Although mortality and morbidity from coronary heart disease have decreased in many countries, the complexity of the patients treated has increased, concomitantly with the continuous rise of patients’ age. In particular, two recent registries have reported a prevalence of coronary total occlusion (CTO) as high as 15-20% in the overall patient population undergoing coronary angiography1,2. In studies focusing on diabetes mellitus or heart failure3,4, the prevalence of CTO is greater than 40%. The presence of CTO influences the revascularisation strategy, with patients more often left on medical therapy or referred for coronary bypass surgery. This in turn modifies patient outcome.
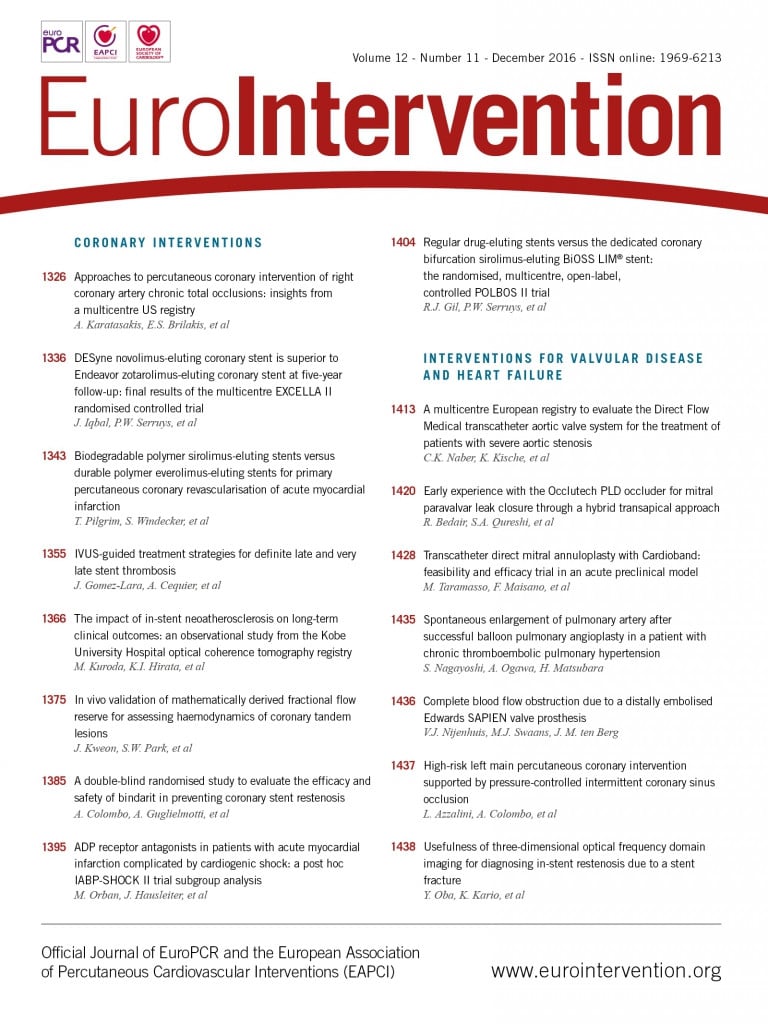
In this issue of EuroIntervention, there is a report by Karatasakis et al of a large contemporary US study of 739 patients with right coronary artery (RCA) occlusion5 which has an impact going beyond the technical aspects of the revascularisation procedure and which may influence clinical practice. The RCA is the most frequently treated vessel in CTO revascularisation, mainly because bypass surgery is more successful on the left anterior descending (LAD) artery than on the RCA. This makes surgery more appealing in patients with LAD CTO and creates a large group of patients with recurrent symptoms after occlusion of saphenous vein grafts (SVG) implanted on the RCA with persistent LIMA patency, a very poor target for redo CABG surgery. The success rate in the recanalisation of the RCA is known to be lower than in the LAD but higher than in the left circumflex (LCx) artery6. Tortuosity and length of occlusion are the key factors explaining the difference.
The article by Karatasakis et al explores success and indications of modern techniques of CTO revascularisation in a large cohort of patients (739) with very complex RCA occlusion (length 34 mm, 61% with moderate or severe calcification, 35% with moderate or severe tortuosity, J-CTO score 2.7±1.2). The key finding that should shake the beliefs and practice of the cardiology community is the success rate: 90.2% success in crossing with less than 30% final residual stenosis and TIMI 3 flow, 20 to 30 percentage points higher than the success rates reported in contemporary practice (54.7% in the 6,442 patients undergoing PCI for CTO in the SCAAR Registry7, and 59% in the 22,365 patients treated with PCI for CTO in the NCDR Registry8). What made the difference? A liberal utilisation of the retrograde approach and of anterograde dissection re-entry techniques, accounting for over 50% of cases in this series and hardly ever used in non-dedicated CTO centres. The dedicated material used is still not perfect and the retrograde approach alone is successful only in 62% of the cases attempted, mainly because the interventional collateral is too tortuous even for modern steerable wires or, more rarely, because the microcatheter is unable to follow. Similarly, the anterograde dissection re-entry technique, based on the utilisation of a flat balloon (Stingray™; Boston Scientific, Marlborough, MA, USA) directing a stiff needle towards the true distal lumen, has a low direct success (51%) but contributes to the overall improvement of results. The registry appears to confirm the value of the hybrid strategy proposed by Christopoulos et al9, i.e., an algorithm to decide the initial approach, based on the characteristics of the stump and length of occlusion, with a rapid switch out of a failure mode persisting in one approach to a move to other techniques.
Other groups outside the USA are approaching similar success rates. A consecutive series of 1,211 patients (2012-14) from seven UK centres showed a success rate of 87% using the same hybrid approach10. Many large Japanese CTO centres report greater than 90% success despite the lack of availability of the Stingray, with a trend towards an increased successful utilisation of an anterograde approach with escalation/de-escalation of the wires, including highly steerable tapered wires of limited stiffness (Gaia wires; ASAHI Intecc, Aichi, Japan) and simplification of the parallel wire technique using dual lumen catheters11. In Europe, the EuroCTO Club reported a progressive increase of success rates approaching 87% in 2015, with greater utilisation of a retrograde approach (35.1% in 2015 vs. 11.3% in 2010) as the most likely contributing factor12,13.
Despite these more aggressive approaches, periprocedural complications remained low and similar to literature data (1.6% in CTO PCI of the NCDR registry8 and 3.75% in a recent meta-analysis14).
Have we conquered CTO, the last challenge of PCI? Before bursting into overoptimistic celebrations, let us consider the main limitation of the study by Karatasakis et al5. It reflects the optimal practice of a selected group of high-volume operators sharing experience and with an unlimited access to costly devices and no difficulty in occupying a cathlab suite for an average of 98 min for the anterograde cases and 184 min for the retrograde cases. Outside Japan, we are rather pessimistic that we will see a widespread improvement to match such performances, unless the CTO technique is simplified and made shorter and accessible to less experienced PCI operators.
Conceptually, however, the success rate is sufficiently different from the previous practice to make obsolete the results of many trials comparing PCI with medical therapy or bypass surgery without approaching most of the CTO lesions and/or failing to open approximately 50% of the arteries15,16, e.g., in BARI 2D3, where CTO were left untreated in 38% of patients. In the 675 heart failure patients in the COMMIT-HF trial3, the investigators hardly ever tested viability in the territory of distribution of the occluded vessels, present in 41.2% of patients, and approached the occlusion with PCI in 3.5% of cases. The 10-year results of STICHES17 reversed the neutral outcome of the primary endpoint at five years, showing a significant reduction of mortality and rehospitalisation in the patients receiving revascularisation. Offering revascularisation to the many patients with ischaemic heart failure who are inoperable or too high risk for surgery may offer additional benefit on top of optimal medical treatment and cardiac resynchronisation therapy, and calls for new trials to be performed.
In recent years we have made a great deal of steady progress in CTO recanalisation but further work is needed to make success easier and more predictable. An equally daunting task will be to conquer the hearts and minds of our heart failure and general cardiology colleagues and change the conservative attitude towards occlusion treatment.
Conflict of interest statement
The authors have no conflicts of interest to declare.