Introduction
A substantial proportion of candidates for transcatheter aortic valve implantation (TAVI) still present a contraindication to transfemoral (TF) access. Furthermore, major vascular and bleeding complications remain concerning issues in patients undergoing TF TAVI, with an accompanying significant impact on mortality and morbidity.
Transcarotid (TC) TAVI was initially described by Modine et al1; it has subsequently proven to be reproducible2,3 and is associated with significant potential regarding early morbidity and hospital stay. Nonetheless, it still has not achieved broad consensus.
In this report, we sought to present a single-centre experience of TC TAVI, with particular focus on postoperative clinical, neurological, and haemodynamic outcomes.
Methods
PATIENT SELECTION AND PREPROCEDURAL ASSESSMENT
Candidates for TAVI were evaluated by the Heart Team. The TC approach was considered in case of unsuitable transfemoral access. A contrast-enhanced computed tomography (CT) scan was employed for screening of the anatomy of epiaortic vessels; the left common carotid artery was considered as the first-line choice. Preoperative sizing was performed using EndoSize software (Therenva, Rennes, France) (Figure 1). The presence of contralateral common or internal carotid artery stenosis ≥50% was considered an exclusion criterion to TC TAVI. Ipsilateral common carotid calcifications were also considered as a contraindication, as well as previous ipsilateral common carotid artery intervention and occlusion of any vertebral artery. However, ipsilateral internal carotid artery stenosis was not considered as a formal contraindication. An internal minimum diameter ≥5.5 mm was required. The circle of Willis was not systematically evaluated.
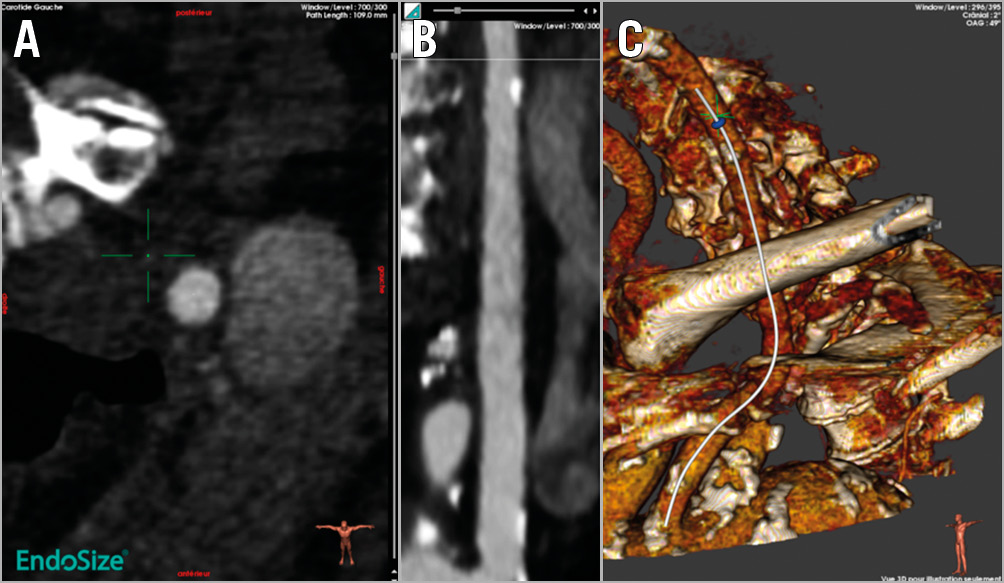
Figure 1. Preoperative sizing of the left common carotid artery. A) Axial view. B) Stretched view, evaluating vascular calcifications and minimal diameter of the left carotid artery. C) 3D rendering.
PROCEDURAL MANAGEMENT
All TC TAVI procedures were conducted within a hybrid operating theatre by a multidisciplinary team. Cerebral oxygenation monitoring was performed using near-infrared spectroscopy. The common carotid artery was approached at the medial border of the sternocleidomastoid muscle (Figure 2). Right transradial (74%) placement of the pigtail catheter was preferred. After valve deployment and sheath removal, the carotid artery was controlled and clamped while maintaining systolic blood pressure above 120 mmHg; the artery was then repaired through interrupted 6-0 polypropylene stitches, and de-clamped after de-airing. Wound closure was completed with drain placement.
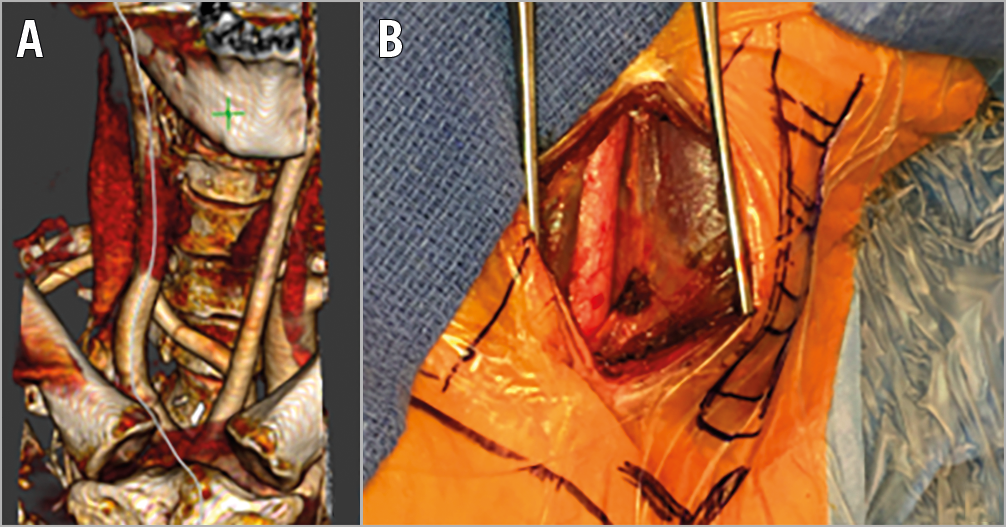
Figure 2. Preoperative sizing of the left common carotid artery. Anatomical configuration (A) and the corresponding operative view (B).
Results
Between April 2017 and June 2018, 317 successive TAVIs were performed at our institution, including 249 femoral and 50 transcarotid procedures. Table 1 describes the baseline characteristics of the patient population and the procedural outcomes.
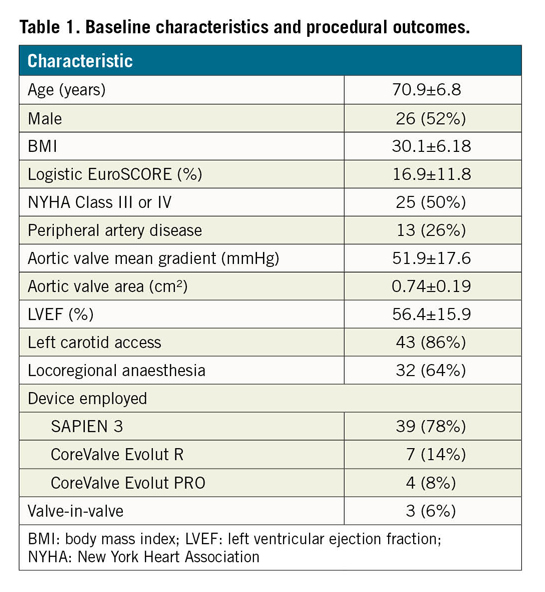
Locoregional anaesthesia was used in the majority of cases (64%). There was one instance of failure of the carotid access (2%), due to insufficient stability of the super-stiff guidewire inside the left ventricular cavity. There were no cases of valve malpositioning, embolisation, or implantation of a second valve. A balloon-expandable valve device was most frequently employed (78%).
Early outcomes are shown in Table 2. There were no cases of early mortality. We noted one case (2%) of stroke, and one transient ischaemic attack (TIA). Life-threatening complications occurred in one case (2%) (haemopericardium requiring pericardiocentesis). Other bleeding complications were classified as major in 2 (4%) cases, and minor in 5 (10%) cases. Concordantly, the rate of access-related vascular complications was as low as 4%.
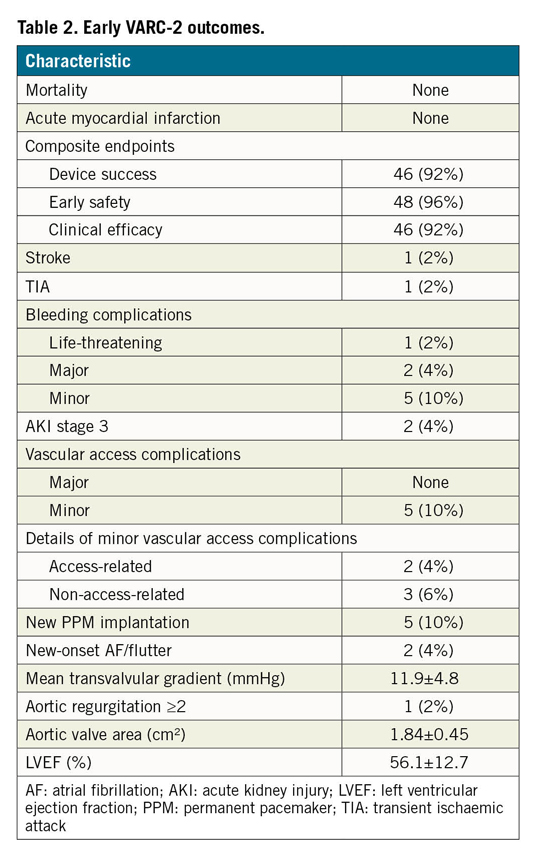
Average hospital stay was 4.1±2.2 days (median three days, interquartile range 2-6). Pre-discharge echocardiography confirmed the effectiveness of transcarotid TAVI (2% rate of aortic regurgitation ≥2/4, 11.9 mmHg average transvalvular gradient). Device success was adjudicated in 92% of cases, early safety in 96% of cases, and clinical efficacy in 92% of procedures.
Discussion
In this report, we present the largest series so far of transcarotid TAVI at a single centre, with uniform management protocols and outcome description using the VARC-2 criteria.
The initial collaborative TC TAVI series indicated very low rates of stroke- and access-related complications, although they suffered from heterogeneous clinical endpoint definitions2. The 30-day rate of cerebrovascular events in our series (4% stroke or TIA) compares favourably with that previously published (6.1% to 5.7%2) about TC TAVI. Careful intraoperative management of the common carotid artery is mandatory in this perspective. Our observed stroke rate (one case, 2%) also compares favourably with a major series focusing on transfemoral TAVI4, underlining the safety of the transcarotid approach under the neurological profile.
Moreover, the transcarotid route allows the performance of awake surgery. The 64% rate of locoregional anaesthesia represents the highest published so far. Furthermore, by using the right radial artery for pigtail insertion, one can avoid femoral arterial puncture. The concurrence of the above factors yielded an average hospital stay of 4.1 days.
Limitations
The single-centre and retrospective nature of the present investigation constitutes its major limitation.
Conclusion
The current study suggests that transcarotid TAVI is associated with low rates of stroke and vascular access complications, with ensuing minimisation of hospital stay. Synergy between different approaches is pivotal for the success of TAVI programmes.
|
Impact on daily practice The reproducibility and safety of the transcarotid approach for TAVI suggest that it can be considered by Heart Teams as an optimal alternative to the transfemoral approach. Its rational employment within TAVI programmes can be useful in optimising the overall outcomes of TAVI patients through prevention of early complications. |
Acknowledgements
The present work was partially conducted in the experimental platform TherA-Image, supported by Europe FEDER.
Conflict of interest statement
G. Leurent declares having received speaker fees from Abbott, Abiomed, AstraZeneca and Novartis and consultancy fees from Abbott and Novartis. The other authors have no conflicts of interest to declare.