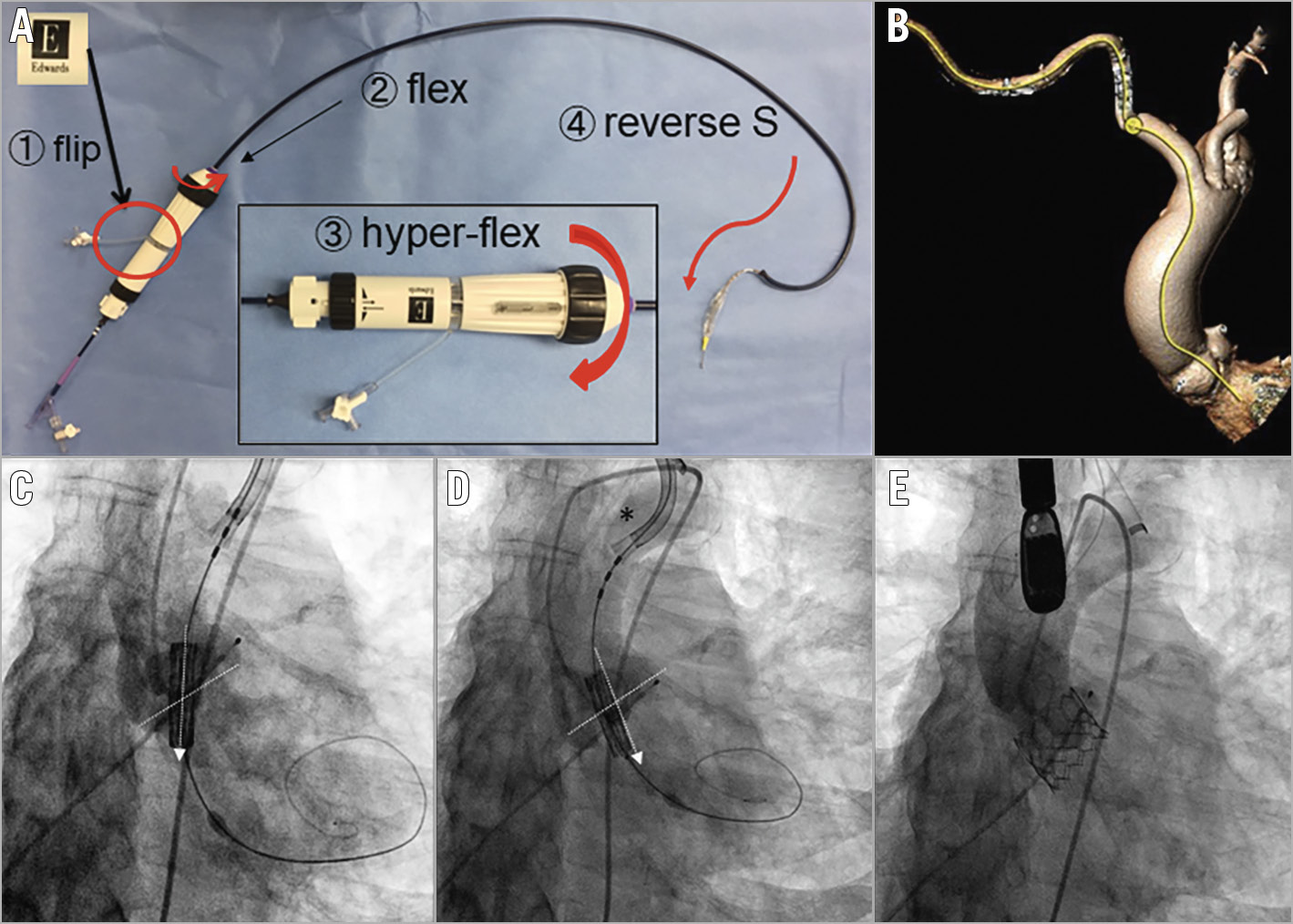
Figure 1. Right transaxillary transcatheter aortic valve replacement using the SAPIEN 3 valve and “flip-n-flex” technique. A) Step-by-step illustration of the “flip-n-flex” technique. B) Tortuous delivery route from the right axillary artery to the aortic root (yellow line). C) Malalignment of the bioprosthesis (arrow) with the aortic root. Dotted line marks the annulus. D) Coaxial alignment after “flip-n-flex” manoeuvre. Note the hyper-flexed delivery device (asterisk). E) Post-deployment aortic angiography showing the well-positioned valve and no significant paravalvular leak.
Transaxillary (TAx) transcatheter aortic valve replacement (TAVR) is rarely performed with balloon-expandable valves especially via the right axillary artery due to anatomical constraints1,2. We present a case of right TAx-TAVR where challenging vascular anatomy was noted, and where a simple “flip-n-flex” technique (Figure 1A) was used to facilitate the insertion and coaxial implantation of the SAPIEN 3 valve (Edwards Lifesciences, Irvine, CA, USA).
An 89-year-old male with symptomatic severe aortic stenosis and peripheral arterial disease was referred for TAVR. The left axillary artery was found to have a small luminal diameter and unfavourable angulation on preoperative computed tomography angiography (CTA), so the right axillary artery access was planned. A considerably tortuous vasculature from the right subclavian artery to the aortic root was revealed on the CTA and intraoperative aortography (Figure 1B, Moving image 1). In addition, the angle of the aortic annulus to the horizontal plane measured >45° which further complicated valve positioning. After access was obtained to the right axillary artery, a 14 Fr expandable sheath (Edwards Lifesciences) was advanced to the aortic arch with the “seam” positioned upward over an Amplatz Super Stiff™ wire (Boston Scientific, Marlborough, MA, USA) to accommodate the tortuosity to a greater degree (Moving image 2). The 26 mm SAPIEN 3 delivery system was rotated 180° and advanced with the Edwards logo facing downwards (step ←, “flip”), as opposed to facing up per the manufacturer’s recommendation. Thereby, the device could articulate in the direction of the vasculature when flexed during insertion (step ↑). During the initial attempt, we noticed the malalignment of the valve (Figure 1C, Moving image 3). Therefore, we modified the procedure by hyper-flexing the device and configuring the wire against the greater curvature of the aorta (step →, “flex”). Gentle torque of the device and fine adjustment ensured the perpendicular orientation of the SAPIEN 3 valve to the aortic annulus (Figure 1D, Moving image 4). The hyper-flexing of the flex catheter (1st curve) and positioning the wire along the axis of the aorta (opposite 2nd curve) created a “reverse S” shape which compensated for the vascular tortuosity (step ↓). After valve deployment, an aortography demonstrated trace paravalvular leak and optimal valve position (Figure 1E, Moving image 5). The “flip-n-flex” technique was a critical element in the successful performance of right TAx-TAVR through a tortuous delivery route. Novel use of the pre-existing device features was advantageous to this procedure.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Aortography showing tortuous vascular anatomy.
Moving image 2. Inserting the expandable sheath.
Moving image 3. Initial attempt at positioning the valve.
Moving image 4. Coaxial alignment prior to valve deployment.
Moving image 5. Post-deployment aortography.