Transcatheter aortic valve replacement (TAVR) has expanded widely in recent years. The femoral access constitutes the gold standard and the first-line access for TAVR procedures1,2, allowing totally percutaneous procedures. Despite several iterations in device profiles and the improvement of TAVR techniques, 10 to 15% of patients are deemed ineligible for femoral access due to unfavourable femoral or aortic anatomy3. While the European guidelines4 recommend the surgical option in intermediate-risk patients if the femoral access is not feasible, non-femoral peripheral (nFP) accesses have emerged as alternatives to the femoral access, achieving comparable results in high-volume centres5,6 with a trend towards more minimalist and less invasive procedures7. More recently, in a propensity-matched study, the French TAVR group8 reported that nFP TAVR was associated with similar outcomes compared to transfemoral TAVR except for a twofold lower rate of major vascular complications and unplanned repairs, regardless of the centre volume. In this issue of EuroIntervention, two papers9,10 report the results of two alternative nFP access routes for TAVR procedures. The first paper by Costa et al9 reports the initial European experience of transcaval TAVR.
The authors conclude that transcaval access for TAVR is feasible and safe in patients not suitable for femoral access. In fact, 10% of patients experienced major vascular complications, which is quite high when compared with the results reported in the French registry8 for nFP access (0.68%). Furthermore, about half of the patients had a residual aorto-caval shunt without any information on their midterm and long-term evolution. In this study, fifty patients were enrolled in five high-volume centres over a five-year period. This reflects the small number of potential candidates for this approach nowadays; this number will be even lower in the future. The second paper by van der Wulp et al10 reports the results of 200 patients who had TAVR through a subclavian/axillary access with rates of 0.5% major vascular complications and 8.5% unplanned vascular repairs.
The authors developed a predictive model of vascular complications. A ratio of the sheath area to the axillary artery minimal lumen area >1.63 was found to be the strongest independent predictor of these complications. Although the developed model is very interesting, its discriminatory power remains intermediate with an area under the curve of 0.67. The third nFP access for TAVR not addressed in these two papers is the transcarotid (TC) access. Surprisingly, the authors of the first paper9 proposed the transcaval approach to their patients not suitable for either the transfemoral or axillary approach and did not first consider the TC approach. The TC-TAVR approach (Figure 1) represented 3.4% of patients treated with TAVR in the FRANCE TAVI registry2. The TC access has the potential to alleviate the drawbacks of the other nFP accesses. Indeed, the carotid artery is easily exposed. The closure of the artery at the end of the procedure is performed with extreme simplicity using well-known vascular techniques. The short distance between the entry point and the aortic valve facilitates the stability of the valve during the deployment. Patients can be mobilised as soon as they are returned to their rooms. Left carotid access for TAVI should be favoured. It allows superior coaxial alignment, optimal positioning for the transcatheter valve during device deployment, and a simple operating room configuration. On the other hand, manipulation of the carotid artery and insertion of a large-bore sheath could potentially increase the risk of stroke. Reported 30-day cerebrovascular events were under 2.5% in many series7,11,12. These events were reduced by the use of local anaesthesia, reaching a rate as low as 0%7. However, in a propensity-matched study using the France TAVI registry data, TC-TAVR showed a twofold higher rate of stroke but a twofold lower rate of major vascular complications compared to transfemoral TAVR13.
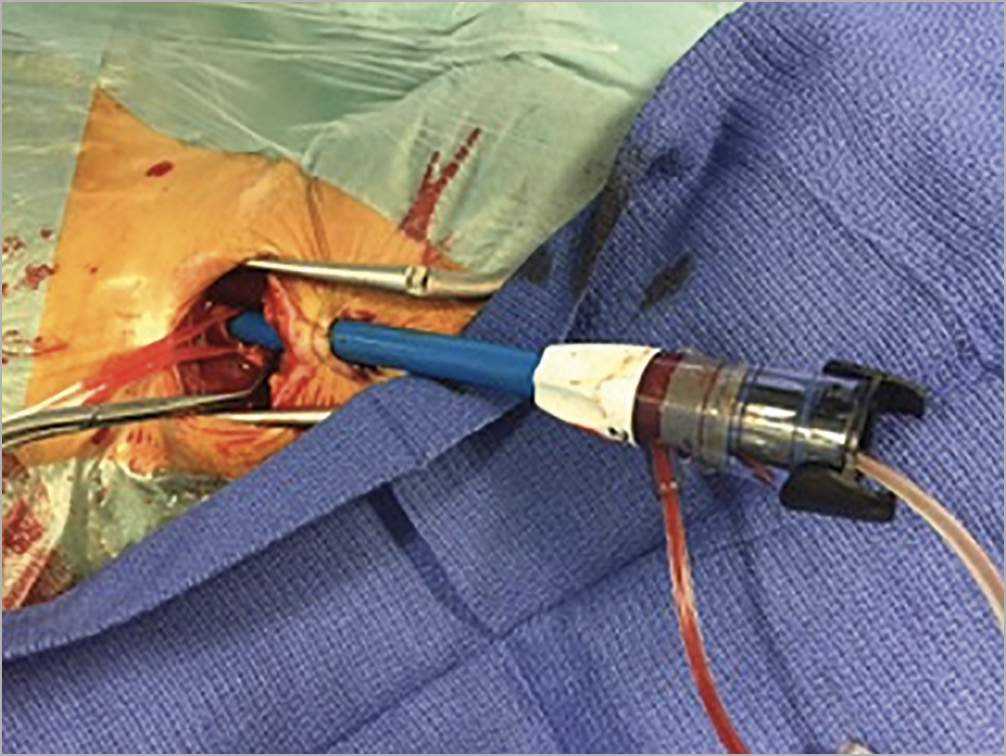
Figure 1. Transcarotid access.
In conclusion, although femoral access remains the first choice in TAVR, nFP TAVR may be a safe alternative when the femoral access risk is considered too high and may be favoured over surgery in patients not suitable for transfemoral TAVR.
Conflict of interest statement
T. Modine is a consultant for Boston Scientific, Medtronic, Edwards, Cephea, MicroPort, GE, Abbott; he received a research support grant from Edwards. The other authors have no conflicts of interest to declare.