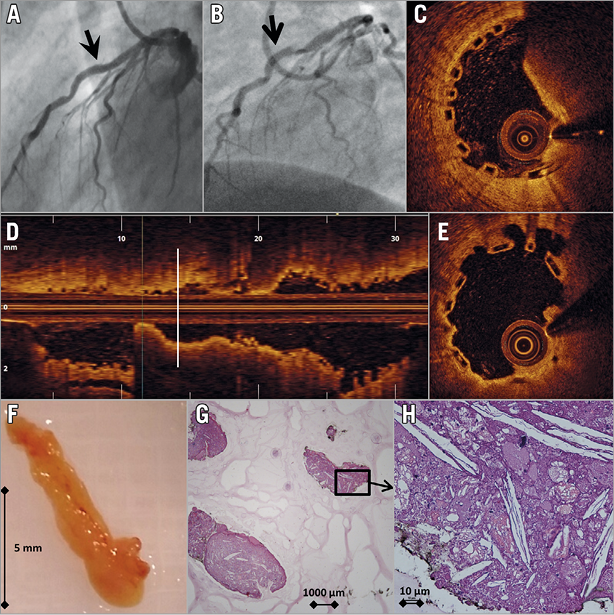
The patient was a 53-year-old (male) suffering from unstable angina due to stenosis of the left anterior descending (LAD) artery. After 2.5 mm balloon predilatation (12 atm), a 3.0×28 mm bioresorbable vascular scaffold (BVS) (Absorb™; Abbott Vascular, Santa Clara, CA, USA) was implanted at 14 atm with an angiographically good result (Panel A). The patient was discharged on aspirin and clopidogrel.
Coronary angiography one month later showed a severe lesion in the distal part of the BVS, suggesting in-stent thrombosis (Panel B). Optical coherence tomography (OCT) confirmed mixed thrombus (Panel C, Panel D). With an aspiration catheter, a white structure measuring 9×2 mm (Panel F) was evacuated. Control OCT confirmed the disappearance of a protrusive structure, revealing an area of suboptimal BVS expansion and apposition (Panel E). A 3.5 mm non-compliant balloon post-dilatation (16 atm) was performed. OCT re-evaluation after one month was inconspicuous.
Platelet reactivity test (Multiplate® analyser; Roche Diagnostics Limited, Rotkreuz, Switzerland) demonstrated normal response to clopidogrel. Histologic examination of the aspirated debris revealed atherosclerotic plaque with a high concentration of cholesterol crystals, histiocytes, lymphocytes and red blood cells (Panel G, Panel H).
Although suggestive of in-scaffold thrombosis, this image shows the probable cause to be plaque protrusion into the scaffold lumen. The mechanism is eccentric plaque position in combination with insufficient expansion and apposition of a BVS within an angulated segment. This case emphasises the need for lesion preparation and post-implant optimisation when implanting BVS.
Conflict of interest statement
The authors have no conflicts of interest to declare.