Abstract
Aims: The aim of the study was to assess the long-term outcomes of coronary chronic total occlusion (CTO) lesions after retrograde percutaneous coronary intervention (PCI) in comparison with those after antegrade PCI alone.
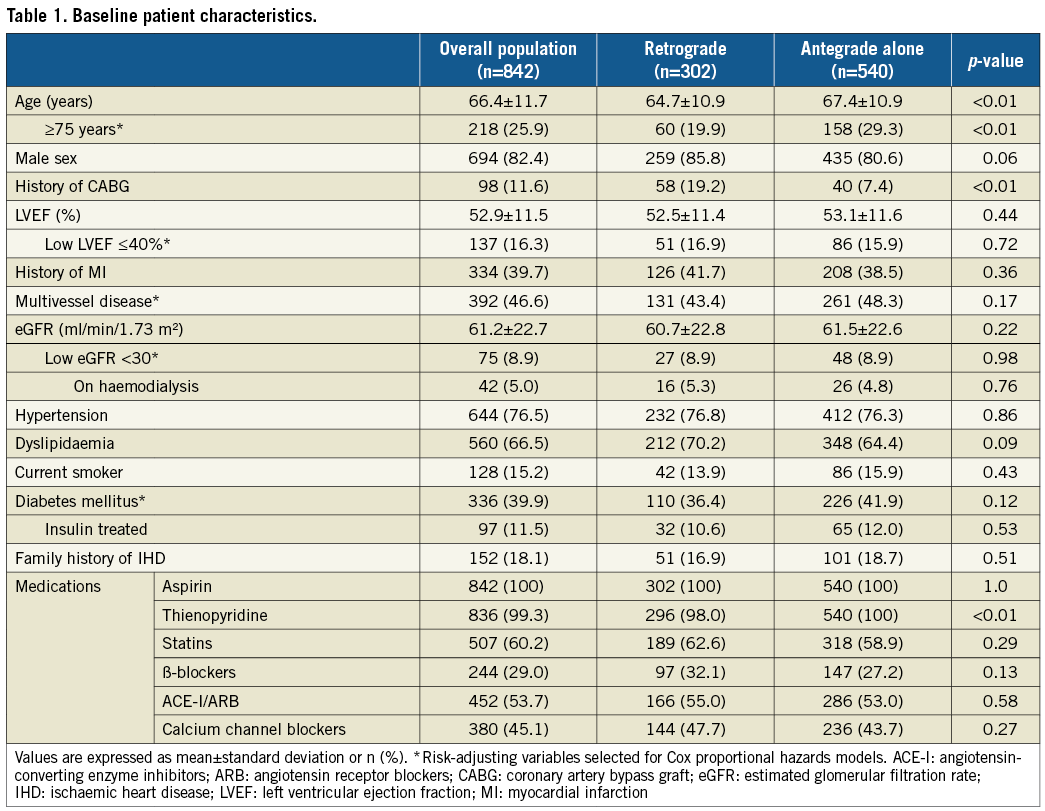
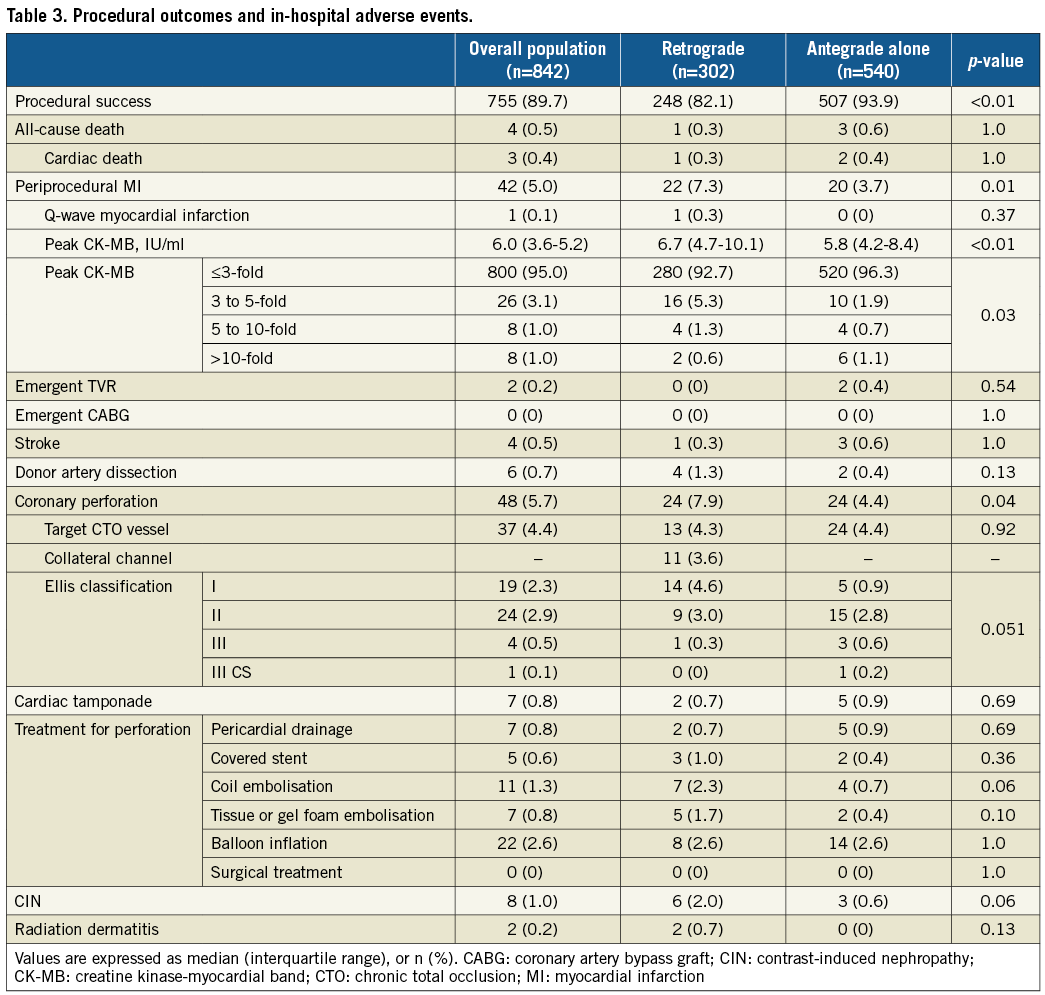
Methods and results: A total of 842 consecutive patients (928 CTO lesions) undergoing PCI and subsequent follow-up were classified into two groups: retrograde PCI for at least one CTO (n=302, retrograde group) and antegrade PCI alone (n=540, antegrade group). The total procedural success rate was 89.7%. The retrograde group had significantly higher incidences of periprocedural myocardial infarction and coronary perforation (7.3% vs. 3.7%, p=0.01; 7.9% vs. 4.4%, p=0.04, respectively). Median follow-up duration was 7.7 (interquartile range 5.6-8.7) years. Seven-year relative risk comparing the retrograde and antegrade groups was neutral in all-cause death (adjusted HR [aHR] 1.06, 95% CI: 0.75-1.49; p=0.745), cardiac death (aHR 0.85, 95% CI: 0.47-1.55; p=0.598), coronary artery bypass grafting (aHR 1.62, 95% CI: 0.74-3.54; p=0.229), and non-target vessel revascularisation (aHR 0.96, 95% CI: 0.78-1.17; p=0.663).
Conclusions: Retrograde CTO PCI did not lead to worse long-term outcomes despite increased risk in periprocedural myocardial infarction and coronary perforation.
Abbreviations
BMS: bare metal stent
CABG: coronary artery bypass grafting
CK-MB: creatine kinase-myocardial band
CTO: chronic total occlusion
DES: drug-eluting stent
MI: myocardial infarction
PCI: percutaneous coronary intervention
TVR: target vessel revascularisation
Introduction
Successful percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) lesions is associated with improvement in quality of life and left ventricular function, reduction in long-term mortality, and less need for coronary artery bypass grafting (CABG)1-6. The introduction of techniques such as the retrograde approach has contributed to the procedural success7-9. In patients undergoing the retrograde procedure using a coronary collateral circulation of the target occluded vessel, however, procedural complications such as collateral channel injury and donor artery dissection have been reported10,11. The aim of this study was to assess the long-term clinical outcomes of retrograde PCI in comparison with those of antegrade PCI alone in a consecutive series of patients undergoing CTO PCI.
Methods
STUDY DESIGN AND PROTOCOL
All patients undergoing PCI for at least one CTO lesion at Kurashiki Central Hospital between October 2005 and December 2009 were included in this study. We introduced the retrograde approach in October 2005. Data were prospectively entered into a clinical database at the time of PCI by the operator or the attending physician. The retrograde group included patients who had received the retrograde approach for at least one CTO lesion. The retrograde approach was indicated if a guidewire was inserted into a collateral channel from a donor vessel of the target CTO vessel. Regarding patients in whom CTO PCI was performed multiple times, if they were treated by the retrograde approach at least once, they were assigned to the retrograde group. The use of the retrograde approach was dependent on the operator’s discretion. Heparin was administered to achieve an activated clotting time of more than 300 seconds. An antiplatelet agent regimen consisted of aspirin indefinitely and thienopyridine (ticlopidine 200 mg or clopidogrel 75 mg daily) for at least 12 months after drug-eluting stent (DES) implantation and at least one month after bare metal stent implantation or balloon angioplasty.
The study was carried out in accordance with the provisions of the Declaration of Helsinki and the guidelines for epidemiological studies issued by the Ministry of Health, Labour and Welfare of Japan. Informed consent was provided for research purposes. The study was approved by the institutional ethics committee.
DEFINITIONS AND STUDY ENDPOINTS
CTO was defined as coronary artery obstruction of Thrombolysis In Myocardial Infarction (TIMI) flow grade 0 that lasted more than three months. The duration of the occlusion was estimated from the onset of clinical events such as history of a sudden onset, aggravation of chest symptoms, or angiographic findings. Lesion complexity of a target CTO lesion was assessed using the J-CTO score12. Quantitative assessment was performed using a commercially available software package (QCA-CMS 6.0; Medis, Leiden, the Netherlands). The occlusion length was defined as the length from the proximal occlusion to the distal retrograde filling from contralateral collaterals. Multivessel disease was defined as the presence of at least one stenosis of >50% in another major branch. Death from uncertain causes and sudden death were regarded as cardiac death. Creatine kinase-myocardial band (CK-MB) levels of all the patients were measured before PCI and between 12 and 24 hours after PCI in all patients. Myocardial infarction (MI) was defined according to the Academic Research Consortium definitions13. Periprocedural MI was defined as CK-MB levels elevated to >3-fold the upper limit of normal. Coronary perforation was defined as medically treated perforation for any contrast pool or evidence of contrast leak into the myocardium, the cardiac chambers, and the pericardial space and was also defined as the combination of target CTO vessel perforation and collateral channel perforation. Contrast-induced nephropathy was defined as an elevation in the peak serum creatinine of ≥0.5 mg/dl from the baseline after PCI. Target CTO vessel perforation was defined as perforation in the major vessel and distal vessel branch of a target CTO vessel. Target vessel revascularisation (TVR) was defined as either PCI or CABG resulting from restenosis or thrombosis after successful PCI. Procedural success was defined as successful CTO recanalisation with final % diameter stenosis <50% by quantitative coronary angiography (QCA) and TIMI flow grade 3. We evaluated the following clinical outcomes: all-cause death, cardiac death, CABG, and non-target vessel revascularisation. Non-target vessel revascularisation was defined as PCI or CABG including staged PCI for a vessel other than the target CTO vessel.
Follow-up information was collected either by reviewing the hospital charts and medical records obtained from other hospitals or by contacting patients and/or their referring physicians. We checked the condition of the patients every year to ensure the accurate assessment of the clinical endpoints.
STATISTICAL ANALYSIS
Categorical variables are expressed as numbers and percentages, and were compared using the chi-square test. Continuous variables are presented as mean±standard deviation or median (interquartile range). Continuous variables were compared using the Student’s t-test or the Wilcoxon rank-sum test. Follow-up was censored at the last follow-up date. The cumulative incidence was calculated using Kaplan-Meier curves, and differences were assessed using the log-rank test. Cox proportional hazards models were constructed to adjust the potential confounders at seven years after the procedure. We evaluated the risk of retrograde PCI relative to that of antegrade PCI alone for individual endpoints, which were expressed as hazard ratios (HR) and 95% confidence intervals (CI). We selected variables with a p-value <0.1 in the univariate Cox models to determine the independent risk factors. The risk-adjusting variables in the Cox proportional hazards models included five clinically relevant factors, listed in Table 1. Proportional hazards assumptions for the variables were assessed on the plots of log (time) versus log (-log [survival]) stratified by each variable and were verified to be acceptable for all the variables. All statistical analyses were performed using IBM SPSS Statistics, Version 23 (IBM Corp., Armonk, NY, USA). All reported p-values were two-sided, and p-values of <0.05 were considered statistically significant.
Results
PATIENTS, LESIONS, AND PROCEDURAL CHARACTERISTICS
A total of 842 consecutive patients (928 CTO lesions) undergoing PCI and subsequent follow-up were classified into two groups: retrograde PCI (n=302, retrograde group) and antegrade PCI alone (n=540, antegrade group). Baseline patient and lesion characteristics are summarised in Table 1 and Table 2. In the retrograde group, the selected channels were septal in 170 lesions (53.3%), epicardial in 123 (38.6%), and bypass graft in 26 (8.2%). The ipsilateral collateral channel was used in 14 lesions. In successful channel crossing, retrograde direct wire crossing was performed in 100 lesions (40.0%), kissing wire in 60 (24.0%), controlled antegrade and retrograde tracking (CART) in 28 (11.2%), and reverse CART in 29 (11.6%)7,8. Balloon dilatation of the septal collateral channel was performed in 84 lesions (26.3%).
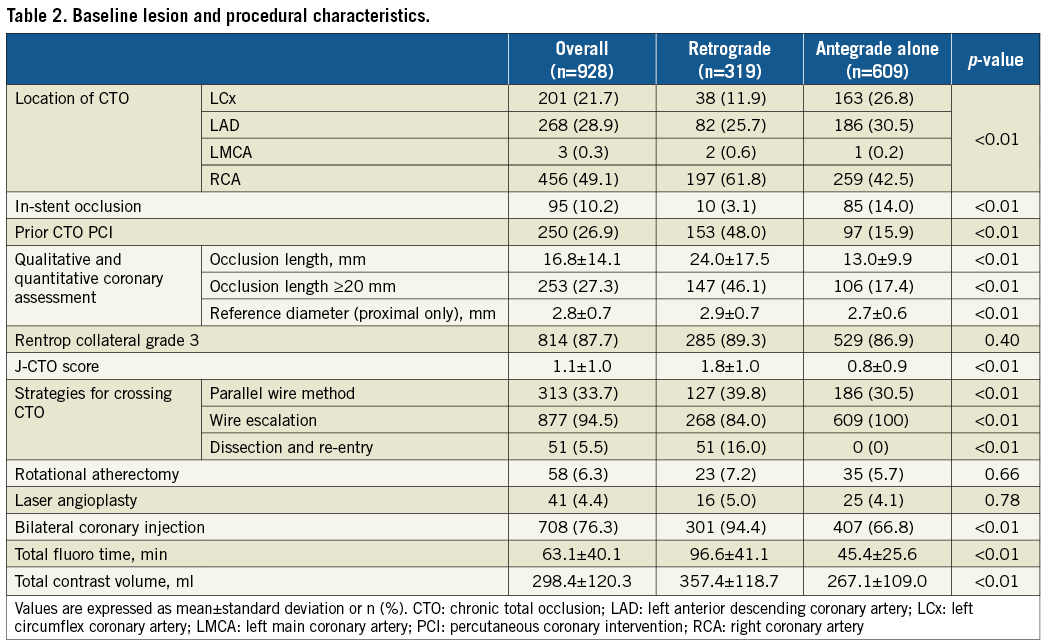
IN-HOSPITAL OUTCOMES
The procedural success rate of CTO PCI was 89.7%. The procedural success rate was significantly higher in the antegrade group than in the retrograde group (Table 3). Between the two groups, the retrograde group had significantly higher rates in periprocedural MI and coronary perforation, but there was no significant difference in periprocedural MI with >5-fold CK-MB elevation (2.0% vs. 1.9%, p=0.89) and Ellis classification grade Ш of coronary perforation (0.3% vs. 0.6%, p=1.0). In the retrograde group, four patients experienced dissection of the donor artery, two of them during contralateral injection before the retrograde approach.
LONG-TERM CLINICAL OUTCOMES
The median follow-up duration of surviving patients was 7.7 (interquartile range: 5.6-8.7) years. Clinical follow-up at seven years after the procedure was completed in 72.2%. The cumulative incidences in the retrograde group relative to those in the antegrade group were neutral for all-cause death (27.7% vs. 31.8%, p=0.549) (Figure 1A), cardiac death (9.9% vs. 12.5%, p=0.646) (Figure 1B), CABG (4.8% vs. 4.0%, p=0.446) (Figure 1C), and non-target vessel revascularisation (54.0% vs. 55.8%, p=0.338) (Figure 1D). The frequencies of non-target vessel revascularisation performed within 30 days after the procedure were 29.8% in the retrograde group and 35.7% in the antegrade group. The frequencies of non-target vessel revascularisation beyond one year were 1.8% per year in the retrograde group and 1.3% per year in the antegrade group. The univariate predictors of cumulative all-cause death at seven years are shown in Table 4. Even after adjusting for confounders, the incidences in the retrograde group relative to those in the antegrade group remained neutral for the above-mentioned four categories (Table 5). Baseline patient and lesion characteristics of a successful CTO PCI subgroup analysis are summarised in Supplementary Table 1 and Supplementary Table 2. The cumulative incidence of TVR was significantly higher in the retrograde group than in the antegrade group (54.6% vs. 38.8%, p=0.045) (Figure 2).
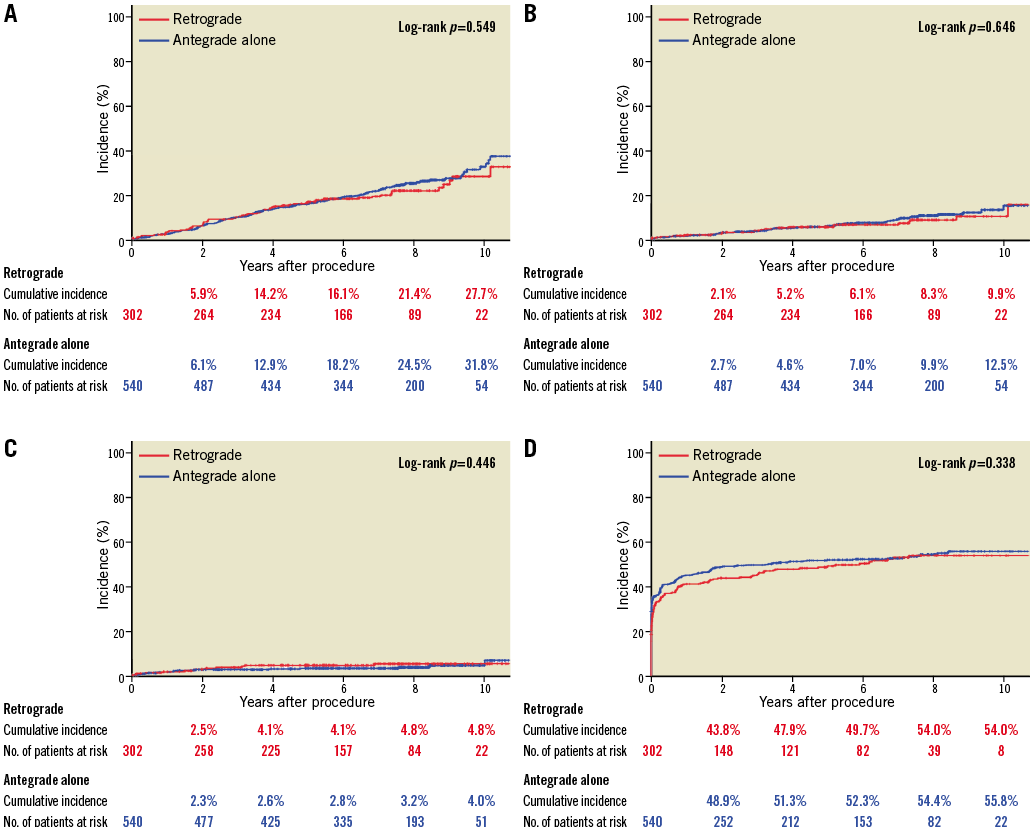
Figure 1. Cumulative incidences in the retrograde group relative to those in the antegrade group. A) All-cause death. B) Cardiac death. C) Coronary artery bypass grafting. D) Non-target vessel revascularisation.
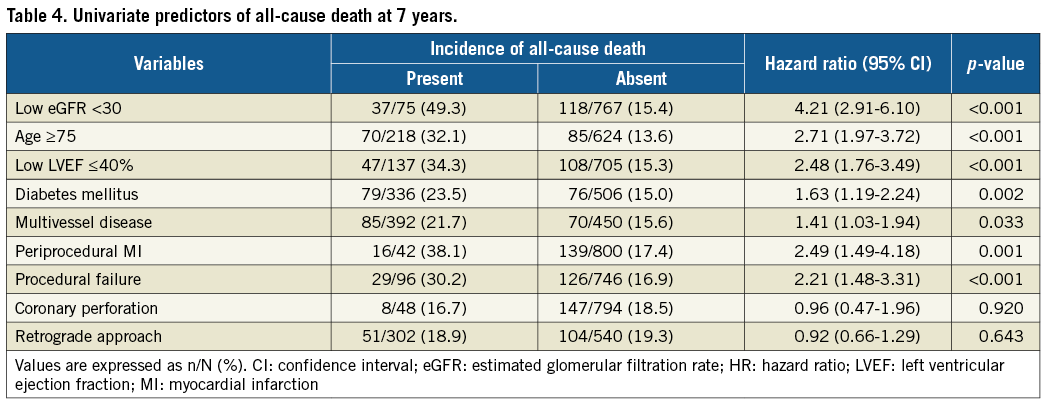
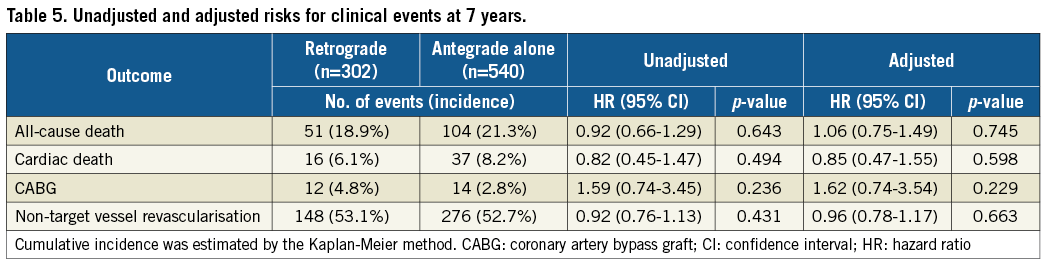
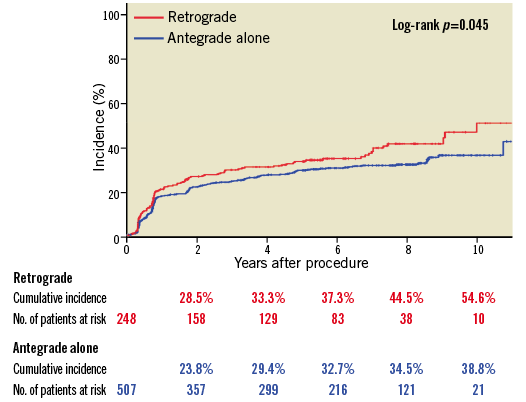
Figure 2. Cumulative incidences of TVR after successful PCI for CTO lesions in the retrograde group relative to those in the antegrade group. CTO: chronic total occlusion; PCI: percutaneous coronary intervention; TVR: target vessel revascularisation
Discussion
The main findings of this study are as follows: 1) retrograde CTO PCI in comparison with antegrade PCI alone was not associated with adjusted risks for all-cause death, cardiac death, CABG, and non-target vessel revascularisation during long-term follow-up, whereas the incidences of periprocedural MI and coronary perforation were significantly higher in patients undergoing retrograde PCI using a coronary collateral circulation of the target occluded vessel than in those undergoing antegrade PCI alone; 2) the incidence of TVR in successful CTO PCI was significantly higher in patients undergoing retrograde PCI than in those undergoing antegrade PCI alone.
Several studies have reported that complex retrograde procedures for CTO lesions, compared with antegrade procedures, led to an increased risk of periprocedural MI14,15. Recently, Lo et al have reported that periprocedural myocardial injury was more common with the retrograde approach than with the antegrade approach and was associated with worse subsequent clinical outcomes during midterm follow-up14. Furthermore, Lee et al have reported that periprocedural myocardial injury was associated with an increased risk of long-term mortality after successful CTO PCI, and some studies have reported that elevation of CK-MB levels after PCI was associated with an increased long-term mortality risk16,17. In our study, the incidence of periprocedural MI was higher after retrograde PCI than after antegrade PCI alone. A higher lesion complexity and a more complex recanalisation in the retrograde group might have resulted in a high incidence of periprocedural MI in the retrograde group in comparison with the antegrade group. However, increased mortality risk caused by the retrograde approach was not observed during long-term follow-up in our study, despite a high incidence of periprocedural MI. One reason may be that the number of 3- to 5-fold elevations in CK-MB levels after retrograde PCI was relatively greater than that after antegrade PCI alone; there was no significant difference in >5-fold elevation in CK-MB levels between the two groups.
Coronary perforation, a rare complication of PCI, is associated with a high risk of in-hospital mortality. Recently, Sapontis et al have reported that, in the OPEN-CTO registry, a registry for contemporary CTO PCI, perforation occurred in 8.8% of all cases, 4.8% of all cases required treatment for perforation, and the in-hospital mortality rate was 0.9%18. Coronary perforation needs to be promptly and appropriately managed, for which efficient preparation is essential. However, there have been few data on the long-term survival after coronary perforation associated with CTO PCI. Al-Lamee et al have reported that coronary perforation of Ellis classification grade Ш was associated with high acute and long-term rates of major adverse cardiac events19,20. Recently, Kinnaird et al have reported that coronary perforation associated with CTO PCI was observed with a legacy effect on the later mortality21. In our study, the incidence of coronary perforation requiring treatment was significantly higher in the retrograde group, but increased mortality risk associated with the retrograde approach was not observed during long-term follow-up. One reason may be that the incidences of feared coronary perforation of Ellis classification grade Ш and cardiac tamponade were low and there was no significant difference between the two groups.
In our study, the incidence of TVR after successful PCI during long-term follow-up was significantly higher in patients undergoing retrograde PCI than in those undergoing antegrade PCI alone. Michael et al have reported that the incidence of target lesion revascularisation during long-term follow-up was significantly higher in successful retrograde PCI than in successful antegrade PCI22. Some studies have reported a worse prognosis in lesions including higher J-CTO scores23,24. Moreover, longer total stent length using first-generation DES is reported to increase the incidence of target lesion revascularisation25. Additionally, first-generation DES implantation after a dissection and re-entry technique used in the retrograde approach may be associated with higher restenosis rates26. The fact that the retrograde group included patients with higher lesion complexity, more complex procedure, and a longer stent length than the antegrade group might have resulted in a higher incidence of TVR in the retrograde group than in the antegrade group.
Limitations
First, this is a non-randomised single-centre study with a relatively small sample size. Second, it has a selection bias because the selection of strategies was dependent on the operator’s discretion. Third, the underestimation of the presence of calcification and the degree of tortuosity due to a visual assessment might have been related to the relatively low J-CTO score. However, the J-CTO score of the retrograde group was significantly higher than that of the antegrade group. Fourth, the seven-year clinical follow-up results of 27.8% of the initial cohort were missing. Fifth, the study sample had fewer previous CABG histories, suggesting that this may be a lower-risk group than the general population. Sixth, the guidewires and the other devices used for CTO recanalisation have been improved. The procedural outcomes in the study period might be different from those in contemporary CTO practice. Finally, the incidence of TVR might differ between first- and second-generation DES, and first-generation DES were predominantly used in this study.
Conclusions
Retrograde PCI for CTO lesions did not lead to worse long-term clinical outcomes despite increased risks of periprocedural MI and coronary perforation. The incidence of TVR in successful CTO PCI was significantly higher in patients undergoing retrograde PCI than in those undergoing antegrade PCI alone.
| Impact on daily practice Retrograde PCI for CTO lesions has contributed to improving the procedural success rates and did not lead to worse long-term clinical outcomes despite increased risks of periprocedural myocardial infarction and coronary perforation. The incidence of TVR in successful CTO PCI was significantly higher in patients undergoing retrograde PCI than in those undergoing antegrade PCI alone using predominantly first-generation DES. We need to assess the long-term TVR in the second-generation DES of retrograde PCI for CTO lesions in comparison with antegrade PCI alone. |
Acknowledgements
The authors are very grateful to the late Dr Kazuaki Mitsudo for his guidance in the field of catheter intervention and would like to dedicate this paper to him.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Supplementary Table 1. Patient characteristics in successful PCI for a CTO.
Supplementary Table 2. Lesion and procedural characteristics in successful PCI for a CTO.
To read the full content of this article, please download the PDF.