In this chapter of Tools and Techniques - Clinical: the transaortic approach through a mini-sternotomy using the self-expandable CoreValve® Revalving System (Medtronic Inc., Minneapolis, MN, USA) are discussed using a stepwise approach. The following is a summarised overview of this technique. The complete, unabridged version with images is available online at www.eurointervention.org.
Background and indications
The transaortic approach (TAo-TAVI) is a recently developed surgical technique to perform transcatheter aortic valve implantation (TAVI) in either high-risk or inoperable patients. TAo-TAVI is predominantly reserved for patients in whom the vascular anatomy does not allow transfemoral valve implantation, and in whom subclavian or transapical implantation is not feasible or desirable.
Technique, tips and tricks
Patients are positioned on the operating table exposing the anterior chest and the groins. Once femoral or radial artery access has been obtained, a pigtail catheter is advanced to the non-coronary leaflet of the aortic valve and left in position for aortographies throughout the procedure. A temporary pacemaker lead is inserted via the right femoral vein into the right ventricle.
TAo-TAVI can be performed through an upper “J” median hemisternotomy or a limited right anterior thoracotomy. After this, the aorta is dissected free from its surroundings and exposed.
Using a graduated pigtail catheter under fluoroscopy, the surgeon can assess the distance between the cannulation site and the aortic annulus by placing a forceps at the desired position of entry. The minimum distance we use is 7 cm. Two purse-string sutures are placed at the desired location on the lateral aspect of the aorta (Figure 1). The aortic wall is then punctured and a short wire is advanced.
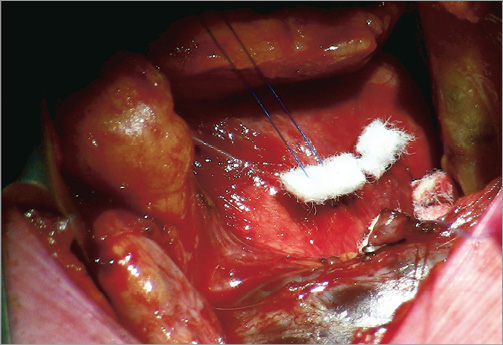
Figure 1. Purse-string sutures on the lateral aspect of the aorta.
A 6 Fr sheath is advanced over the wire in the aorta. The native valve is then crossed into the left ventricle with a straight, preferably non-hydrophilic wire. This wire is followed by another pigtail into the left ventricle, removed and replaced by an Amplatz Super Stiff™ wire (Boston Scientific Corp., Natick MA, USA) or an Amplatz Extra-Stiff (Cook Medical, Bloomington, IN, USA) wire whose tip has previously been re-shaped in order to avoid ventricular perforations. A short ring of plastic tubing is cut off and mounted on the 18 Fr sheath of the delivery system (GORE® DrySeal; W. L. Gore & Associates Inc., Newark, DE, USA) 2 cm from its tip. This “stop ring” prevents the sheath from moving too deep in the aorta and leaves enough distance for deployment of the valve. The 18 Fr sheath is advanced over the stiff wire into the aorta (Figure 2). Predilatation of the aortic valve is usually performed under rapid pacing, but this can often be omitted because a direct approach allows for a more meticulous valve placement.
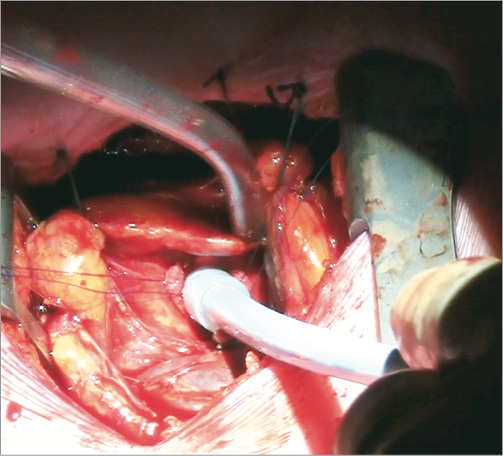
Figure 2. 18 Fr sheath and its stop ring inserted into the ascending aorta.
Under fluoroscopy and direct tactile and visual feedback the self-expandable valve is slowly released. The delivery system should approach the aortic annulus perpendicularly, which can be difficult to achieve particularly when the aorta is short or curved. In these cases the surgeon can, under fluoroscopy, manipulate the sheath and the ascending aorta obtaining the required implant angulations. After valve implantation, LV and aortic pressures are recorded to assess the gradient and paravalvular leakage. A final supravalvular injection is made 10 minutes after placement. If the result is satisfactory, the sheath can be withdrawn with tying of the purse strings. Chest closure is performed in classical fashion with steel wires, using a protection tool to avoid injury to the underlying structures and leaving wound and pleural drains when required.
Conflict of interest statement
A.P. Kappetein is a principal investigator of the SURTAVI trial, which is sponsored by Medtronic. The other authors have no conflicts of interest to declare.

