A 62-year-old man had stenting of the proximal left anterior descending artery with a 3.5×23 mm CYPHER® drug-eluting stent (DES) (Cordis, Johnson & Johnson, Warren, NJ, USA) 10 years ago. He presented with unstable angina. Optical coherence tomography (OCT) revealed evidence of neoatherosclerosis and a minimal luminal area (MLA) of 2.08 mm2 as well as evagination with extensive late stent malapposition (Figure 1A-Figure 1C, Moving image 1).
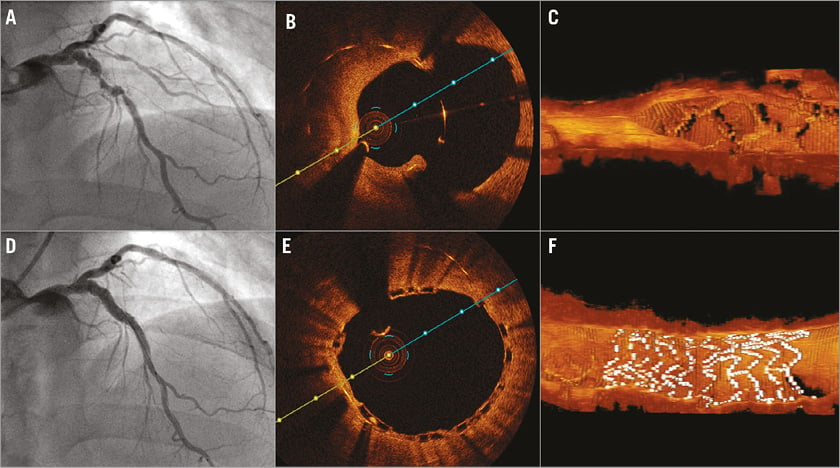
Figure 1. Very late metallic stent thrombosis and in-stent restenosis treated with a BVS. A) In-stent restenosis and focal aneurysm in the left anterior descending artery around the sirolimus DES implanted for 10 years. B) Neointimal proliferation and evagination with stent malapposition detected on 2D and 3D OCT (C). D) Final angiography and OCT (E & F) reveal the adequate scaffold expansion and apposition with an MLA of 9.74 mm2.
After re-dilatation of the lesion, drug-eluting balloons (DEB) were applied across the stented segment and a 3.5×12 mm Absorb Bioresorbable Vascular Scaffold (BVS) (Abbott Vascular, Santa Clara, CA, USA) was deployed proximally to cover the aneurysm and a proximal stent-edge dissection. This was followed by post-dilation of the scaffolded segment using a 4.0×15 mm NC balloon. Final angiography and OCT study revealed adequate scaffold expansion and apposition with an MLA of 9.74 mm2 (Figure 1D-Figure 1F).
OCT imaging can provide valuable insights into late failure of metallic DES. Late stent malapposition has been reported following DES implantation and is recognised as a hallmark for late stent thrombosis. Here the patient presented with both restenosis and aneurysm formation. Implantation of another DES may continue to aggravate the late stent malapposition issue. On the other hand, use of bare metal stents would result in a high likelihood of recurrent restenosis or neoatherosclerosis. Hence, BVS may be a reasonable alternative in the treatment of patients with such late DES failure.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. 3D OCT of the CYPHER evagination and late stent malapposition.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. 3D OCT of the CYPHER evagination and late stent malapposition.