The revascularisation of chronic total coronary occlusions (CTO) has made huge progress with the introduction of new strategies for percutaneous coronary intervention (PCI). While the inability to treat a CTO had been the Achilles’ heel of the PCI approach to multivessel disease in the SYNTAX trial with a success rate of 49% as compared to 68% with surgery1, the reverse may now be the case. The recent SYNTAX II study showed that even in a multicentre study we can achieve 87% success, well above the level of coronary artery bypass graft surgery (CABG)2. This has been achieved mainly by incorporating modern CTO strategies, foremost among them being the retrograde approach. This technique, introduced by Dr Katoh and colleagues more than ten years ago3 and perfected with the availability of specific collateral wires and microcatheters, can be considered the major game changer4.
Both in SYNTAX II and in the randomised EuroCTO trial5, as well as in contemporary registries4,6, the percentage share of the retrograde procedure in achieving high success rates is in the range of 30-40% (Figure 1). However, the retrograde approach using the bilateral transcollateral access increases the complexity of the procedure and consequently the potential risks involved7. We add the risk of damage to the collateral and to the donor artery. This requires additional skills to deal with these potential complications, and a vigilant and careful approach to avoid these pitfalls. The retrograde approach is required with more complex lesions, and this entails some stretch of subintimal pathways and longer stents. This was demonstrated by the J-PROCTOR study a few years ago, with a trend towards a higher lesion recurrence rate in these complex cases8. However, data regarding the long-term outcome of retrograde procedures, especially beyond a one-year period, are scarce.
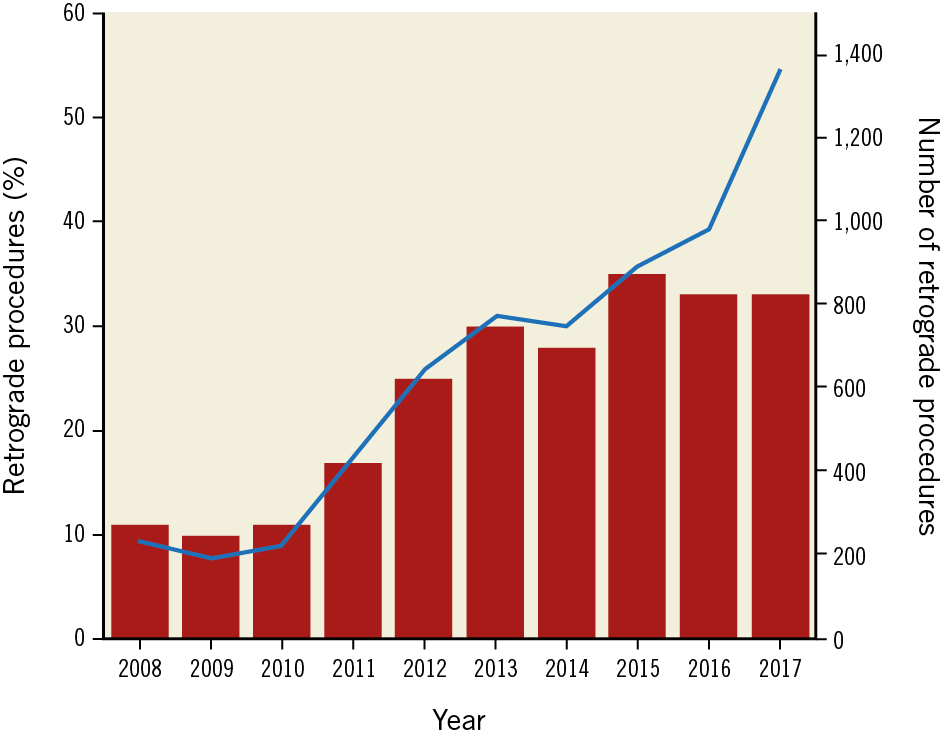
Figure 1. The adoption of the retrograde approach in the European CTO registry (ERCTO) as initiated by the EuroCTO Club and containing over 25,000 procedures between 2008 and 20174,7.
In this issue of EuroIntervention, the paper by Kwon et al9 from Korea shows the adoption of the retrograde approach within a single centre with dedicated operators and puts this into perspective with the clinical and long-term outcome as compared to the antegrade approach.
In 1,635 consecutive procedures observed over about 10 years, the authors saw an increase of the retrograde approach of up to 25%. The success rate increased with the introduction of the retrograde approach from below 80% to about 90% in their final observation period. This was not accompanied by an increased complication rate in this study and, most remarkably, they observed no periprocedural mortality in the retrograde group and only 0.1% in the antegrade group. This should be interpreted as indicating a careful case selection and the exclusion of high-risk patients rather than giving the impression that these procedures are without a mortality risk. In the contemporary OPEN CTO registry from the USA, with a higher rate of retrograde procedures and a more complex patient population (37% post-CABG patients), the periprocedural mortality was 0.9%10 in comparison to the present study where the rate of prior CABG was below 5%.
Kwon et al present a detailed analysis of their strategy and changes thereof over time, showing that reverse controlled antegrade and retrograde tracking (CART) increased to one third and retrograde wire crossing was used in one fourth of patients as the pathway to success; the epicardial route was chosen only in less than 20%. These are features attesting to a careful approach. However, with the latest collateral wires the use of the epicardial approach has tended to increase, and reverse CART takes a higher share of the retrograde approach6.
Despite moderate use of the retrograde approach, it must be noted that there is a clear difference in long-term major adverse cardiac events (MACE) attributable mainly to lesion recurrence. The difference in the steepness of the curves in their long-term follow-up shows that this may remain an ongoing problem. This is all the more notable as the study was conducted in a centre with a high utilisation of intravascular ultrasound (more than 90% in both groups). With this they achieved a four-year long-term patency of 91% after the antegrade approach, and 83% after the retrograde approach. The target vessel revascularisation (TVR) rate includes reocclusions; it is unfortunate that we do not learn the reocclusion rate per se, as it makes a difference for patient management if there is a lengthy stent occlusion or an easily manageable stent restenosis. The rate of reocclusions should be minimised as much as possible. The difference in outcome was attributable not so much to the retrograde mode, but to the fact that the retrogradely approached lesions were more complex and required longer stents and extension into smaller vessel diameters.
To conclude from this study that the retrograde approach per se has a higher long-term MACE rate would be to ignore the fact that lesion complexity drives the required approach, and extensive lesion coverage may explain the outcome. In general, the retrograde approach should follow an antegrade attempt; only rarely should it be the primary strategy (ostial lesions, very long lesions with ambiguous path, severe kidney dysfunction). In such cases, it is the decisive strategy to improve the procedural outcome, and also the clinical course5. The present study prompts us to bear in mind the long-term benefit, especially when we start to compete with surgery, beyond the one-year perspective. It is important to have more such well-conducted long-term studies to evaluate the differences in strategy on the clinical outcome.
Conflict of interest statement
The author has no conflicts of interest to declare.