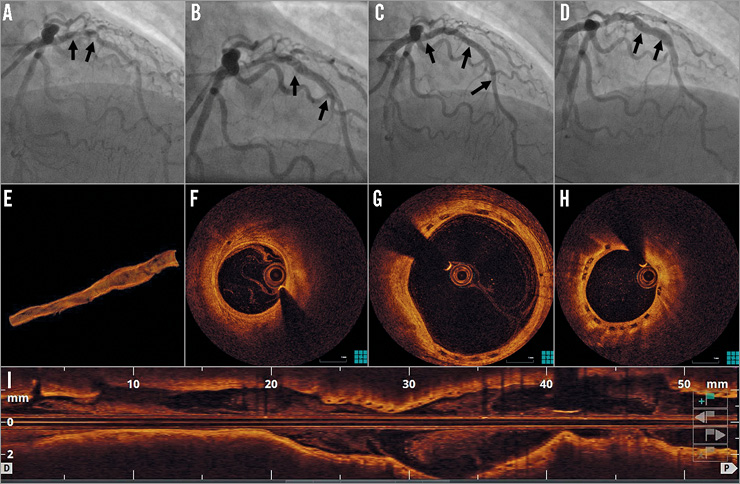
A 54-year-old male underwent coronary angiography for non-ST-elevation myocardial infarction. This identified significant left anterior descending artery (LAD) disease (Panel A, Moving image 1). After predilatation with a 3×15 mm balloon, a type B dissection occurred (Panel B, Moving image 2). Two Absorb™ bioresorbable vascular scaffolds (BVS) (Abbott Vascular, Santa Clara, CA, USA) were implanted in the mid (3×18 mm at 16 atm) and proximal (3.5×28 mm at 6 atm) LAD (Panel C, Moving image 3). After post-dilatation with a 3.5×15 mm non-compliant balloon at 18 atm, the vessel diameter was 3.5 mm. Thirty-two months later, a coronary angiogram showed a segment of ectasia in the proximal and mid LAD, with a maximal vessel diameter of 5.3 mm (Panel D, Moving image 4). Optical coherence tomography demonstrated the absence of strut malapposition. Instead, completely endothelialised strut remnants were visible in the positively remodelled vessel wall (Panel E, 3D reconstruction, Panel F, distal reference, Panel G, ectatic segment, Panel H, proximal reference, Moving image 5). This suggests that the scaffold was incorporated into the vessel wall and that gradual degradation of the scaffold resulted in disruption of strut continuity, allowing outward strut displacement along with the enlarging coronary artery. Positive remodelling causing late acquired metallic DES malapposition has been recognised as a potential cause for very late stent thrombosis. This image demonstrates that coronary aneurysm formation can occur after BVS implantation. However, in contrast to metallic DES, the transient nature of BVS integrity can result in the absence of late strut malapposition. Whether this entails a lower risk of very late thrombosis after positive coronary arterial remodelling remains uncertain.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Baseline coronary angiogram.
Moving image 2. Coronary angiogram after balloon dilatation.
Moving image 3. Angiographic result after BVS implantation.
Moving image 4. Angiogram 32 months after BVS implantation.
Moving image 5. Optical coherence tomography.
Supplementary data
To read the full content of this article, please download the PDF.
Baseline coronary angiogram.
Coronary angiogram after balloon dilatation.
Angiographic result after BVS implantation.
Angiogram 32 months after BVS implantation.
Optical coherence tomography.