Abstract
Aims: We aimed to evaluate the contribution of the retrograde approach to real-world practice over time and its long-term outcomes in chronic total occlusion (CTO) percutaneous coronary intervention (PCI).
Methods and results: We evaluated 1,635 CTO procedures conducted at our high-volume centre between 2003 and 2015. The retrograde approach has been actively adopted in practice since January 2007. The primary endpoint was target vessel failure (TVF), a composite of cardiac death, target vessel-related myocardial infarction, or target vessel revascularisation/reocclusion. The technical success rate of CTO-PCI has increased from 79.5% to 87.1% since 2007, although the complexity of the CTOs has also significantly increased in that time (J-CTO scores: from 1.8±1.2 to 2.0±1.1, p=0.03). The incidence of in-hospital MACCE using the retrograde approach was 4.5%, which was comparable to the antegrade-only approach rate of 4.1% (p=0.58). The retrograde approach showed a higher four-year TVF rate after successful stenting compared with the antegrade-only approach (17.1% vs 9.4%, p=0.01), but this difference was mainly driven by a higher target vessel revascularisation/reocclusion rate. Multivariable analysis revealed that renal dysfunction (hazard ratio [HR] 3.33, 95% confidence interval [CI]: 1.42-7.83), acute coronary syndrome (HR 1.99, 95% CI: 1.26-3.14), the J-CTO score (per 1, HR 1.23, 95% CI: 1.00-1.51), and the smallest stent diameter (per 1 mm, HR 0.39, 95% CI: 0.21-0.74) (all p<0.05) were independently associated with TVF.
Conclusions: A retrograde approach contributes to the increased success of more complex CTO-PCI over time with an acceptable frequency of in-hospital complications and four-year TVF rate.
Introduction
Coronary chronic total occlusion (CTO) is observed in approximately 15-30% of patients referred for cardiac catheterisation and has long been considered one of the most challenging lesion subsets for percutaneous coronary intervention (PCI)1. Dedicated devices and techniques have become available during the past decade and have allowed operators to overcome some of the previous difficulties with the CTO-PCI procedure. The worldwide expertise and experience with CTO-PCI has also steadily increased through effective training programmes and conferences, thereby enabling clinicians to deal with more complex CTOs.
The retrograde approach through collateral circulation was a revolutionary technical breakthrough in CTO-PCI2. Combined with the use of new microcatheters working as a channel dilator and the controlled antegrade and retrograde subintimal tracking (CART) technique, CTO-PCI procedures using a retrograde approach have produced an increasingly higher technical success rate in experienced centres2. The retrograde approach has now been rapidly adopted worldwide despite the possibility of some complications attributed to its inherent methodology. Until recently, however, the information on how this approach has contributed to CTO-PCI practice over time has largely been limited. In addition, the long-term results of successful PCI using a retrograde approach are not well known. We therefore evaluated the contributory role of the retrograde approach to CTO-PCI and associated long-term outcomes in comparison with cases treated using only the antegrade approach.
Methods
STUDY POPULATION
The study population was obtained from the Asan Medical Center-CTO registry which has prospectively collected data on consecutive patients undergoing CTO-PCI since March 2003. Only patients who underwent CTO-PCI between January 2007 and June 2015 were included in the outcome analyses as this was the period during which the retrograde approach was actively performed at our centre. Although all operators at our institution have participated in CTO-PCI, these procedures have mainly been performed by three dedicated CTO operators (S.W. Lee, J.Y. Lee, P.H. Lee). This study was approved by the institutional review board of Asan Medical Center and all participants provided written informed consent.
DEFINITIONS AND STUDY OUTCOMES
A CTO was defined as a complete coronary obstruction with a Thrombolysis In Myocardial Infarction (TIMI) flow grade of 0 and an estimated duration of more than three months. If the duration of the occlusion was not clear from the medical information, the diagnosis was made based on angiographic findings, as suggested by the Euro CTO Club consensus document1. The PCI procedure was defined as a retrograde approach if an attempt was made to cross the collateral channel supplying the vessel distal to the target CTO lesion. The procedure was otherwise classified as an antegrade-only approach. The general indications for adopting a retrograde approach included a proximal cap ambiguity, a distal vessel of poor quality or bifurcation, or the presence of interventional collaterals3. Technical success was defined as a restoration of TIMI 3 flow with a residual diameter stenosis ≤30% within the treated segment, as determined by angiographic assessment. Procedural success was defined as the achievement of technical success without any in-hospital major adverse cardiac or cerebrovascular events (MACCE). In-hospital MACCE included any of the following adverse events prior to hospital discharge: death from any cause, periprocedural myocardial infarction (MI), urgent target vessel revascularisation with PCI or bypass surgery, tamponade requiring intervention, and stroke4.
The primary outcome of interest in this study was target vessel failure (TVF), defined as a composite of cardiac death, target vessel-related MI, or target vessel revascularisation (TVR)/reocclusion. Death was considered to be of cardiac cause unless an unequivocal, non-cardiac origin was documented. Periprocedural MI was defined as a peak elevation of the creatine kinase-myocardial band of more than tenfold above the upper reference limit within 48 hours after the procedure5,6.
DATA ACQUISITION
Clinical, procedural, and outcome data were recorded in dedicated databases by independent research personnel6. Follow-up information regarding outcomes was obtained from out-patient visits, telephone interviews, and from the medical records of other hospitals as necessary. All baseline and procedural coronary angiograms were analysed independently by researchers in the angiographic core laboratory. The CTO length and total lesion length around the target CTO were determined from analyses of digital angiograms using an automated edge detection system (CAAS 5.7; Pie Medical Imaging, Maastricht, the Netherlands). CTO lesion complexity was assessed by calculating the Japanese-CTO (J-CTO) score for each case7.
STATISTICAL ANALYSIS
Continuous variables were compared using the Student’s t-test or the Wilcoxon rank-sum test and categorical variables using χ2 statistics or Fisher’s exact test, as appropriate. Cumulative event rates and survival curves were generated using the Kaplan-Meier method with the log-rank test. Owing to the different durations for the different techniques used, follow-up was censored at the date of the last follow-up or at 4.0 years, whichever came first. If an antegrade-only approach and a retrograde approach were used for separate CTO lesions in the same patient, these cases were assigned to the retrograde approach group, and the vessels treated via the retrograde approach were considered target vessels in the outcome analyses. Cox proportional hazards regression analysis was performed to identify primary outcome predictors. Candidate predictors included patient age, diabetes mellitus, renal dysfunction, clinical diagnosis of acute coronary syndrome, left ventricular ejection fraction, CTO located in the left anterior descending artery, J-CTO score, total stent number and smallest stent diameter. The final model was determined using a backward stepwise elimination procedure where the least significant variable was removed one at a time from the full model. P-values were two-sided, and p-values <0.05 were considered significant. Data analyses were performed using R software version 3.2.2 13 (R Foundation for Statistical Computing, Vienna, Austria; www.r-project.org).
Results
TREATMENT TRENDS, CTO COMPLEXITY, AND TECHNICAL SUCCESS
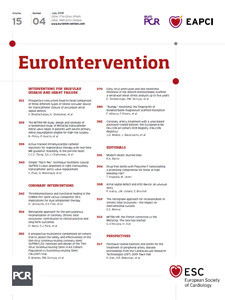
CTO-PCI was performed on 1,558 patients for 1,635 lesions at our hospital between March 2003 and June 2015 (Figure 1). The overall technical success rate during the entire period was 84.9% (failure occurred in 247 cases). The retrograde approach has been increasingly adopted since 2007 at our institution to deal with more complex CTOs. Since that time, this approach has been used in 21.1% of the 1,151 total procedures (243 cases), starting from 11.6% in the first two years to 25% and above each year thereafter. Compared to the period from 2003 to 2006, the overall complexity of CTOs showed a significant increase after 2007, as reflected in the higher average J-CTO scores (1.8±1.2 vs 2.0±1.1, p=0.03). Nevertheless, the overall technical success rate has also increased from 79.5% in 2003 to 2006 to 87.1% after 2007 (Figure 2). Among the CTO cases treated after 2007, the average J-CTO scores for the retrograde and antegrade-only approach were 2.6±1.0 and 1.8±1.0 (p<0.001), respectively. Of note, the average J-CTO scores for each strategy remained similar but the corresponding success rates for both approaches have significantly increased over time (Figure 3).
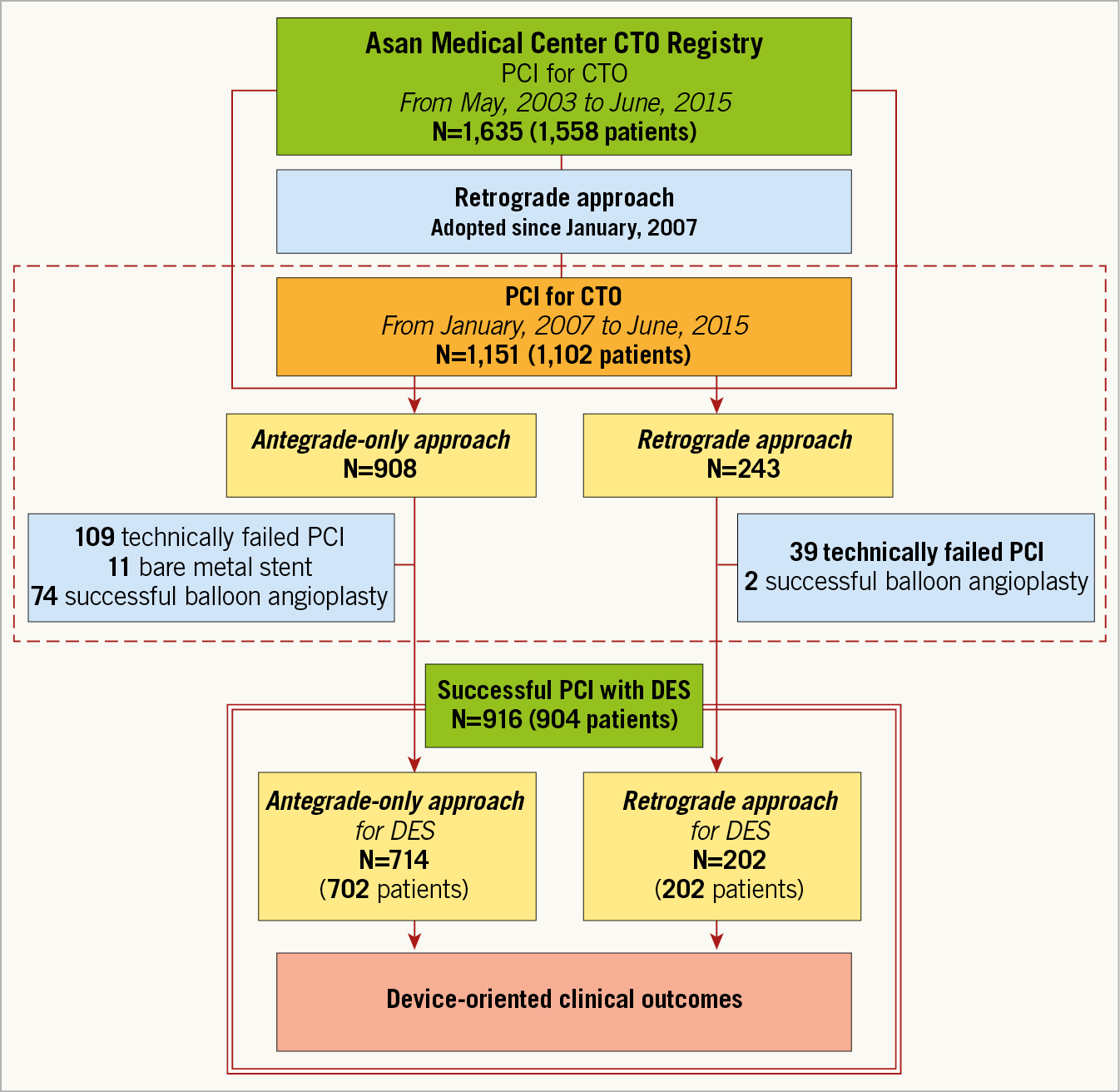
Figure 1. Study flow chart. The single solid line on top indicates the Asan Medical Center CTO registry to analyse treatment trends and technical successes over time. The dotted line denotes the patient population used to assess in-hospital outcomes of CTO-PCI since 2007. The double solid line at the bottom indicates the patient population used to analyse the long-term clinical outcomes of a successful CTO-PCI with DES. CTO: chronic total occlusion; DES: drug-eluting stents; PCI: percutaneous coronary intervention

Figure 2. Technical success rates before and after adoption of the retrograde approach. CTO: chronic total occlusion; J-CTO: Japanese-CTO; PCI: percutaneous coronary intervention
Figure 3. Average J-CTO score and technical success rate trends. CTO: chronic total occlusion; J-CTO: Japanese-CTO
PROCEDURAL SEQUENCE AND IN-HOSPITAL OUTCOMES
The retrograde approach was used as an initial strategy in 141 of the total number of cases that underwent this procedure (58.0%), and after a failed antegrade attempt in the remaining 102 cases (42.0%). Among cases of successful PCI using the retrograde approach, the final crossing techniques were as follows: CART or reverse CART in 46.4%, direct true lumen passing in 34.0% and the wire mark technique in 19.6%. When dividing the population of patients who underwent the retrograde approach into two period groups (period 1, 2007-2010; period 2, 2011-2015), the reverse CART technique has become significantly more popular while retrograde failure or halt has decreased. In addition, the use of epicardial collaterals has become more frequent (Supplementary Table 1).
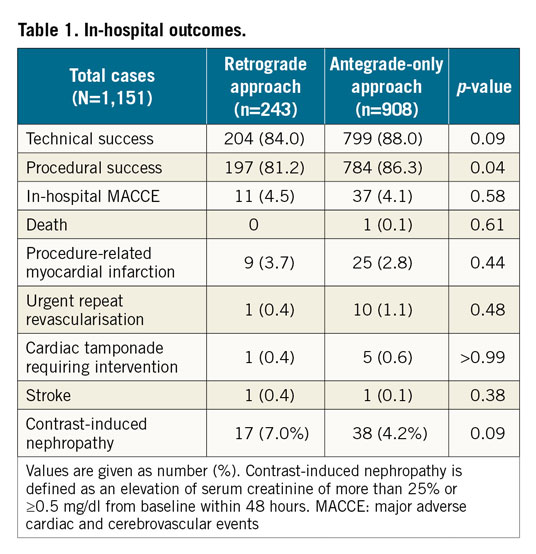
Table 1 summarises the procedural and in-hospital outcomes of all 1,151 CTO-PCI cases performed at our hospital between 2007 and 2015. The technical and procedural success rates were 88.0% and 86.3% in the antegrade-only, and 84.0% and 81.2% in the retrograde approach group, respectively. The incidence of clinically relevant in-hospital MACCE did not differ between the antegrade-only and retrograde approach groups (4.1% vs 4.5%, p=0.75).
PATIENT AND PROCEDURAL CHARACTERISTICS IN THE SUCCESSFUL CASES
Between January 2007 and June 2015, 904 consecutive patients successfully underwent drug-eluting stent implantation for 916 CTO lesions (Figure 1). Among the 12 patients who underwent PCI for multiple CTO lesions, there were seven patients who received PCI using the antegrade-only approach for 14 multiple CTO lesions and five patients treated with a mixed antegrade-only and retrograde approach for 10 separate CTO lesions. The latter five patients were classified into our retrograde approach group, resulting in a final cohort of 202 patients (22.3%) who received PCI with the retrograde approach for 202 CTO lesions. The other 702 patients underwent PCI with an antegrade-only approach for 714 lesions and were assessed in parallel.
Detailed demographic and clinical characteristics of these patients are provided in Supplementary Table 2. Considerable differences in both the lesion and procedural characteristics were noted between these two groups (Supplementary Table 3). Both the CTO length and the total lesion length incorporating the CTO were significantly longer in the retrograde approach group, contributing greatly to the final numbers and lengths of the stents used.
CLINICAL OUTCOMES DURING FOLLOW-UP
During the pre-specified four-year follow-up period, the primary endpoint occurred in 85 patients (9.4%). Death occurred in 43 patients (4.8%), 24 of whom (2.7%) died of a cardiac cause. MI occurred in 36 patients (4.0%), with 26 (2.9%) of these cases having a target vessel-related MI. TVR/reocclusion occurred in 41 patients (4.5%). The clinical endpoints are listed in Supplementary Table 4 and Figure 4. Patients who underwent PCI using a retrograde approach had a significantly higher cumulative TVF rate (17.1% vs 9.5%, hazard ratio [HR], 1.79; 95% confidence interval [CI]: 1.13 to 2.83, p=0.01) compared to the antegrade-only cases. This difference was largely attributable to the higher incidence of TVR/reocclusion (9.4% vs 4.6%, HR 2.01; 95% CI: 1.06 to 3.84, p=0.03) in the retrograde approach group. Multivariable analysis of the entire population revealed that renal dysfunction (HR 3.33, 95% CI: 1.42–7.83, p=0.006), acute coronary syndrome (HR 1.99, 95% CI: 1.26–3.14, p=0.003), the J-CTO score (per 1, HR 1.23, 95% CI: 1.00–1.51, p=0.047), and the smallest stent diameter (per 1 mm, HR 0.39, 95% CI: 0.21–0.74, p=0.004) were independently associated with TVF at the four-year follow-up (Supplementary Table 5). On the other hand, when we divided the retrograde cases into two time periods (period 1, 2007-2010; period 2, 2011-2015) the lesions were more complex overall and the TVF rate was higher in period 2, albeit not statistically significant (14.7 vs 19.7%, p=0.46) (Supplementary Table 1). In addition, when we analysed the clinical outcomes of the retrograde approach according to the technique used, no significant differences were found in the in-hospital or long-term clinical outcomes (Supplementary Table 6).
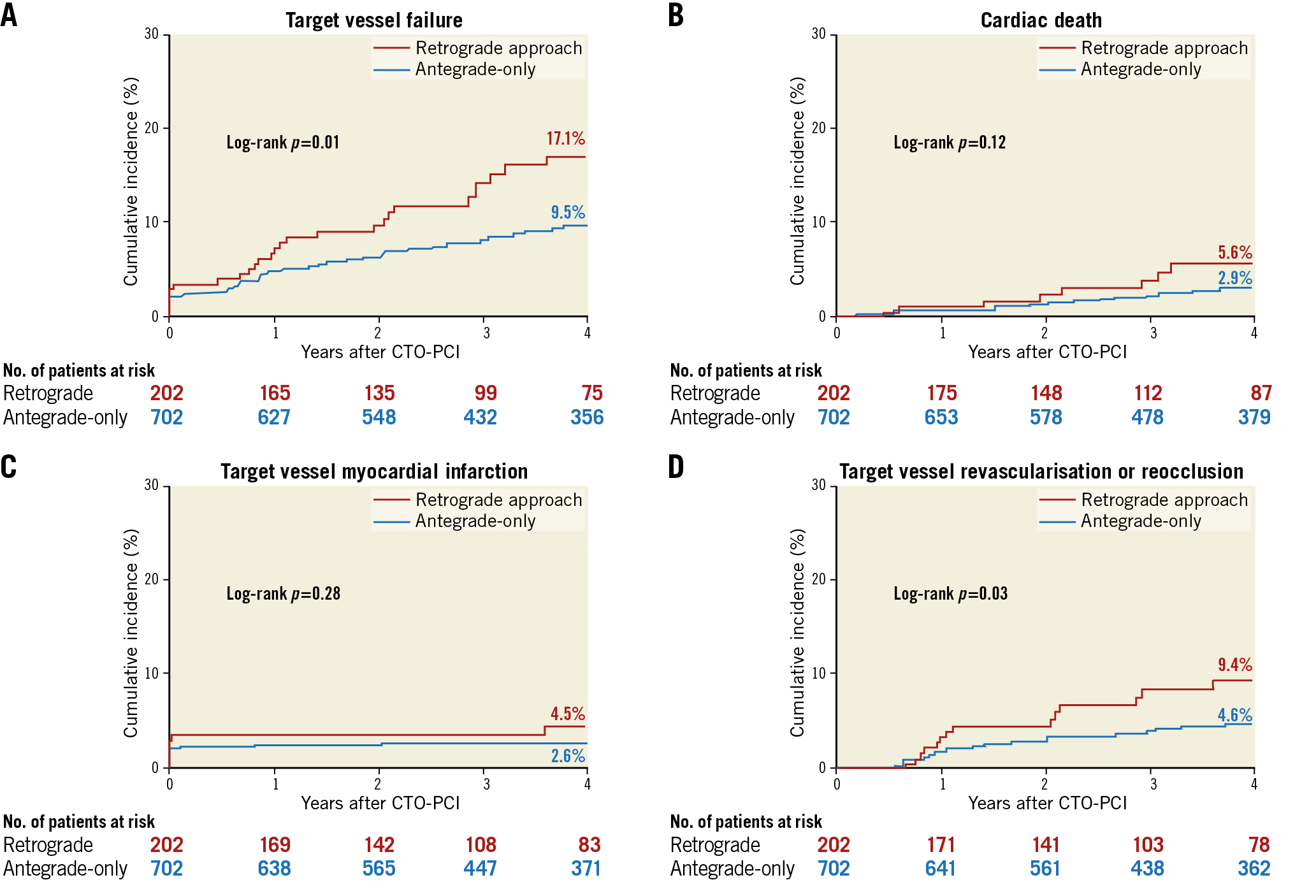
Figure 4. Kaplan-Meier event curves. Cumulative incidence of target vessel failure (A), cardiac death (B), target vessel myocardial infarction (C), and target vessel revascularisation or reocclusion (D). CTO: chronic total occlusion; PCI: percutaneous coronary intervention
Discussion
Our current analysis of consecutive CTO-PCI cases at our single tertiary referral centre revealed some important patient characteristics and outcome measures associated with the retrograde approach. The retrograde approach was found to be more commonly used for complex CTO lesions and contributed to their increased recanalisation rates over time. The in-hospital MACCE rate using the retrograde approach and the four-year TVF rate (17.1%) after successful stenting were acceptable, indicating that it is a safe option. The inevitable use of a smaller stent associated with a successful retrograde approach may be responsible for the future likelihood of TVF.
Over the past decade, in combination with the revolution in dedicated specific devices for CTO such as guidewires and microcatheters, various strategies including subintimal tracking and re-entry, a parallel wire technique, and intravascular ultrasound-guided wire crossing have been developed and have substantially contributed to the increasing procedural success rates of CTO-PCI. Of note, the retrograde approach has become an important technique for contemporary CTO-PCI practice and has been incorporated into algorithms for CTO crossing3,8. Recently, the findings from a multicentre CTO registry demonstrated a high technical success rate of 86% using the hybrid algorithm where the retrograde approach was applied in 34.9% of the successful cases9. Several other studies have also demonstrated the feasibility of the retrograde approach with an acceptably low level of in-hospital complications10,11. Importantly, our present data reinforce the contribution of the retrograde approach to the success of CTO-PCI, which rose from 79.5% to 87.1% after adoption of this technique despite a higher anatomic complexity. Furthermore, the success rate of the retrograde approach has increased significantly over time, reaching nearly 90% in recent years in cases with an average J-CTO score of 2.7. Combined with improvements in expertise, as reflected by the increased success rate of the antegrade-only approach over time, the aforementioned observations underline the importance of the retrograde approach in dealing with more complex and difficult CTO lesions.
There are limited data available regarding the long-term outcomes of successful PCI using the retrograde approach (Table 2),12,13,14,15. Michael et al reported the two-year outcomes of successful CTO-PCI using the retrograde approach and compared these with antegrade-only cases13. Of the 193 patients, 41 patients treated with the retrograde approach showed a higher incidence of target lesion revascularisation (45.6% vs 25.7%, p=0.006), but a similar incidence of death and MI was found in both groups. Galassi et al recently reported European experiences with the retrograde approach15. Among the 1,060 successful cases, the incidence of a composite of cardiac death, MI, stroke, and further revascularisation was 8.7% during a mean follow-up of 24.7 months. Overall, however, these few available studies have been of limited size or follow-up duration. Our present large-scale study thus provides important new insights into long-term stent-related outcomes of CTO-PCI performed with a retrograde approach.
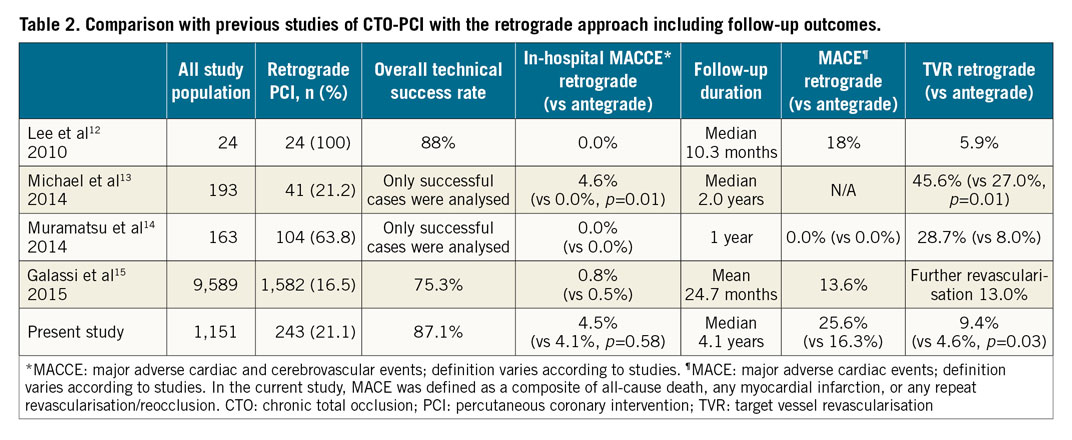
The performance of the drug-eluting stents implanted via the retrograde approach in our present cohort was acceptable given that the four-year rates of TVF and TVR/reocclusion were 17.1% and 9.4%, respectively. These results are comparable to those of previous coronary stent studies16 and other CTO-PCI studies17. However, these rates indicating stent failure were significantly higher than those seen in our antegrade-only group. A plausible explanation for the differences could be drawn from our multivariable analysis. In addition to certain other clinical factors, the J-CTO score and small stent diameter were found to be important lesional or procedural predictors of TVF in our cohort. CTOs constitute the most advanced form of atherosclerotic disease and are frequently accompanied by diffuse, long lesions and site calcifications. Hence, reopening a CTO commonly requires multiple, overlapping stent deployment with high-pressure balloon inflation to achieve a satisfactory angiographic result. This was particularly true for the CTOs requiring a retrograde approach, which typically showed a longer CTO length or total lesion length compared with the cases requiring antegrade-only approach in our present study series. This finding indicates that, in the retrograde approach cases, the more prominent diffuse atherosclerotic burden may inevitably lead to stenting in smaller calibre distal vessels. Consequently, the numbers and total lengths of the stents tend to be greater with smaller diameters in the retrograde approach cases. It would thus be reasonable to assume that the relatively unfavourable final results associated with a more complex anatomy and smaller stent implant may have led to some poorer outcomes in the retrograde approach group18,19. To reduce the potential risk of stent failure in this group, adjunctive therapies such as intensive medical treatments or thorough cardiac rehabilitation will be important.
Limitations
This study had several limitations of note. The first of these was inherent to the retrospective nature and observational design of the analyses. Second, the PCI policy of our hospital involves the routine use of intravascular ultrasound for stent optimisation where possible. This procedure was used in more than 90% of our current study patients, a considerably higher rate than that reported in other studies, which may have attenuated some of the drawbacks associated with the stenting of complex CTOs. Third, our sample population was drawn from a single high-volume centre with a certain level of expertise which predominantly uses wire-based techniques for CTO-PCI8. Patient risk conditions, CTO complexity, and the PCI strategies differ between centres and regions and this should be noted in relation to the general applicability of our findings. Finally, although the present study investigated four-year long-term clinical outcomes (median 4.1 years), complete four-year follow-up data were not available in 379 of the study cases (41.9%).
Conclusions
The retrograde approach contributes significantly to the increased recanalisation rates of more complex CTOs over time. The rate of in-hospital MACCE is low and the long-term device-oriented outcomes after successful stenting via this technique are acceptable. The unfavourable final stent results associated with complex anatomy in this patient population may be responsible for the future likelihood of TVF.
|
Impact on daily practice A retrograde approach has contributed significantly to an increase of the recanalisation success rates for more complex CTOs over time, confirming its substantial value for successful CTO-PCI. The retrograde attempt, reflecting the higher clinical and procedural complexity of CTO-PCI, was associated with a higher rate of TVF at long-term follow-up, mainly due to TVR/reocclusion. Given the potential hazard and clinical disadvantage (TVR) of the retrograde approach, subjects suitable for the retrograde approach should be assessed with careful deliberation by integrating the clinical and procedural factors. |
Funding
This study was supported by the Bio & Medical Technology Development Program of the NRF funded by the Korean government (NRF-2017R1A2B3009800 & NRF-2015R1A2A2A04003034), and by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI14C0517).
Conflict of interest statement
The authors have no conflicts of interest to declare.