoronary adenosine injection is frequently used in the clinical setting due to its simplicity7. On the other hand, some recent studies have suggested that higher doses of intracoronary adenosine produce a greater grade of hyperaemia without compromising safety8,9. Contemporary guidelines recommend assessing intermediate coronary stenosis using FFR to indicate revascularisation based on a fixed dichotomic cut-off of 0.801,2.
The instantaneous wave-free ratio (iFR) is a non-hyperaemic pressure index that samples intracoronary pressure during the diastolic “wave-free” period – a period in the cardiac cycle when microvascular resistance is stable and minimal10. Likewise, Pd/Pa is a simple pressure index that uses mean aortic and distal pressures to the target lesion during the entire cycle11. Both resting indices have been proposed as an alternative to hyperaemia-induced measures in order to minimise time, costs and side effects, therefore promoting an expanded use of physiological indices for guiding coronary revascularisation12.
Interventional cardiologists interpreting the available criteria for physiology-guided revascularisation should be aware of the consequences of the biological variability of these indices for diagnostic classification of stenosis. Unfortunately, there is a lack of data about the intrinsic natural variability of these parameters in a population of intermediate coronary lesions13.
In this study, we sought to assess the reliability of the most frequently used physiologic ischaemia indices (including intravenous adenosine FFR [IV-FFR], intracoronary low-dose adenosine FFR [LD-IC-FFR], intracoronary high-dose adenosine FFR [HD-IC-FFR], Pd/Pa and iFR). In addition, we analysed factors affecting their reproducibility in a real-world patient population.
Methods
STUDY POPULATION
From January 2015 to October 2015, consecutive patients scheduled for coronary invasive investigation and presenting with a clinical indication for an intracoronary pressure-wire study of a coronary stenosis of intermediate severity (visual estimation 40% to 80%) were included. Exclusion criteria were limited to patients with an acute coronary syndrome with troponin elevation within 48 hours before the index procedure, weight >160 kg, previous coronary artery bypass surgery and tandem lesions. However, patients presenting with acute coronary syndrome who needed invasive evaluation of non-culprit lesions after 48 hours from symptom onset were eligible.
All included subjects gave written informed consent in accordance with a specific protocol which was approved by the institutional ethics committee.
CARDIAC CATHETERISATION
Cardiac catheterisation was undertaken through the radial approach. After diagnostic coronary angiography, coronary haemodynamic data were obtained using a 0.014-inch pressure sensor-tipped wire (PrimeWire Prestige® Plus and Verrata®; Volcano Corporation, San Diego, CA, USA) which was advanced through the target lesion via a 6 Fr guiding catheter. Intravenous heparin was given according to patient weight (70 IU/kg) at the start of the procedure. Two hundred mcg of intracoronary nitroglycerine was routinely given before haemodynamic measurements in order to stabilise epicardial resistance. Pressure equalisation was carefully performed at the tip of the catheter before its advancement distal to the stenosis. Likewise, at the end of each set of recordings, the pressure sensor was returned to the catheter tip to ensure that there was no pressure drift. When a pressure drift was detected, the measurements were repeated all over again. All involved operators have extensive experience in the use of the pressure wire (>100 cases).
MEASUREMENT PROTOCOL
The pressures and electrocardiogram signals were extracted from the digital archive of the device console (s5i®; Volcano Corporation). Repeated measures, at least two times, separated by at least three minutes, were made of each individual index in every intermediate coronary lesion included. According to protocol, the same order of determination was always followed: Pd/Pa, iFR, LD-IC-FFR (60 µg), HD-IC-FFR (600 µg), and IV-FFR (140 µg/kg/min). The hyperaemic stimulus was only given when both the Pd/Pa and the heart rate had completely returned to their baseline value. Each intracoronary adenosine bolus was followed by a flush of saline. Measurement of FFR after the intracoronary bolus was started five beats after the end of flushing.
ANALYSIS OF HAEMODYNAMIC DATA
The analysis of every index was made in a fully automated way by customised software applying the specific algorithm for iFR (Version 3.3; Volcano Corporation). Minimum Pd/Pa during intravenous infusion of adenosine and the minimum Pd/Pa after an intracoronary bolus of adenosine were established for FFR value. The analysis cut-off thresholds to define a positive result for resting whole cycle Pd/Pa, iFR and FFR were ≤0.93, <0.90 and ≤0.80, respectively.
QUANTITATIVE CORONARY ANGIOGRAPHY
An independent experienced observer, who was blinded to the results of FFR, performed quantitative coronary angiography. Using the guide catheter for calibration and an edge detection system (CAAS-QCA system; Pie Medical, Maastricht, the Netherlands), the reference vessel diameter and minimum lumen diameter were measured, and the percent area and diameter stenosis was calculated.
STATISTICAL ANALYSIS
Quantitative variables are described with mean and standard deviation and qualitative ones with their frequency distribution. Test-retest reliability was evaluated by the intraclass correlation coefficient (ICC) and its 95% confidence interval (CI). Absolute errors and medians were estimated for each index and the Bland-Altman method was used to represent the intramethod reliability at the index rank14. The mean error for each index was compared between the two subgroups generated according to the corresponding clinical cut-off points, to ascertain if the reliability tended to increase for measures extremely over the corresponding cut-off point. Relative differences and coefficients of variation (CV) were used to express the inter-method variability. Moreover, in order to test the significance of the reliability of the different tests, the CV of interval estimators were assessed15. According to this statistical method, a CV is statistically significantly different when its CI does not include any value of the CV-CI values from the other studied indices. After conducting univariate analysis of the different pertinent clinical, haemodynamic and angiographic variables, multivariate linear regression models were performed for each index, one by one, by selecting only those variables that were considered relevant in the univariate analysis. This allowed the identification of those variables that independently explained the variability of the different measures. Every variable that was considered as biologically relevant was included, and their slopes (β) and 95% CI, as well as the adjusted R square, were determined. The clinical, haemodynamic and anatomic factors included in the univariate analysis were: age, gender, hypertension, diabetes, current smoker, obesity (BMI >35), acute coronary syndrome, anaemia (Hb <12 gr/dl), renal failure (CCr <40 ml/min/1.73 m2), impaired left ventricle ejection fraction (LVEF <35%), atrial fibrillation, heart rate and blood pressure during measurement, coronary location and segment, lesion length, minimal lumen diameter, reference diameter, distal diffuse disease and presence of severely calcified lesion. Statistical analysis was performed using Stata, version 12.0 (StataCorp, College Station, TX, USA). P-values <0.05 were considered to indicate statistical significance.
Results
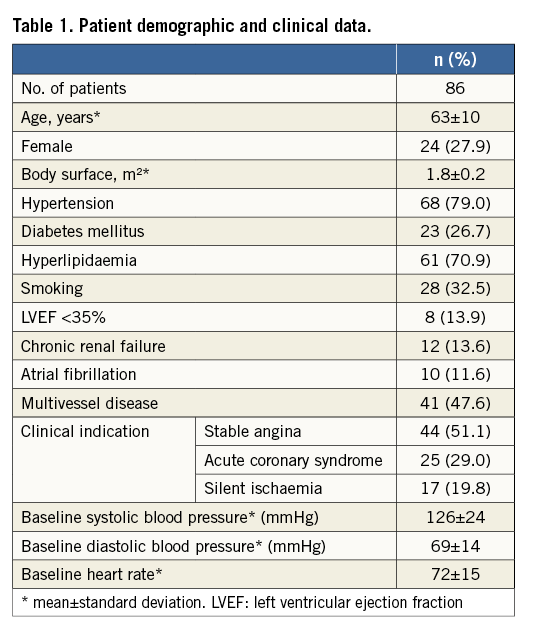
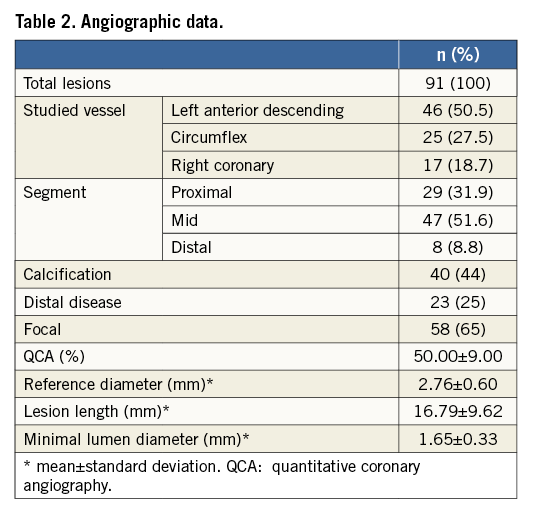
A total of 91 lesions in 86 consecutive patients were included in the study. During the study period, two eligible patients refused to participate. The baseline clinical and angiographic characteristics of these patients are summarised in Table 1 and Table 2. Overall baseline features were characteristic of an unselected population of patients undergoing coronary angiography for diagnostic purposes. A total of 902 intracoronary measurements were performed in the corresponding 91 target lesions of ambiguous severity.
The mean±SD values for each physiologic index were 0.94±0.05, 0.87±0.08, 0.81±0.09, 0.81±0.08 and 0.80±1.1 for Pd/Pa, iFR, LD-IC-FFR, HD-IC-FFR and IV-FFR, respectively. The box-plot distribution of the studied variables is shown in Figure 1.
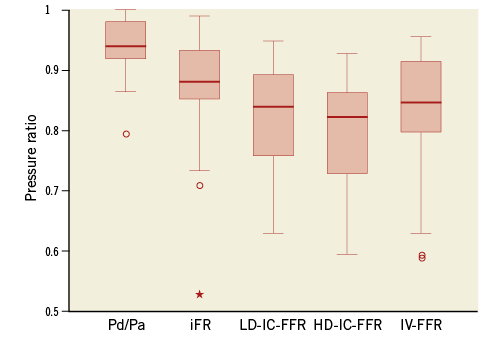
Figure 1. Pd/Pa, iFR and FFR box plots. The iFR and FFR ranges are larger than resting whole cycle Pd/Pa (Pd/Pa: 0.86-1.00; iFR: 0.74-0.96; LD-IC-FFR: 0.63-0.99; HD-IC-FFR: 0.60-0.95; IV-FFR: 0.63-1.00). HD-IC-FFR: high-dose intracoronary adenosine fractional flow reserve; iFR: instantaneous wave-free ratio; IV-FFR: intravenous adenosine fractional flow reserve; LD-IC-FFR: low-dose intracoronary adenosine fractional flow reserve
INTRAMETHOD RELIABILITY
All indices showed excellent test-retest reliability, with ICC over 0.96 and very accurate confidence intervals (Table 3). The studied physiological indices had very low relative differences between the repeated measurements and also very low CV, which speaks in favour of a high homogeneity of each of the measurements and little difference among them. Interestingly, IV-FFR showed the highest CV values among the studied measurements (Pd/Pa: 0.05; iFR: 0.10; LD-IC-FFR: 0.10; HD-IC-FFR: 0.08; IV-FFR: 0.12). Additionally, Pd/Pa was significantly less variable than the other indices according to the CV confidence interval estimation method (Table 3), with the value of the CV half that of the other indices. Pd/Pa CV-CI presented the lowest values and did not include any other indices’ CV-CI estimators (Figure 2). According to the default cut-off values for each index, the lowest value of misclassification frequency was for HD-IC-FFR (1.4%), followed by IV-FFR (3.7%), iFR (8.2%), Pd/Pa (8.4%) and LD-IC-FFR (9.4%).
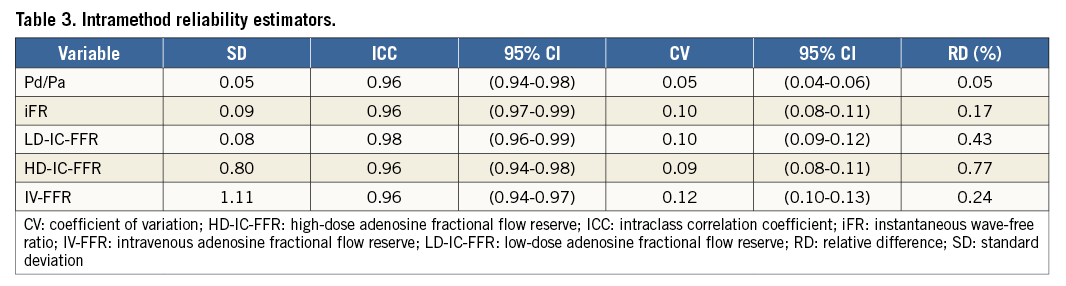
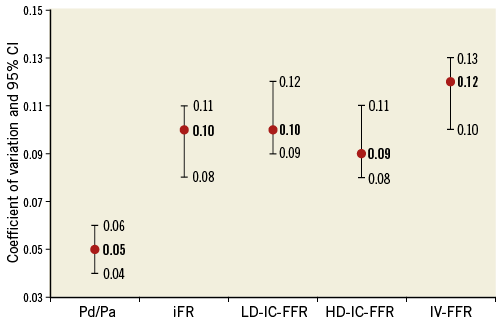
Figure 2. Coefficients of variation confidence interval estimation method. IV-FFR showed the highest CV values among the studied measurements. HD-IC-FFR: high-dose intracoronary adenosine fractional flow reserve; iFR: instantaneous wave-free ratio; IV-FFR: intravenous adenosine fractional flow reserve; LD-IC-FFR: low-dose intracoronary adenosine fractional flow reserve
The Bland-Altman graphical method also confirmed very high test-retest reliability for all these indices (Figure 3). Finally, the mean errors of each index were compared according to the groups generated by the clinically established cut-off points. Notably, maximal variability tended to increase significantly for very positive measures far above the cut-off points for iFR, HD-IC-FFR and IV-FFR (Figure 3).
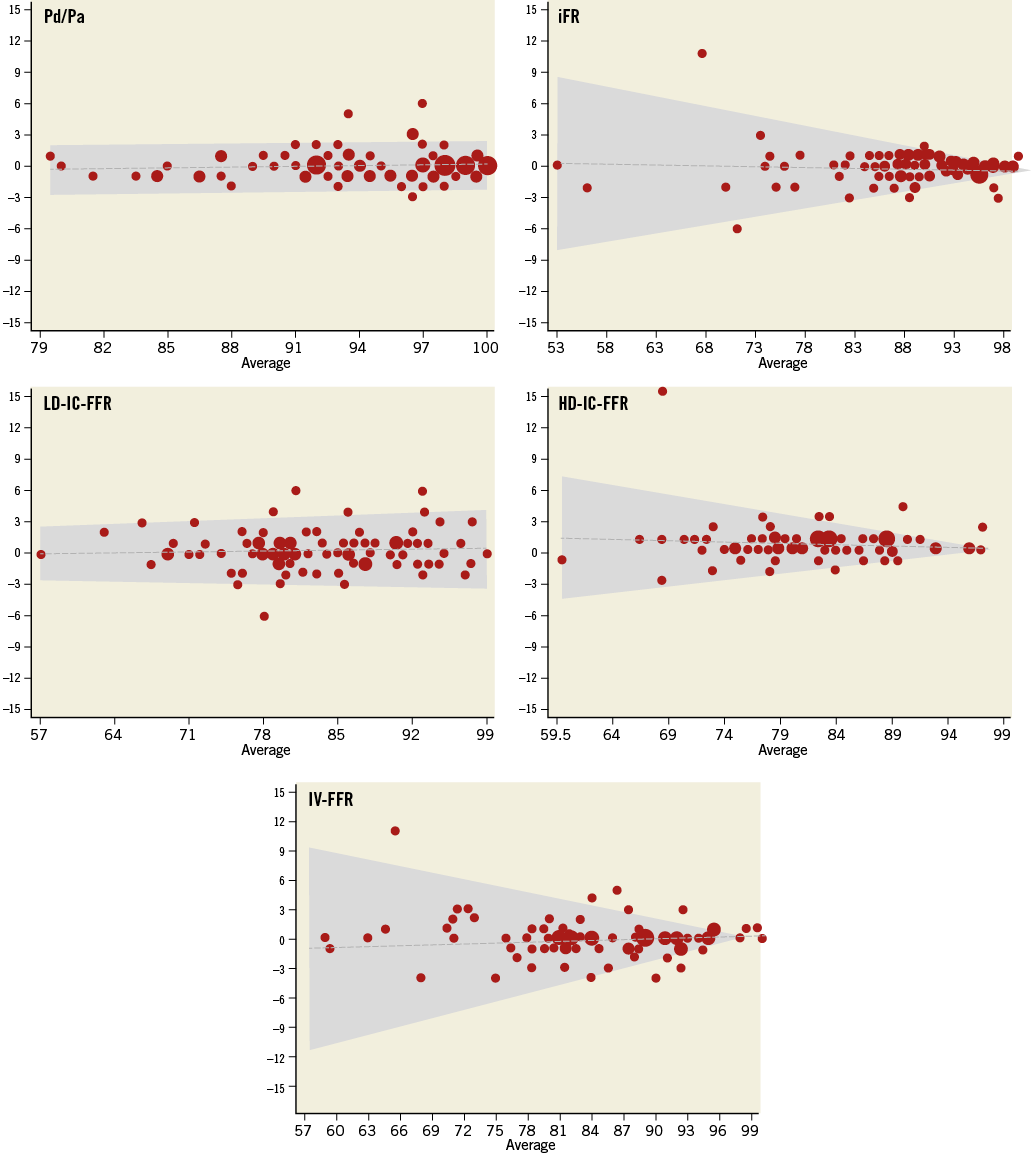
Figure 3. Bland-Altman analysis for the test-retest reliability of all the coronary pressure indices included. The differences between the two measurements are shown on the vertical axis. After comparing the mean error among the groups created according to each cut-off point, we observed that variability tended to increase significantly for very positive measures for iFR, HD-IC-FFR and IV-FFR (p<0.001). HD-IC-FFR: high-dose intracoronary adenosine fractional flow reserve; IFR: instantaneous wave-free ratio; IV-FFR: intravenous adenosine fractional flow reserve; LD-IC-FFR: low-dose intracoronary adenosine fractional flow reserve
VARIABLES EXPLAINING THE VARIABILITY OF THE MEASURES
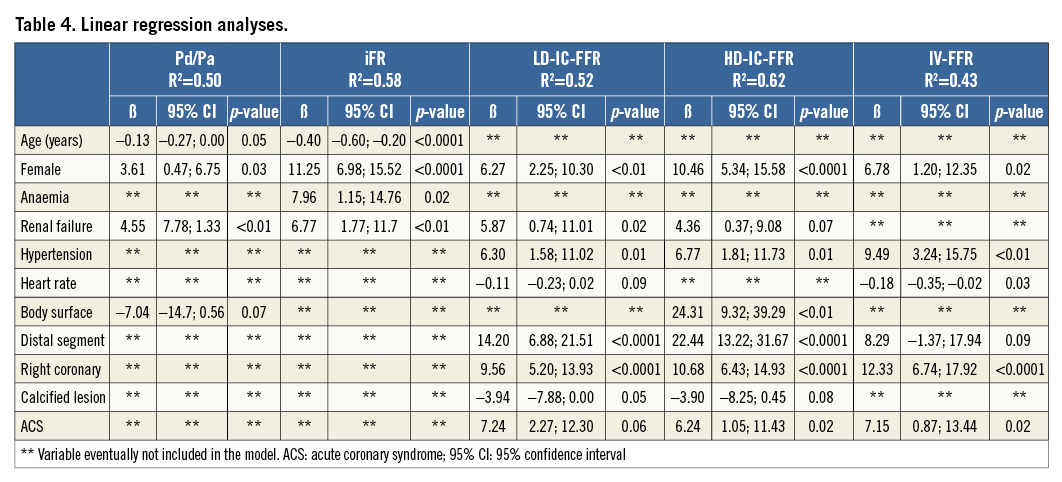
Being a woman was significantly associated with a higher variability in all the indices. Presence of a unique intermediate coronary lesion in a distal segment was the anatomic factor most strongly associated with a high variability in every studied index. Finally, a clinical history of hypertension or kidney failure and a presentation as an acute coronary syndrome were also identified as the factors explaining most variability in these physiologic indices (Table 4).
Discussion
The results of our study demonstrate an excellent reliability in the entire spectrum of invasive physiological indices currently used in routine clinical practice to assess intermediate coronary stenosis. To the best of our knowledge, this study provides the first specifically designed study aimed at determining the test-retest reproducibility data for these different physiologic indices.
Clinicians should be aware of the precision and robust reliability of the invasive physiological tests commonly used to ascertain the ischaemic impact of a coronary lesion. However, the measurement process always involves some degree of error, as there are different factors inherently associated with the individuals, the observers, the measuring instrument, the technique and even the methodology, which may induce variation. This is of relevance as current guidelines recommend FFR clinical use based on a fixed 0.8 cut-off criterion. This implies transforming a continuous variable, such as myocardial ischaemia, into an “all or nothing” choice1,2. Although attractive indeed from a clinical standpoint, in order to help in the decision-making process of guiding revascularisation procedures, the limitations of this approach are obvious.
It should be borne in mind that, although our data show high accuracy in the measurements, with ICC above 0.96 for every studied index, a relative difference (RD) ranging from 0.05 to 0.77 means that, in some patients, an FFR value of 0.81 could be 0.79 in the next measurement. This issue acquires a unique clinical relevance within the region of physiologically intermediate values, namely around the 0.80 cut-off value. Petrarco et al previously investigated the effects of FFR intrinsic variability on treatment decisions in this clinically relevant zone16. Using a retrospective analysis of the DEFER trial reproducibility data, they found an absolute difference of 0.03±0.02 in FFR measurements. Establishing a cut-off value of 0.80, these investigators found that each time a single FFR value falls between 0.75-0.85 there is a chance that the dichotomous classification of the stenosis will change if the test is repeated16,17. Other physiologic indices were not evaluated in their study.
Previous investigation by Schlundt et al found results consistent with those of the present study when analysing the intramethod variability of LD-IC-FFR and IV-FFR with a trend towards less variability in IC-FFR18. Likewise, Johnson et al found an excellent and clinically insignificant average difference between repeated measurements (average difference between measurements was <0.005 for all studied indices)19. Conversely, they found lower reliability values for resting parameters than for FFR. Lumping together IC and IV adenosine in the FFR group and differences in IC adenosine dose and in the software for post hoc analysis could explain these divergent results19.
Otherwise, the excellent reliability data obtained should make interventional cardiologists consider the unnecessary repetition of the same test. Therefore, we firmly believe that, despite the low variability of our measurements, integrating both clinical and anatomical information with the invasive functional test data remains crucial in the clinical decision-making process of revascularisation of these patients, particularly for those with values within the so-called “grey area”.
As might be expected, Pd/Pa showed the lowest values for CV and RD, while IV-FFR presented the lowest reliability values within the hyperaemic indices. A variable response of the microcirculation to adenosine, due to its local and systemic effects20-23, and potential technical problems during drug administration, especially with the intracoronary route, might explain the minimal, but not absent, test-retest variability of these measures. On the other hand, we observed that the highest variability of the measurements tended to cluster in lower values, becoming larger as the distance from the cut-off point increased. In other words, as lesions become more ischaemia-provoking, HD-IC-FFR, IV-FFR and iFR values become more variable. This effect, however, was not found for Pd/Pa and LD-IC-FFR. An association between coronary lesion severity and the variability of the downstream microvascular resistance has been previously reported by Chamuleau et al using a Doppler and pressure guidewire24. A large heterogeneity of minimal microvascular resistance during maximal hyperaemia could be seen in patients with severe flow-limiting coronary artery disease. Paradoxical vasoconstriction, as a result of passive collapse of larger-sized (>100 μm) arterial microvessels due to reduced distending pressure, might explain these findings25,26. In clinical practice, as shown in our population, this high variability among the extreme positive values would not affect the dichotomic lesion classification as, by definition, they are all far away from the clinically relevant cut-off values.
Importantly, clinical and anatomical sources of variability have not been previously studied. In our population, we identified several factors consistently associated with a lower reliability in the measurements. Female gender was associated with higher FFR values. Previous studies suggested that women are more likely to have impaired coronary microvascular reactivity to adenosine than men27,28. Moreover, a clinical history of hypertension, acute coronary syndromes and kidney failure was also associated with higher variability in intra-patient repeated measurements. Interestingly, the presence of atrial fibrillation and high-density extrasystolia did not impact on the reliability of iFR measurements. Finally, among the angiographic parameters analysed, the location of the target lesion on a distal segment was the most robust factor consistently associated with a low reliability for all the measurements. It is tempting to suggest that measurements in distal lesions are more prone to technical subtleties and inconsistent drug effects compared to proximal lesions.
Study limitations
This single-centre, observational study has the limitations inherent to this kind of observational trial. However, the study was performed in an unselected patient population, with differences in baseline characteristics, and involved multiple operators. We therefore believe that this is representative of a typical workload clinical practice. The uniform sequence of measurements, strictly followed by protocol, might have influenced the results because of adenosine tachyphylaxis. However, special care was taken in every patient to wait for the restoration of baseline haemodynamic parameters before beginning each new measurement.
Conclusions
Invasive physiological assessment tests of intermediate coronary stenosis showed an excellent reliability. Pd/Pa provides a lower intra-patient variability than iFR and adenosine-induced tests. Female gender, distal lesion location, history of hypertension or kidney failure, as well as presentation as an acute coronary syndrome were associated with poorer reliability for most of the physiological intracoronary measurements.
| Impact on daily practice Commonly used intracoronary physiologic indices provide excellent reliability parameters. As every biological measurement, however, they have some intrinsic biological variation: we were able to identify female gender, distal lesion location, history of hypertension or kidney failure, as well as presentation as an acute coronary syndrome, as independently associated with a greater variability. Integration of clinical data and previous non-invasive tests on patients should be mandatory before making any revascularisation decision, specifically in these particular settings and in the grey-zone results. |
Conflict of interest statement
The authors have no conflicts of interest to declare.