Percutaneous revascularisation of chronic totally occluded coronary arteries is technically one of the most complex transcatheter procedures and represents 5% to 8% of all percutaneous coronary interventions (PCIs) performed (Figure 1)1,2. Its successful performance requires excellent interventional know-how and sophisticated dedicated equipment. During the last decade, chronic total occlusion (CTO) PCI has reached technical maturity. Various risk scores to predict technical success have been established, and a hybrid CTO PCI algorithm has been introduced. Use of the retrograde approach as a firm part of the CTO PCI algorithm resulted in a noticeable increase in the overall technical success rates – up to 90% in teams of very experienced operators3. The frequency of use of this approach as a final crossing strategy is between 24% and 35% in CTO PCI1,2,4,5.
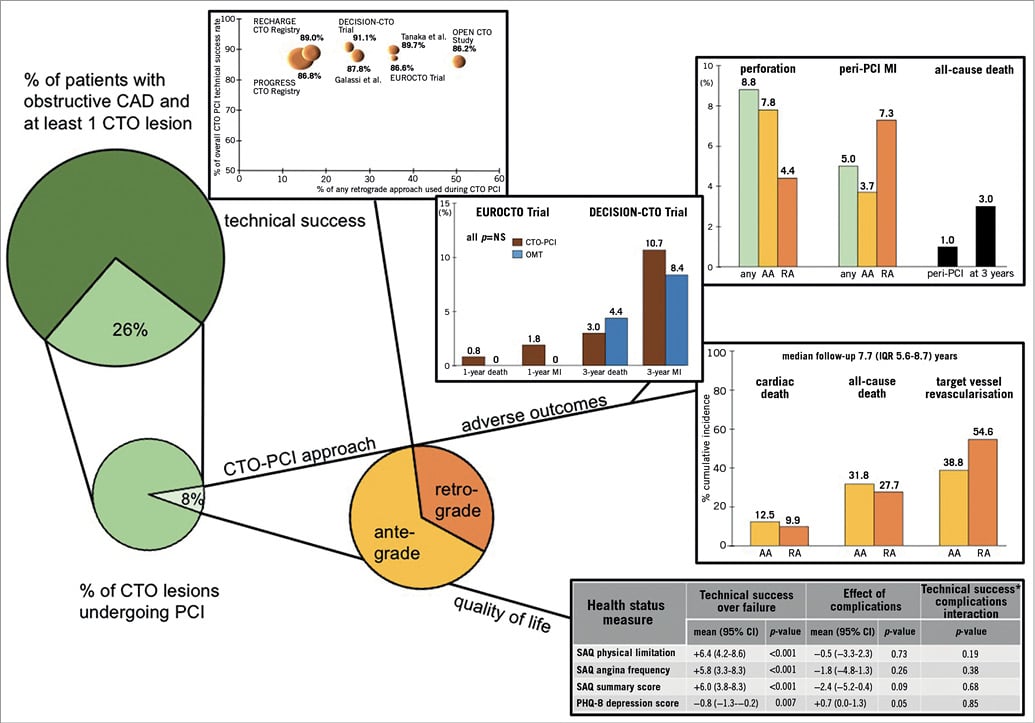
Figure 1. Chronic total occluded lesion frequency, percutaneous coronary intervention approach, its technical success and outcomes. AA: antegrade approach; CTO: chronic total occlusion; MI: myocardial infarction; PCI: percutaneous coronary intervention; RA: retrograde approach
Is the retrograde approach a guarantee of success?
The overall technical success rate reported for CTO PCI in various studies, including the OPEN-CTO study6 and the Kurashiki Central Hospital registry7, both published in this issue of EuroIntervention, is 87%.
Among patients undergoing the retrograde approach, direct retrograde wire crossing is reported as being between 40% and 61%7,8, reaching an overall technical success of 82%, which is lower than when the antegrade approach alone has been used (87%-94%). In this issue, Tanaka and colleagues (and others before) report that patients considered for the retrograde approach more frequently have a history of aorto-coronary bypass surgery, and half of them undergo reattempted CTO PCI and have a J-CTO score significantly higher compared to patients treated with the antegrade approach alone6-8.
Despite this, there is an encouraging body of evidence demonstrating an increase in the overall success rate of CTO PCI with the adoption of a hybrid algorithm, meaning the flexible use of the antegrade or retrograde approach3,8. Galassi et al reported the 10-year experience of one single CTO-dedicated operator who performed 1,073 CTO procedures between 2004 and 20143. They demonstrated an increase of the procedural success rate from 88% within the first five years of experience to 94% within the second five-year period, paralleling the increase in retrograde approach use from 20% to 32%. On the other hand, patients treated within the second five-year period more frequently underwent treatment of single-vessel coronary artery disease (CAD), less frequently had a history of bypass surgery and reduced LV function and, most importantly, 90% of the occluded arteries were well collateralised compared to 61% within the first five-year period3. We do not know whether there was an interaction between time period, patient selection and the retrograde approach CTO PCI success rate among the 842 CTO patients treated within a four-year period in Kurashiki Central Hospital7.
Is the retrograde approach safe?
Generally speaking, CTO PCI is associated with more periprocedural complications than non-CTO PCI. The overall core lab-adjudicated complication rate among 1,000 patients in the OPEN-CTO study was 9.7%, with 70% of these events occurring among patients undergoing retrograde approach CTO PCI6. Older age, J-CTO score and use of the retrograde approach were identified as predictors of complications in that study. The most common adverse events are perforations, reported in 8.6% of retrograde approach versus 5.4% of anterograde approach CTO PCIs7. The authors do not report any association between perforations and the use of rotational atherectomy. In this issue of EuroIntervention, Brinkmann et al report the frequency of use and complications related to rotational atherectomy among 14,947 non-occlusive and 2,972 CTO lesions in their institution9.
About 2.5% of both non-CTO and CTO lesions underwent rotational atherectomy. Among these carefully selected patients, the use of rotational atherectomy in CTO lesions (despite the presence of dissection planes) seems to be as safe as in non-occlusive lesions9. Another frequent complication reported in both studies was periprocedural myocardial infarction (MI), occurring in 2.6% and 5% of patients, respectively6,7. These patients have more than double the risk of death at long-term follow-up5. In a meta-analysis including 6,529 patients with CAD, patients with high collateralisation have a 36% reduced mortality risk compared to patients with low collateralisation10. Although few MIs are related to the compromised donor artery (<1%), this highlights the importance of operator experience in CTO PCI.
Is there a net clinical benefit with CTO PCI?
There are only three randomised trials in this field reporting either negative or inconclusive results1,11. Both the DECISION-CTO (n=815, 63% of the assumed sample size) and EUROCTO trials (n=396, 66% of the assumed sample size) failed to demonstrate differences in clinical adverse events among CTO PCI and optimal medical treatment up to three years of follow-up. While DECISION-CTO, presented at the American College of Cardiology Annual Scientific Session, March 2017, reported comparable measures of health-related quality of life among treatment strategies, the EUROCTO trial demonstrated greater improvement in the Seattle Angina Questionnaire (SAQ) subscales for angina frequency and quality of life with CTO PCI as compared with optimal medical treatment at one-year follow-up1. Within the setting of the OPEN-CTO registry, Riley and colleagues analyse for the first time the impact of technical success and peri-PCI complications on a variety of health status measures captured serially at baseline, 1-, 6- and 12-month follow-up. Patients with non-fatal peri-PCI complications reported a 3.7-point (95% CI: –0.64-–0.9; p<0.01) lower SAQ summary score and a 0.9-point (95% CI: 0.2-1.5; p<0.01) higher PHQ-8 depression score at 12-month follow-up compared to those without complications6. Interestingly, technical success was more strongly associated with quality of life outcomes than the presence or absence of complications (Figure 1). Unfortunately, no efforts have been made to investigate the characteristics of patients undergoing CTO PCI having no benefit in terms of health status measurements despite technical success without complications. Besides the type of CTO lesion, it is important to be able to select the patient who derives greater benefit regarding long-term wellbeing considering nearly prohibitive higher revascularisation rates, particularly when using the retrograde approach7. More randomised evidence needs to be accumulated in this complex, time- and resource-demanding field before CTO PCI can be extensively recommended.
Conflict of interest statement
J. Mehilli reports an institutional grant from Boston Scientific, and lecture fees from Edwards Lifesciences, Boston Scientific, Terumo and Siemens.