Abstract
Transcatheter aortic valve implantation (TAVI) using either the Edwards SAPIEN Valve or Medtronic CoreValve is a well-established procedure. Although initially carried out through transfemoral and transapcial approaches, alternative approaches have become popular and have been utilised to optimise the outcomes. The transaortic (TAo) approach can be used for both these devices and is carried out through the ascending aorta, which can be approached through a partial upper J-sternotomy, T-sternotomy or a right anterior thoracotomy. Due to its familiarity, this procedure is within the comfort zone of surgeons which reduces the learning curve as well as access site-related complications. There are also other potential advantages to the TAo approach, which make it versatile and less invasive. These advantages, indications, contraindications, surgical technique and results will be discussed in this paper. The ongoing ROUTE registry (SAPIEN multicentre European TAo registry), prospective CoreValve multicentre European registry and data from a pivotal trial for CoreValve in the United States will certainly provide robust data in confirming the various advantages seen in centres utilising this approach. Dedicated TAo delivery systems, which could also be used for the subclavian approach, are on the horizon for the newer devices which are currently implanted through other approaches.
Introduction
Aortic stenosis (AS) is a major cause of cardiovascular morbidity and mortality in the elderly. Up to 4.6% of patients aged over 75 have severe AS1. Once symptoms develop, one and five-year survival rates of unoperated patients have been shown to be 60% and 32%, respectively2. The efficacy of aortic valve replacement (AVR) for symptomatic AS is well established3. Despite this, a large population remains untreated because of advanced age and multiple comorbidities1,2,4. This landscape is changing with a marked growth in transcatheter aortic valve implantation (TAVI) ever since it was first demonstrated by Cribier et al using a transvenous, transseptal approach5,6. Randomised controlled trials and large registry data have already demonstrated the feasibility and benefit of TAVI in inoperable and high-risk cohorts7,8. Trials are also underway to evaluate the use of TAVI in medium-risk cohorts (US PARTNER 2 and SURTAVI).
Currently, four devices are CE marked and commercially available - the Edwards SAPIEN XT™ valve (Edwards Lifesciences, Irvine, CA, USA), the Medtronic CoreValve® (Medtronic, Minneapolis, MN, USA), JenaValve™ (JenaValve Technology GmbH, Munich, Germany) and Acurate TA™ (Symetis, Ecublens VD, Switzerland). TAVI was initially performed through a retrograde transfemoral (TF) approach and an antegrade transapical (TA) approach. Two more retrograde approaches were subsequently described, the transaortic approach (TAo) through the ascending aorta and the transsubclavian approach (TS). These are growing in popularity as alternative approaches when TF is not possible. One of the key observations in earlier studies and ongoing registries is the high incidence of access site complications, which directly impact on the mortality and one-year survival7,8. Hence, choosing the right access for a given patient is of paramount importance in order to reduce morbidity and mortality. This will become vital to the utilisation of TAVI in medium or lower-risk patients. In this report, we describe the indications, patient selection, utilisation of imaging techniques in planning, important tips and tricks, the results and advantages of the TAo approach.
TAVI progression
Developments in TAVI technology have focused on three important aspects:
1. making the procedure less invasive, e.g., lowering the profile of the delivery system, percutaneous closure of the femoral artery9,10;
2. lowering the incidence of complications, e.g., paravalvar leak solution, re-capturability11,12;
3. making the procedure less complicated for the user, e.g., alternative access, improvements in the delivery systems13,14.
The TAo approach contributes to all three aspects of this progression and thus translates into a better outcome for the patient and ease for the operator.
Indications for TAo
The TAo approach was initially utilised as an alternative when conventional approaches were not possible. With increasing experience it is now being used as a preferred approach in non-TF patients. This is summarised below.
TF AND TA NOT POSSIBLE
TAVI implantation was carried out and subsequently commercialised using the TF and TA approaches. The landscape of TAVI then was to choose the TF approach and if not possible use the TA approach. It took a long time before TAo was first described for SAPIEN and CoreValve through the ascending aorta for patients who were not suitable for the TF and TA approaches (Moving image 1)15,16.
TA NOT DESIRABLE
With excellent outcomes in the extremely high-risk cohort of patients unsuitable for TF and TA and the ease of the procedure itself, indication for TAo was extended. The initial indications for SAPIEN valve implantation via TAo were patients with poor respiratory function, poor ventricular function and frail patients17,18. For the CoreValve, although the TS approach was described and was gaining momentum as an alternative access, the ease of implantation and good results led to the increased utilisation of the TAo approach when the TF approach was not feasible19,20. At this stage the TAo approach was not yet CE marked and purpose-made delivery systems were not available (Moving image 1). However, important aspects of the procedure were well described20.
PREFERRED OVER TA
This coincided with CE mark (2011) for CoreValve users, and with the availability of the next-generation AS plus system with a nose cone for SAPIEN valve users, along with its CE mark (2012). With purpose-made delivery systems the implantation of the device became easier (Figure 1A, Moving image 2). This also included patients requiring a redo procedure such as a valve-in-valve implantation (Figure 1B, Moving image 3) or a TAVI in the presence of a mitral prosthesis (Figure 1A, Moving image 4)21-25.
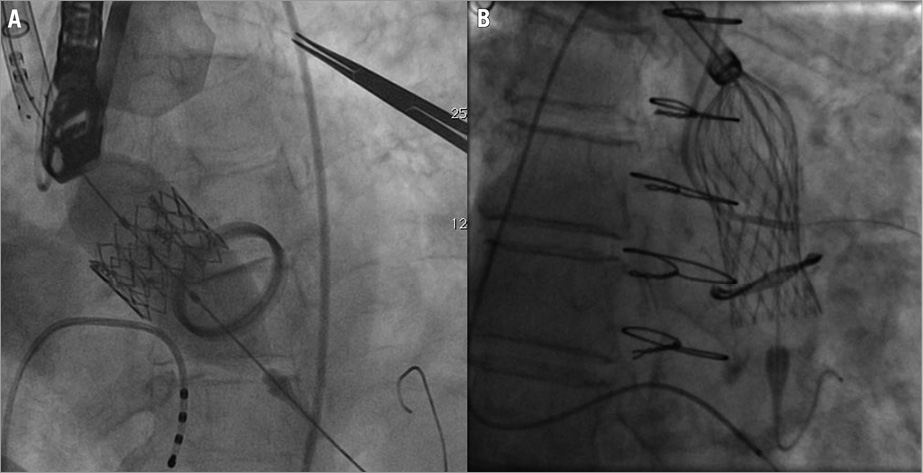
Figure 1. TAo implantation of devices. A) TAo implantation of SAPIEN valve in the presence of a mechanical mitral prosthesis; B) TAo implantation of CoreValve in a degenerated Mitroflow bioprosthesis.
PREFERRED OVER TF
In patients with a mobile atheroma in the arch and/or a large atherosclerotic load in the descending aorta with a possibility of trash embolism, the TAo approach should be considered, as one can avoid the instrumentation of the arch and descending aorta completely.
COMBINED OR HYBRID APPROACH
One of the growing indications for utilisation of the TAo approach has been a combined procedure where the TAo approach is used for the treatment of AS and then an additional procedure is performed through a partial or full sternotomy. These procedures could be off-pump coronary artery bypass grafting (CABG) or thoracic aortic stenting26.
Patient selection
If the patient is accepted for TAVI, an appropriate case selection by a “Heart Team” for this approach is of paramount importance. Two important points when considering suitability of the approach for a patient are:
1. TAo zone – this is the area on the ascending aorta where the purse-strings are placed to perform a TAVI. This area should be free of calcium, should allow perpendicular placement of the TAVI device within the aortic annulus and should be a minimum distance away from the annulus to allow complete deployment of the TAVI device27.
a. Aortic calcification – the incidence of aortic calcification is high in patients undergoing TAVI. We have earlier described distribution of calcium in the ascending aorta and its relevance to TAo27. The TAo zone is usually free of calcium (Figure 2A)27. Essentially, even if the aorta is labelled as a porcelain aorta, if the TAo zone is free of calcium on the CT scan, one can perform a TAo TAVI without exposing the patient to the additional risk of a stroke. CT scan is routinely performed during a TAVI work-up and is the most sensitive investigation to detect the presence of calcium. Using 3-D reconstruction tools it is easy to determine whether the TAo zone is free of calcium.
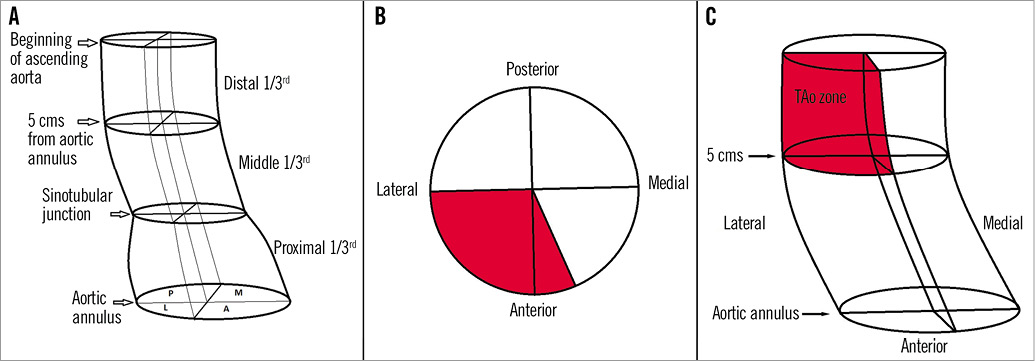
Figure 2. TAo zone. A) Zones of ascending aorta used for calcium mapping. A schematic representation of three segments of the ascending aorta, which are further divided into four quadrants (Anterior, Medial, Posterior and Lateral), thus resulting in 12 zones. B) and C) A schematic representation of the ascending aorta to demonstrate TAo zone (red).
b. Perpendicular placement – with the current delivery systems it is important to try and puncture the aorta so as to allow a perfect alignment of the TAVI device in the aortic annulus.
c. Minimum distance from the annulus – for SAPIEN XT valve this varies from 5-7 cm from the aortic annulus depending on the size of the SAPIEN XT valve (Figure 2B and Figure 2C). For the CoreValve, this varies from 6-7 cm from the aortic annulus. This allows complete deployment of the device.
2. Reoperations – CT scan and angiography should be used to determine the suitability for a TAo approach in a reoperation (Figure 3).
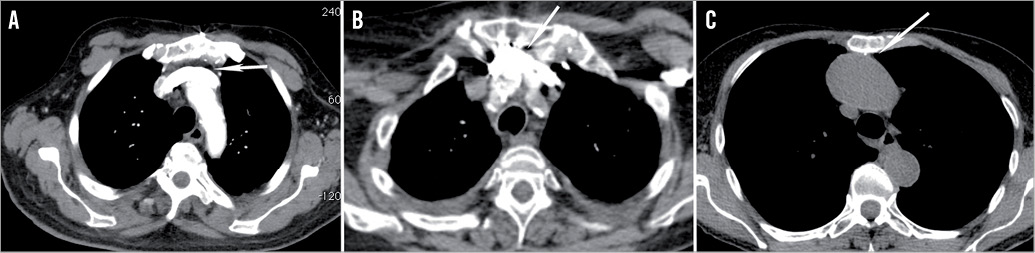
Figure 3. CT scan evaluation, in redo operations when considering TAo approach. A) CT scan at the level of the upper part of the sternum demonstrates innominate vein far away from the undersurface of the sternum, hence not likely to be injured. B) Innominate vein is adherent to sternum and hence TAo through mini-sternotomy is contraindicated. C) Aorta is stuck to the undersurface of the sternum, hence TAo through mini-sternotomy is contraindicated.
a. Proximity of the innominate vein and/or aorta to the sternum – as the procedure only involves an upper sternotomy, if the innominate vein and aorta are away from the sternum then there is no danger of injuring these structures during sternal re-entry. If they are in proximity then a right anterior thoracotomy should be considered.
b. If the patient has had a prior CABG, it is also important to look at the lie of the patent grafts, especially the left internal mammary artery (LIMA). If the LIMA does come to lie in the midline (Moving image 5) or when the right internal mammary artery crosses the midline (Moving image 6), there is a danger of injuring these grafts if a mini-sternotomy is performed. If faced with this scenario, the only way to perform a TAo approach is via a right anterior thoracotomy.
Options for TAo approach
Exposure of the ascending aorta can be carried out either through a mini-sternotomy or through a right anterior thoracotomy. A full sternotomy may be performed when performing a hybrid procedure.
1. Mini-sternotomy – this usually involves a J-upper sternotomy through the second or third right intercostal space or a T-sternotomy through the second intercostal space (Figure 4A and Figure 4B). Mini-sternotomy has certain advantages over the right anterior thoracotomy, such as familiarity for the surgeons, ability to keep the pleural space intact, thus avoiding complications such as pleural effusion, and the ability to convert it to a full sternotomy rapidly if needed (Figure 4C and Figure 4D). Further, patients also tolerate this better than any rib-spreading incision thus aiding patient recovery.
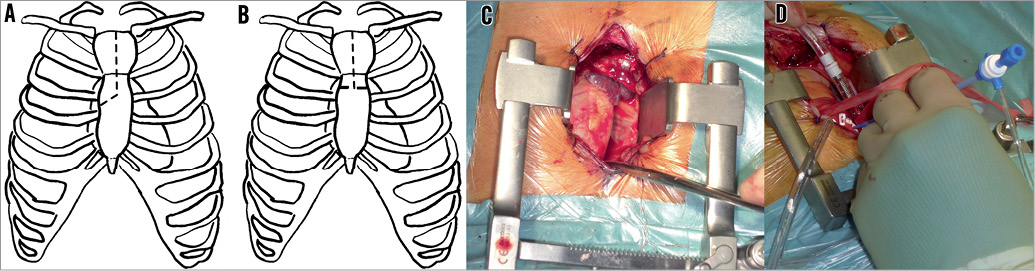
Figure 4. TAo approach through mini-sternotomy. A) Schematic representation of J-sternotomy; B) schematic representation of T-sternotomy; C) exposure of the aorta; D) purse-string sutures with 6 Fr sheath through the TAo zone of the ascending aorta.
2. Right anterior thoracotomy – is performed more commonly through the second right intercostal space but can also be performed through the 1st right intercostal space (Figure 5A and Figure 5B). Right anterior thoracotomy is not a bone-cutting incision and hence has its benefits. It is the approach of choice if the patient has undergone a previous sternotomy especially if the patient has patent bypass grafts (Figure 5C and Figure 5D).
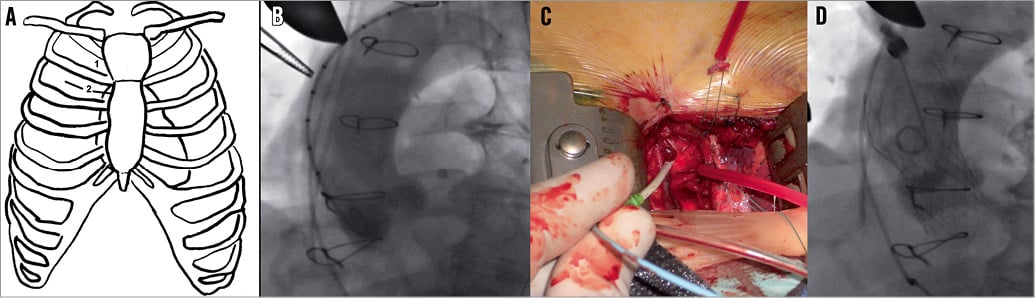
Figure 5. TAo approach through right anterior thoracotomy. A) Schematic representation of right anterior thoracotomy through second intercostal space; B) method to confirm correct site for the purse-string using fluoroscopy which is minimum distance away from the aortic annulus. Metal forceps are clearly seen at the proposed site of purse-string; C) exposure of the aorta with purse-string sutures and 6 Fr sheath through the TAo zone of the ascending aorta; D) fluoroscopic image of CoreValve valve deployment.
It is important to choose the right access for a given patient. Although certain clinical situations such as patent grafts, as explained earlier, dictate the choice, in the majority of cases the decision should be based upon which is technically easier. A right anterior thoracotomy approach is easier if the aorta is to the right side and not very far from the rib cage, and a mini-sternotomy is easier if the aorta is in the midline or deeper.
To assess this, we follow a CT-based protocol as described below. The cross-sectional CT scan is reviewed at the level of the second right costal cartilage. A perpendicular line is dropped from the right edge of the sternum as shown (Figure 6A) and the percentage of the aorta to the right of the line is calculated. Then the distance from the outer margin of the costal cartilage to the upper, outer surface of the aorta is calculated (Figure 6A). A right anterior thoracotomy is the access of choice if the aorta is >50% to the right of the line and if it is <6 cm from the costal cartilage (Figure 6B). Otherwise, a mini-sternotomy is favoured (Figure 6C).
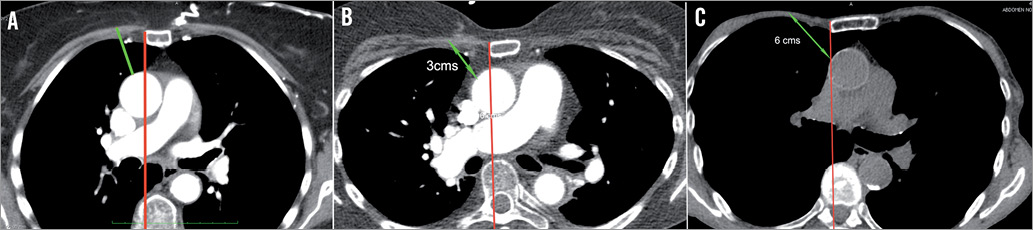
Figure 6. CT-scan-based protocol to choose between mini-sternotomy and right anterior thoracotomy for TAo approach. A) Cross-section image at the level of second costal cartilage. Red line is drawn at the right edge of the sternum to determine percentage of aorta to its right; B) example of a case suitable for right anterior thoracotomy; C) example of a case suitable for mini-sternotomy.
Exceptions to these rules, apart from those with patent grafts or innominate vein/aorta stuck to the sternum, are those patients with poor lung function and those with anatomical deformation of the thoracic cage. In the former, a mini-sternotomy is always better as the pleural space is not opened and, in the latter, the approach is governed by the position of the aorta. If a mini-sternotomy is not feasible and a right anterior thoracotomy could be difficult, then one should evaluate other access routes. Using a double lumen tube to collapse the right lung for a short duration (lung function permitting) is a good adjunct to expose the aorta through a right anterior thoracotomy. This allows an easier access to the aorta by shifting the mediastinum to the right.
Procedural considerations
The surgical technique and details of this approach have been described previously13,20. TAo TAVI has definitely become easier with increasing experience and the availability of dedicated delivery systems. It is essentially either a mirror image of the TA procedure or a TF procedure through the aorta. Thus, it is a technique a “Heart Team” can adapt to in a short time.
The key points for performing a successful TAo TAVI are:
1. A dedicated procedure room set up – this is vital to the performance of this procedure. Example of a set ups is shown (Moving image 7).
2. If in doubt, use a mini-sternotomy as it gives more control to the operator.
3. Reconfirm the site of the purse-string before placement of purse-strings (Figure 5B).
4. Use a suture ring or a bumper to stabilise the sheath (Figure 7).
5. Use the Seldinger technique to cannulate the aorta but, if the aorta is thin, a small incision with a knife may be preferred to insert the sheath.
6. Maintain and control the wire position in the left ventricle similar to that in the TF approach.
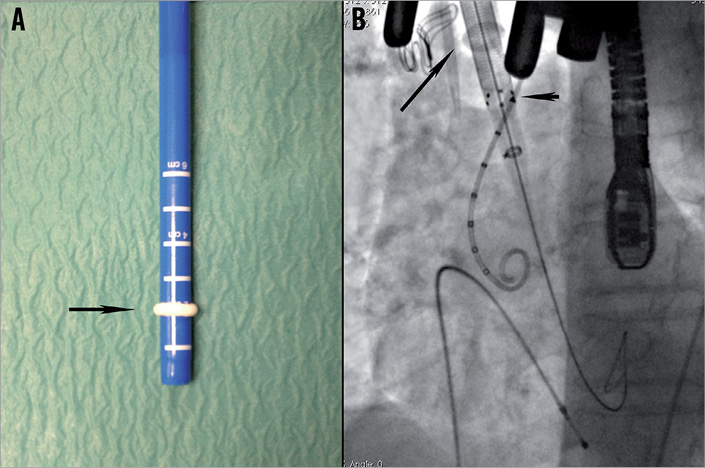
Figure 7. Use of suture ring or bumper. A) Suture ring obtained from Medtronic EOPA cannula size 20 Fr over the Edwards Ascendra+ sheath; B) EOPA suture ring is radiopaque and hence can be visualised under fluoroscopy. It also allows the operator to visualise the relationship between the tip of the sheath and the entry point in the aorta (location of the suture ring).
Results
COREVALVE RESULTS
Following the first clinical procedure this approach was adopted and further developed at the Niguarda Ca’ Granda hospital in Milan16,20. Since then, multiple single-centre and multicentre experiences have been reported21. The largest series of CoreValve direct aortic implantation was presented by Bruschi et al at the 49th annual meeting of The Society of Thoracic Surgeons (personal communications). This multicentre European experience comprised patients treated in 17 centres in nine countries in Europe and in Israel. A total of 312 consecutive patients have been collected, mean age 81±6.5 years, 47% female, mean logistic EuroSCORE 26.6±16.6. Eighty-six percent of patients were in NYHA functional Class ≥III, and peripheral vascular disease was present in 210 patients (67.3% of cases). One hundred and eighty-eight patients had coronary artery disease and 23% of the patients had undergone previous coronary artery bypass surgery. The procedure was performed in 43% of cases through a right anterior mini-thoracotomy in the second intercostal space. Procedural success was achieved in 98.1% of cases. There was one procedural death, and 30-day mortality was 9.6%. The incidence of stroke was 1.9% (six patients) and 44 patients (15.6%) required a new permanent pacemaker. Median postoperative hospitalisation was 10 days. Low access site complications and low stroke rate were two obvious highlights of this data. Also, more than 100 patients have been enrolled in the CoreValve pivotal trial in USA, the results of which will be available in the near future.
SAPIEN/SAPIEN XT RESULTS
Similar to the CoreValve experience, following the first successful procedure there have been several publications reporting experience with this approach.
The largest reported series comprised ninety-four consecutive patients with unfavourable peripheral access22. Mean age was 84.1±5.4 years and logistic EuroSCORE 17.6±10.2%. All procedures were performed with Ascendra2 or older generations of the Ascendra system (Edwards Lifesciences), which did not have a nose cone. The SAPIEN XT was used in 88.3%. Device success rate was 92.6%. Paravalvular leak ≥2/4 was observed in 7.4%. Conversion to open chest surgery was required in 5.3% (three aortic dissections, one valve migration and one left main occlusion). Three cerebrovascular accidents (two transient ischaemia and one delayed stroke) were noted. Total hospital stay was 12.2±6.2 days. Thirty-day mortality and combined safety endpoint were reported in 7.4 and 16.0%, respectively. Thirteen patients with a mean age of 81 years underwent transaortic Edwards SAPIEN valve implantation at The Prince Charles Hospital, Brisbane, Australia23. Six of the 13 cases had previous coronary artery bypass surgery. Mean logistic Euroscore was 17.4. There was no in-hospital mortality, one patient required insertion of a permanent pacemaker for complete heart block. There were no aortic cannulation complications. Recently Lardizabal et al28 published in JACC a single-centre USA experience on forty-four consecutive patients with severe, inoperable aortic stenosis who underwent TAo SAPIEN implantation. Outcome data from the patients who underwent TAo were compared to those of patients who underwent transapical TAVI at the Miller School of Medicine, Miami, FL, USA. Transcatheter valve implantation (including vascular access, device deployment, and retrieval of delivery device) was successful in all patients of the TAo and TA groups. Two of the first five patients who underwent TAo TAVR sustained wire perforation of the left ventricle. One patient in the TAo group and two patients in the TA group died during the procedure. At 30 days, the combined safety endpoint of all-cause mortality, major stroke, disabling bleeding, severe AKI, MI, major vascular complications, and repeat TAVR/SAVR was similar between the TAo and TA groups (20% vs. 33%, respectively; p=0.21). The rate of major bleeding was higher in the TA compared to the TAo group (28% vs. 11%, respectively; p=0.04), as was the incidence of total bleeding and vascular complications (46% vs. 27%, respectively; p=0.05). On average, patients in the TA group stayed twice as long in the ICU as the patients in the TAo group. They concluded that TAo approach was technically feasible and is associated with favourable outcomes.
COMPARISON WITH OTHER APPROACHES
In most centres performing TAVI, the TF approach is chosen before TA due to its less invasive nature. It is a common observation that the non-TF patient cohort has a higher EuroSCORE and a higher incidence of comorbidities. This partly explains the slightly inferior results of the TA approach when compared to the TF approach8. One of the advantages of the TA approach over all others is its antegrade nature. This has been suggested as the main contributing factor towards a lower incidence of stroke in these patients. Proponents of the TA approach often cite this as the main factor to balance the invasiveness of the approach. Interestingly, recent data emerging from the SOURCE XT registry, presented at EuroPCR 2013, demonstrated higher mortality, higher incidence of atrial fibrillation and a higher stroke rate in both unadjusted and adjusted cohorts in the TA group when compared to the TF group29.
This is not surprising as the TA approach is certainly more invasive in nature and, when compared to the TF approach, has three main drawbacks30-32. These contribute to the increased morbidity and mortality in these patients.
1. Access site problems: apical rupture and delayed pseudoaneurysm formation (Moving image 8).
2. Interference with postoperative respiratory dynamics due to thoracotomy.
3. Effects on left ventricular function due to purse-string suture on the ventricle.
There has been a slower adoption of the TS approach, which is intriguing. It may be because the subclavian artery is a less forgiving vessel, especially in elderly patients, and hence suitable only in selected patients. Furthermore, vascular complications such as rupture or perforation may be catastrophic in case of the TS approach. The TS approach may be more complex to learn, requiring additional investigations and experience in choosing the right patient, which limits its usage to very high volume centres33.
A TAo approach can potentially overcome these issues and may become important especially if there is a shift towards using this technology in lower-risk patients17.
1. Safety – all open heart operations are performed through a variation of a full sternotomy. Hence, exposure of the aorta is a common skill for a cardiac surgeon. Also, the majority of open heart operations are performed with cannulation of the aorta with two purse-string sutures. This is also the technique employed for performing a TAo TAVI. Aortic tear and dissections arising from such cannulation are extremely rare and are easier to deal with than a ventricular tear.
2. Respiratory function – TAo performed through a mini-sternotomy without opening the pleural cavities is the best approach in patients with poor respiratory function.
3. Left ventricular function -as the left ventricle is untouched, there is no adverse effect on the ventricular structure or function.
Further, the TAo approach may have some additional benefits.
1. Ability to go on cardio-pulmonary bypass (CPB) – CPB can easily be established with aortic and right atrial cannulation through a mini-sternotomy incision. This can either be done electively when the left ventricular function is poor or when faced with a complication such as left ventricle stunning or coronary obstruction.
2. Avoids the arch – this approach allows one to truly avoid the aortic arch as there is neither a delivery system nor a wire placement in the arch. This may translate into lowering the incidence of stroke. If needed one can also place the pigtail catheter through the ascending aorta.
3. Avoids the mitral valve – there are no purse-strings on the ventricle and no possibility of mitral chordae entanglement as in a TA approach.
a. Tactile feedback – tactile feedback and finer control over positioning of the TAVI device is possible due to proximity to the aortic annulus.
b. Ability to perform hybrid procedures in combination as explained above.
Contraindications
The only contraindications for this approach are a complete porcelain aorta where there is presence of calcium in the TAo zone, and when the ascending aorta is not accessible e.g., anatomical deformity of the chest wall or radiation to the chest wall.
Future outlook
The TAo approach for TAVI is feasible and safe. It mimics the TF approach and hence is less invasive than the TA approach as it does not interfere with left ventricular function and interferes minimally with respiratory function. It also has the added benefit of familiarity amongst most cardiac surgeons, thus taking away a significant proportion of the learning curve of the TAVI procedure. It is versatile enough to be performed as part of a hybrid procedure. Although the current experience is limited to the SAPIEN and CoreValve, dedicated delivery systems will soon be available for other TAVI devices. Hence, TAo will continue to be an important approach in the future for the TAVI procedure.
Conflict of interest statement
V. Bapat is consultant for Edwards Lifesciences, Medtronic Inc., St. Jude Medical and Symetis, and G. Bruschi is consultant for Medtronic Inc.
Online data supplement
Moving image 1. First successful case of Edwards SAPIEN implantation with the Ascendra 1 system. Note that this system has no nose cone.
Moving image 2. SAPIEN XT implantation with the Ascendra+ system. Note that this system has a nose cone which facilitates retrograde crossing of the aortic valve
Moving image 3. Valve-in-valve implantation with CoreValve in a degenerated Mitroflow through right anterior thoracotomy TAo approach.
Moving image 4. SAPIEN XT implantation in presence of mechanical mitral prosthesis.
Moving image 5. LIMA to LAD graft lying left side of the sternum.
Moving image 6. RIMA injection demonstrating it crossing the midline.
Moving image 7. Room set up moving image.
Moving image 8. Example of delayed LV apex aneurysm following transapical approach.

