Abstract
Aims: The aim of this study was to describe the epidemiology, mechanisms, management, and outcomes of coronary artery perforation during chronic total occlusion (CTO) percutaneous coronary intervention (PCI).
Methods and results: We included 1,811 consecutive patients undergoing CTO PCI at five centres between 2011 and 2018. Coronary perforation was observed in n=99 (5.5%). Patients with perforation were older, had a higher J-CTO score, more often required antegrade dissection/re-entry and the retrograde approach, and had lower success rates. The frequency of Ellis type I, II, III and III “cavity spilling” perforations was 11%, 46%, 28%, and 14%, respectively. In 48% of cases, perforation involved the CTO vessel, while the retrograde approach was responsible for 46% of cases. In 53% of cases perforations required intervention. The most frequently applied management strategies included clinical observation (47%), covered stent implantation (25%), balloon occlusion (9%), and coil/fat embolisation (9%). Tamponade was observed in 20/99 (20%) perforation cases. Ellis type III perforations were most frequently observed at the CTO site. These were accountable for 16/20 tamponades and 3/5 deaths. In-hospital mortality was 5.1% vs 0.3% in patients with versus those without perforation (p<0.001). Older age, occlusion length >20 mm, rotational atherectomy, antegrade dissection/re-entry, and the retrograde approach were independently associated with coronary perforation. Patients with perforation suffered an increased incidence of target vessel failure on short-term follow-up.
Conclusions: Coronary perforation is observed in a non-negligible proportion of CTO PCIs, often requires intervention, and is associated with tamponade and mortality in a minority of patients. CTO vessel-related perforations are associated with the highest burden of morbidity and mortality.
Introduction
Despite the remarkable advances witnessed in the past years, chronic total occlusion (CTO) percutaneous coronary intervention (PCI) remains associated with a non-negligible risk of complications1,2. Coronary perforation is one of the most feared complications of such interventions, with an incidence of up to 9%3. Indeed, treating a CTO is the strongest predictor of perforation in all-comers undergoing PCI4.
Coronary perforation can have life-threatening consequences in the acute setting, with tamponade (developing in up to 17%5), major bleeding, the need for emergent cardiac surgery, and in-hospital death5,6. Recently, it has been suggested that perforations during CTO PCI can also have a “legacy effect”, increasing the risk of all-cause mortality at one-year follow-up5. However, the available evidence on this topic is limited in terms of site-reported angiographic analysis6,7, lack of follow-up6, small sample size7, or lack of detailed angiographic data5.
The aim of the present study was to describe the epidemiology, mechanisms, management strategies, and outcomes of patients with coronary perforation during CTO PCI.
Methods
PATIENT POPULATION
This retrospective study included all patients who underwent CTO PCI at five centres in four countries (Italy, Germany, Spain, and the Netherlands) between July 2011 and October 2018. Baseline, procedural, and hospitalisation data were recorded from the electronic medical records. All patients signed an informed consent, approved by the local ethics committee, for procedural data collection and for the anonymous use of data for retrospective evaluation. The CTO PCI procedures were performed electively (ad hoc PCI was discouraged) following dual-catheter angiography, according to the principles of the hybrid algorithm1.
DEFINITIONS AND ENDPOINTS
CTO was defined as a 100% stenosis with a Thrombolysis In Myocardial Infarction (TIMI) flow of 0, and an estimated occlusion duration of ≥3 months8.
Technical success was defined as the achievement of <30% residual stenosis within the treated segment and restoration of antegrade TIMI 3 flow. Procedural success was defined as technical success without in-hospital major adverse cardiac and cerebrovascular events (MACCE)8, which included tamponade, stroke, major bleeding (causing a haemoglobin drop >3 g/dl and/or requiring transfusion, vasopressors, percutaneous or surgical intervention), periprocedural myocardial infarction (MI, defined according to the Society for Cardiovascular Angiography and Interventions definition9), and all-cause death.
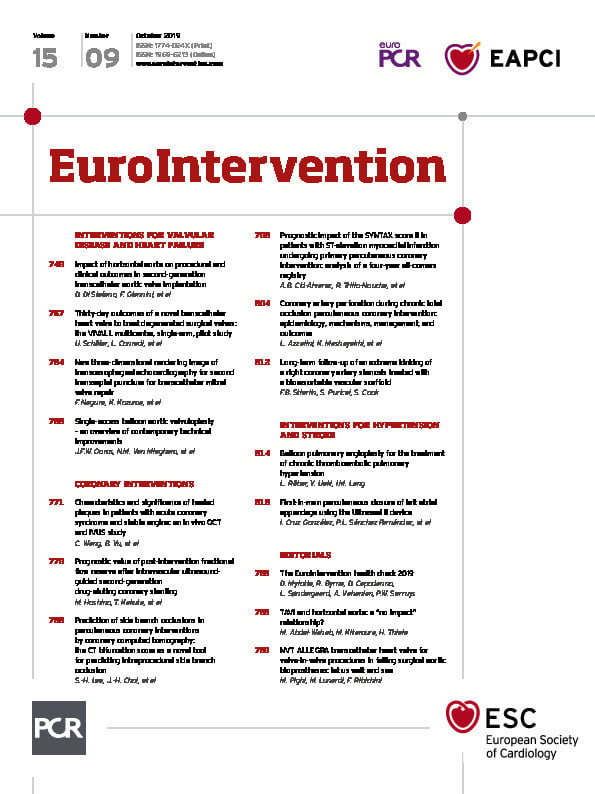
Perforations were classified according to their site (Figure 1) and mechanism (Figure 2). The Ellis classification was used to grade the severity of perforations: type I indicates extraluminal crater without extravasation; type II indicates pericardial or myocardial blush without contrast jet extravasation; type III indicates contrast jet extravasation through a frank (≥1 mm) exit hole; and type III cavity spilling indicates contrast jet extravasation into an anatomic cavity (e.g., cardiac chamber or coronary sinus)10. The occurrence of coronary perforation with the need for intervention (Figure 3) and tamponade was recorded. Coronary angiograms were reviewed by a central core laboratory (San Raffaele Scientific Institute, Milan, Italy) to provide a meticulous assessment of perforation diagnosis, mechanism, characteristics, management, and outcomes.
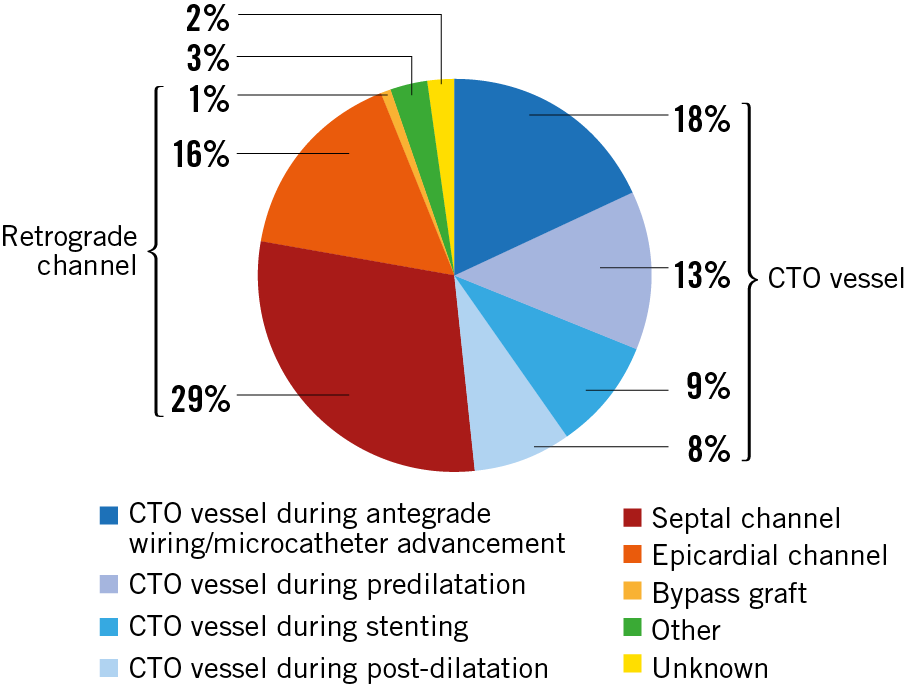
Figure 1. Sites of perforation during CTO PCI.
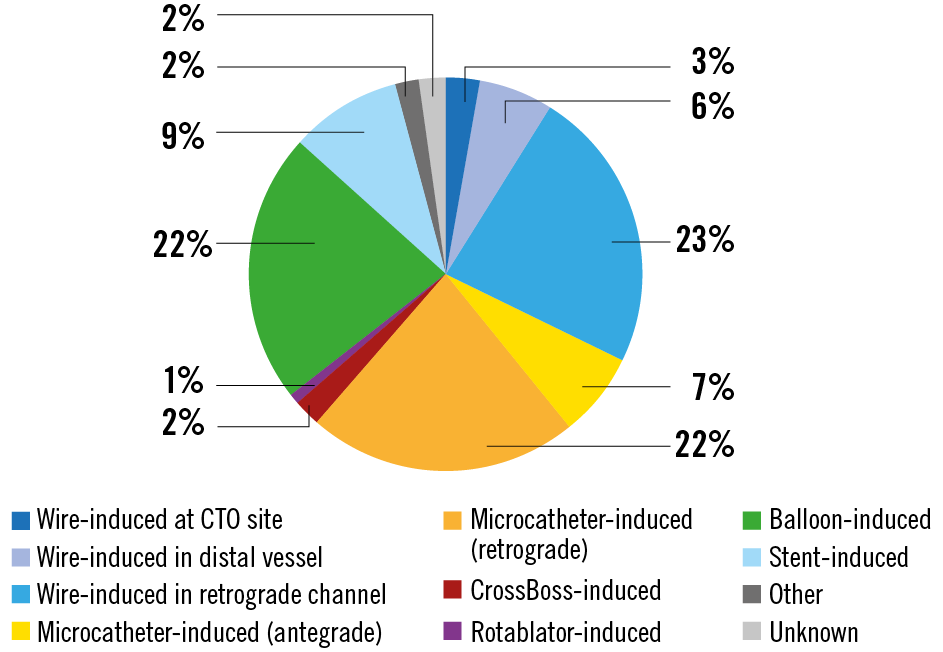
Figure 2. Mechanisms of perforation during CTO PCI.
Figure 3. Association between perforation severity and management strategies.
Thirty-day follow-up was conducted. The primary endpoint on follow-up was target vessel failure (TVF), which was defined as a composite of cardiac death, target vessel MI, and ischaemia-driven target lesion revascularisation11.
STATISTICAL ANALYSIS
Continuous variables are presented as mean±standard deviation and compared with the Student’s t-test. Categorical variables are presented as frequency (percentages) and compared with the chi-square test.
Variables associated with coronary perforation on univariate analysis with a p<0.05, as well as variables cited in the literature as predictors of coronary perforation5,6,7, were entered into a multivariate model to identify independent predictors of perforation. The final model included the following variables: centre, age, sex, prior coronary artery bypass graft (CABG) surgery, blunt stump, moderate-to-severe calcification, >45º bending, length >20 mm, rotational atherectomy, antegrade dissection/re-entry, and retrograde approach. The stepwise backward selection method (p-entry <0.05, p-exit >0.10) was used. The results of these analyses are presented as odds ratios (OR) with 95% confidence intervals.
For all tests, a p<0.05 was considered statistically significant. Statistical analyses were performed using SPSS, Version 24 (IBM Corp., Armonk, NY, USA).
Results
CLINICAL CHARACTERISTICS
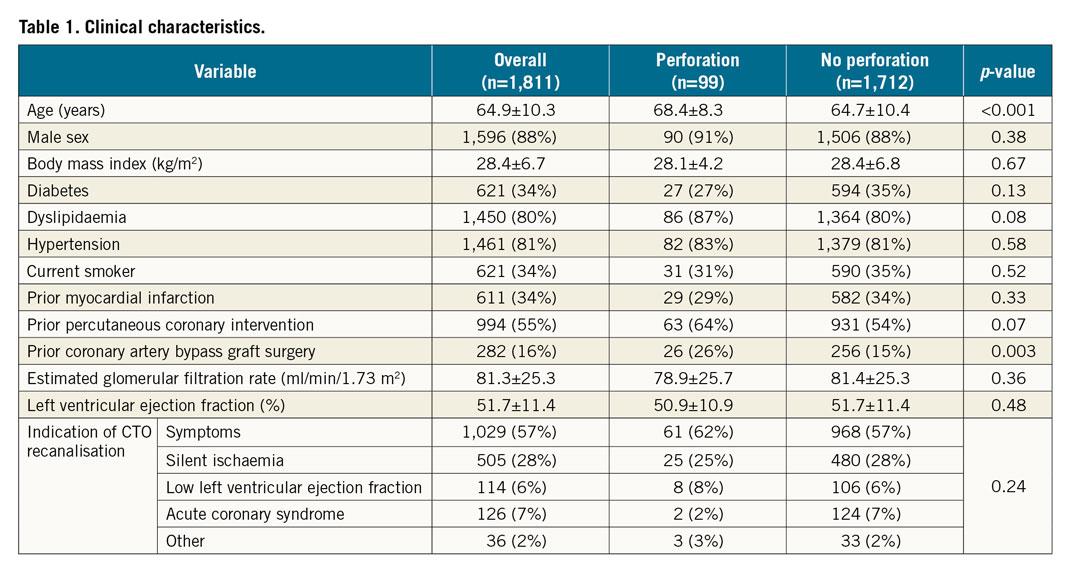
During the study period n=1,811 patients underwent CTO PCI. Of these, n=99 (5.5%) suffered a perforation and n=1,712 did not. Data on CTO PCI activity at each participating centre are provided in Supplementary Table 1. As shown in Table 1, patients in the perforation group were older (68.4±8.3 vs 64.7±10.4 years, p<0.001) and had higher prevalence of prior CABG (26% vs 15%, p=0.003). The prevalence of cardiovascular risk factors, other comorbidities, and indication for CTO revascularisation was similar between groups.
ANGIOGRAPHIC AND PROCEDURAL CHARACTERISTICS
Table 2 shows the angiographic data of the study cohort. There were no differences in the number of diseased vessels, or the target CTO vessel. The prevalence of blunt stump, moderate-to-severe calcification, >45º bending, and length >20 mm was higher in the perforation group. As a consequence, the mean J-CTO score was markedly higher in this group (2.7±1.2 vs 2.0±1.3, p<0.001). Difficult occlusions (J-CTO score ≥2) were very frequent in both groups, although more so in the perforation group (84% vs 62%, p<0.001).
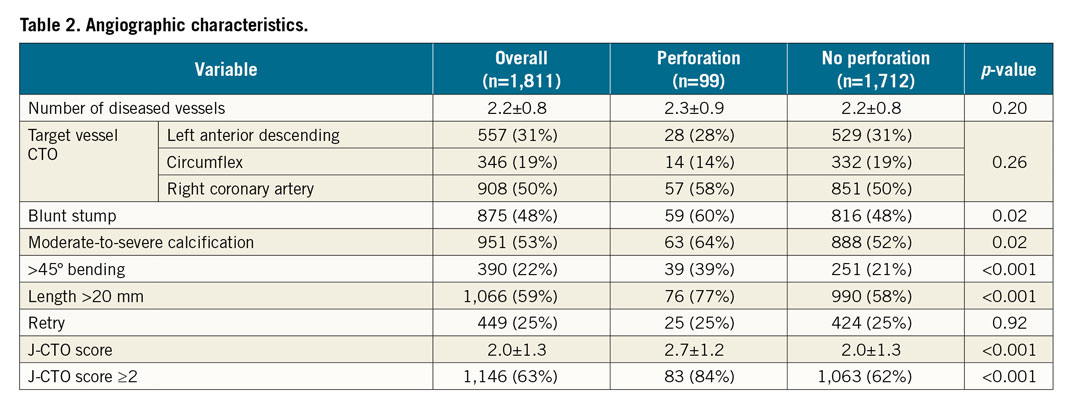
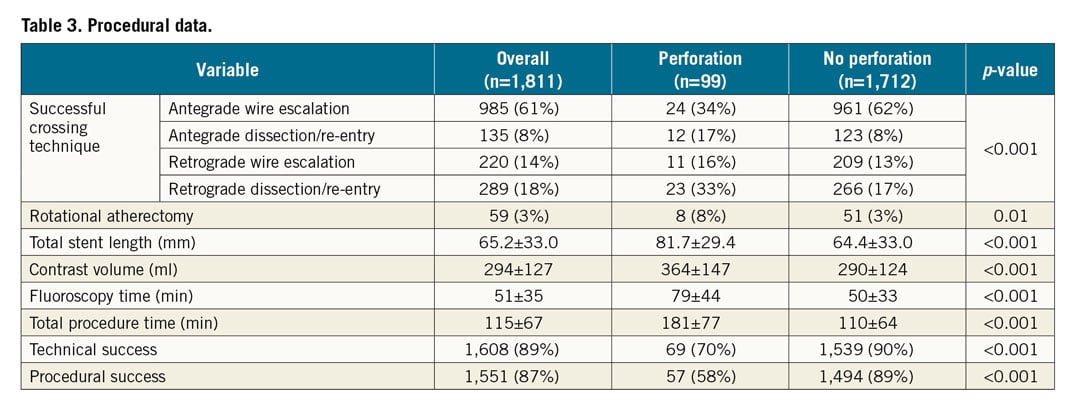
Table 3 shows the procedural characteristics of the study population. While antegrade wire escalation was by far the most frequent successful crossing technique in the no perforation group (62% vs 34%), the retrograde approach (49% vs 30%) and antegrade dissection/re-entry (17% vs 8%) were more frequent successful crossing techniques in cases with perforation (p<0.001). Rotational atherectomy was used more often in cases that developed a perforation (8% vs 3%, p=0.01). Total stent length was longer in cases with perforation. Procedural metrics (contrast volume, fluoroscopy time, and total procedural time) were worse in this group. Technical (70% vs 90%) and procedural (58% vs 89%) success rates were markedly lower in perforation cases (p<0.001 for both).
PERFORATIONS: SITES AND MECHANISMS
The frequency of Ellis type I, II, III and III “cavity spilling” perforations was 11%, 46%, 28%, and 14%, respectively. Figure 1 shows perforation data according to perforation site. In 48% of cases, perforation involved the CTO vessel, while the retrograde approach was responsible in 46% of cases. In two patients, there was a safety/support wire-induced perforation in a non-CTO vessel, while in another case the vessel distal to a right coronary artery CTO was perforated after a forceful pull of an entrapped rotational atherectomy burr (which had been advanced retrogradely through a saphenous vein graft in an attempt to allow retrograde wiring of the CTO). Notably, in two patients no perforation could be observed after a meticulous review of all case runs; however, these patients were still included in the perforation group as tamponade developed in both.
Figure 2 provides insight into the perforation mechanisms. In 32% of cases, perforation was caused by wire exit (either antegradely or retrogradely), while in 29% of cases it was caused by microcatheter advancement. Balloon- and stent-induced perforations were observed in 22% and 9% of cases, respectively. More uncommon mechanisms of perforation were related to dissection or rotational atherectomy devices.
PERFORATIONS: MANAGEMENT AND OUTCOMES
In 47/99 cases (47%), no intervention was performed. In 52/99 (53%) cases (which represented 2.9% of the overall study population), perforations required intervention. The most frequently applied management strategies included: covered stent implantation (25%), balloon occlusion (9%), and coil/fat embolisation (9%). Figure 3 presents data on the association between the degree of perforation and subsequent management. While observation was the most common management strategy for Ellis type I, II, and III cavity spilling perforations, covered stent implantation was the most used approach for Ellis type III perforation (59%). Covered stent implantation was performed with the ping-pong technique in 3/25 cases and with a single guiding catheter technique in the remainder. Covered stents implanted included: BeGraft (n=11) (Bentley Innomed GmbH, Hechingen, Germany), GRAFTMASTER® (n=8) (Abbott Vascular, Santa Clara, CA, USA), Aneugraft® (n=5) (Amnis Therapeutics Ltd., Or Akiva, Israel), and PK Papyrus (n=1) (Biotronik, Berlin, Germany). Other strategies included balloon occlusion, coil embolisation, surgery after covered stent implantation, conventional metallic stent implantation. Notably, in 15% of such cases, pericardiocentesis only was performed because bleeding stopped in the meantime. Heparin reversal with protamine was performed in 11/99 cases (always after removal of wires, balloons and other equipment from the coronary arteries).
While in 43 cases (83%) the intervention needed to manage the perforation was performed during the index CTO PCI, in nine (17%) no action was undertaken acutely but was carried out in a separate procedure a few hours later due to delayed-onset tamponade. Among these, one patient was treated with covered stent implantation, another with coil embolisation, and another with fat embolisation, whereas in the remaining six cases only pericardiocentesis was performed as no residual bleeding was observed. Tamponade was observed in 20/99 (20%) patients (which represented 1.1% of the whole study population).
Figure 4 presents data on the association between perforation site, perforation severity, tamponade, and in-hospital death. Ellis type III perforations were most frequently observed at the CTO site and were accountable for 16/20 tamponades and 3/5 deaths. Septal perforations were benign, regardless of their severity as assessed with the Ellis classification. Notably, the two patients for whom a perforation could not be identified after careful angiogram review suffered a high burden of complications: one developed tamponade after the procedure (which was successfully treated), but again no clear source of bleeding could be identified upon new coronary angiogram. Another patient developed right ventricular outflow tract haematoma soon after the procedure with tamponade physiology and died minutes after the procedure while undergoing a computed tomography scan. This was the only post-CABG subject who suffered tamponade and also the only post-CABG patient who died in the perforation group in our series.
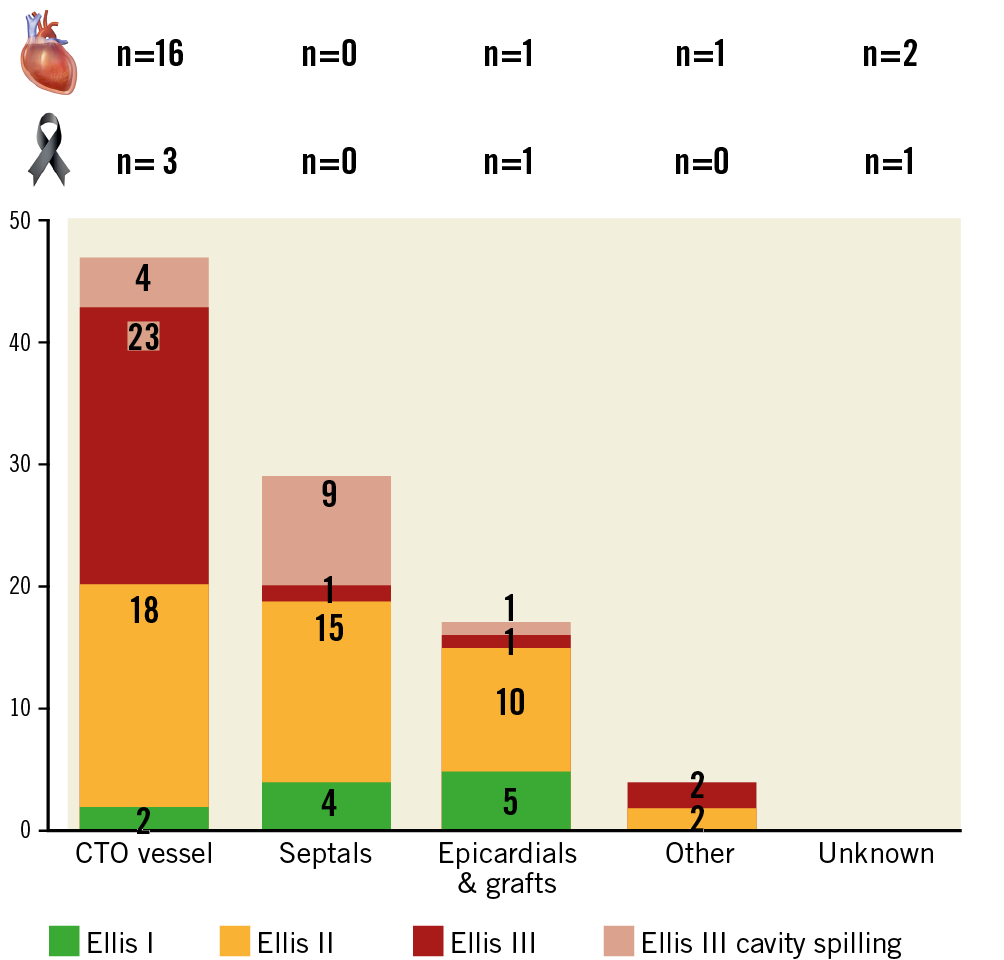
Figure 4. Association between perforation site, perforation severity, tamponade, and in-hospital death.
OTHER IN-HOSPITAL ADVERSE EVENTS
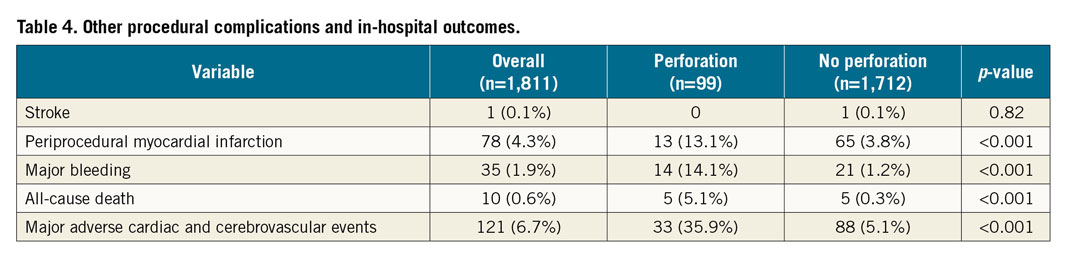
Table 4 presents data on other in-hospital adverse events. While stroke rates were similar between groups, periprocedural MI, major bleeding, and all-cause death were more frequent in the perforation group. In particular, the rate of mortality was markedly higher in patients who suffered a perforation (5.1% vs 0.3%, p<0.001). As a consequence, MACCE incidence was seven times higher in perforation cases (35.9% vs 5.1%, p<0.001).
INDEPENDENT PREDICTORS OF CORONARY ARTERY PERFORATION
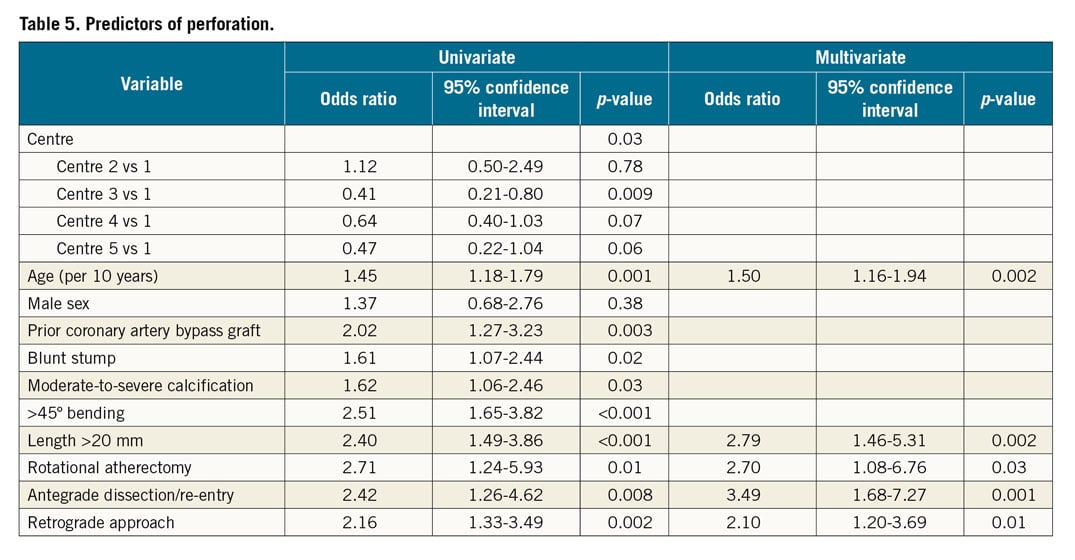
Table 5 presents the univariate and multivariate analysis for the prediction of perforation. Age (OR 1.50, p=0.002), occlusion length >20 mm (OR 2.79, p=0.002), use of rotational atherectomy (OR 2.70, p=0.03), antegrade dissection/re-entry (OR 3.49, p=0.001) and the retrograde approach (OR 2.10, p=0.01) were independently associated with the development of a perforation.
CLINICAL OUTCOMES ON SHORT-TERM FOLLOW-UP
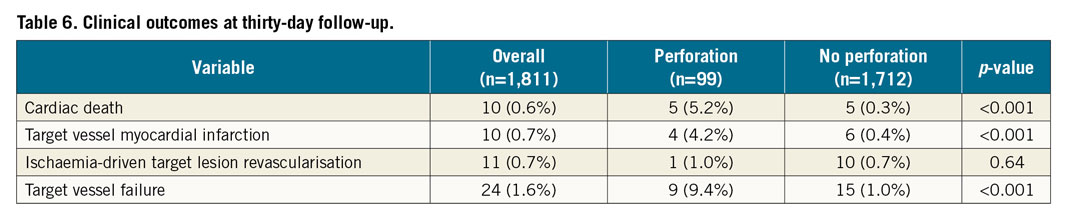
Table 6 shows the rates of clinical outcomes at thirty-day follow-up. The incidence of cardiac death (5.2% vs 0.3%, p<0.001) and target vessel MI (4.2% vs 0.4%, p<0.001) was higher in the perforation group. As a consequence, the TVF rate was markedly higher among patients who suffered a perforation (9.4% vs 1.0%, p<0.001).
Discussion
Our main study findings are: 1) coronary perforations are observed in 5.5% of CTO PCIs, require intervention in half of the cases, and lead to tamponade in one fifth of patients; 2) 5.1% of patients who suffer a perforation die during hospital stay; 3) approximately half of perforations are due to injury to the CTO vessel and the other half are related to the retrograde approach; 4) the highest burden of acute morbidity and mortality was observed in patients who developed CTO vessel-related perforations; 5) age, long occlusions, and advanced techniques (rotational atherectomy, antegrade dissection/re-entry and the retrograde approach) needed to tackle complex occlusions were independently associated with the development of perforation; 6) patients with perforation suffered an increased incidence of TVF on short-term follow-up.
Danek et al6 reported on the incidence, treatment, and outcomes of coronary perforation during CTO PCI in the large multicentre PROGRESS-CTO registry. They included 2,049 patients and observed coronary perforation in 85 patients (4.1%), an incidence comparable to our report (5.5%). Cases with perforation were angiographically more complex, similar to our study. The incidence of tamponade (0.9%) was similar to our series (1.1%). Older age, use of antegrade dissection re-entry and the retrograde approach were independently associated with perforation, confirming our findings. Moreover, similar to our study, Danek et al also found markedly lower technical and procedural success rates in patients who suffered perforation, suggesting that in many cases the operator facing such a complication aborts subsequent recanalisation attempts.
Wu et al7 recently reported on the predictors, treatment, and long-term outcomes of coronary perforation during retrograde CTO PCI via epicardial collaterals. In their small single-centre study (n=155), they observed a coronary perforation in 15.5% of cases, a high figure that reflects the hazard of using such fri-able and tortuous collateral channels. Tamponade was observed in 29%, which was effectively managed using coil embolisation and pericardiocentesis. At seven-year follow-up, 11% of patients suffered major adverse cardiac events, with no differences between patients who did versus those who did not suffer coronary perforation.
A very large study (n=26,807) by Kinnaird et al5 indicated that coronary perforation might have a “legacy effect” on mortality, with an odds ratio for 12-month all-cause mortality of 1.60 for perforation survivors compared with matched subjects without a perforation (p<0.0001). The authors related this intriguing finding to several possible explanations, such as incomplete revascularisation due to procedure interruption secondary to perforation12, concomitant complications (vascular complications, periprocedural MI, major bleeding, etc.), and restenosis/thrombosis of covered stents, among others.
As reported by Parsh et al4, CTO PCI is the strongest independent predictor of developing coronary artery perforation, being associated with a sevenfold increase in the adjusted risk of such a complication, compared to non-CTO PCI. The aetiology of coronary perforation in CTO PCI is multifaceted and can be related to the presence of severe calcification within the occlusion requiring aggressive plaque modification (e.g., atherectomy)13, proximal cap ambiguity and unclear vessel course6, and the use of antegrade dissection/re-entry techniques and the retrograde approach6,14, particularly through epicardial collaterals7,15. Additionally, perforation mechanisms common to non-CTO PCI can be observed as well. Therefore, coronary perforation can develop at any stage of CTO PCI (antegrade approach, retrograde approach, lesion preparation, stenting, post-dilatation). Importantly, it can involve virtually any segment of the coronary tree, as in many cases all three major vessels are instrumented (antegrade wiring, retrograde access, and supportive wire).
We have identified older age, long occlusions, and the need for rotational atherectomy, antegrade dissection/re-entry and the retrograde approach as independent predictors of coronary perforation. Most of these associations had already been reported in the literature6,14, thus conferring external validity to our findings. Specifically, older age and the need for rotational atherectomy are associated with coronary calcification, which increases the risk of perforation during lesion preparation, stenting and post-dilatation. In our series, only one case of perforation was directly caused by rotational atherectomy (forceful pull of an entrapped burr). In two other instances, perforation was observed during vessel predilatation following rotational atherectomy; however, there was no topographic coincidence between the site where rotational atherectomy had been performed and the location of the perforation. Therefore, such a technique has to be considered as a marker of calcification predisposing to perforation in these two cases. In the remaining five cases in which rotational atherectomy was performed, such a technique was not directly related to the development of perforation (e.g., the latter was observed during retrograde wiring of a collateral channel). The use of antegrade dissection/re-entry and the retrograde approach is more frequent in complex occlusions, with a higher risk for wire exit within the CTO body or a collateral channel, respectively. Finally, long occlusions are also associated with a higher likelihood of wire exit.
In our cohort, 53% of perforation cases required intervention, which was most frequently performed for Ellis type II/III perforations. Ellis type II/III perforations of the CTO vessel were the most common, often evolving to tamponade and subsequent death, despite the use of several management strategies (most commonly covered stent implantation). The incidence of life-threatening collateral channel perforation during the retrograde approach (Ellis type II/III of epicardial collaterals) was low (1/1,811, 0.06%), and possibly related to the extensive experience with the retrograde approach of the operators at the five participating centres.
Notably, in two cases, no clear cause of coronary perforation could be observed, despite meticulous angiogram review. Both patients suffered tamponade, and one of them died, as previously explained. Therefore, although very infrequent, the absence of a perforation image throughout CTO PCI is not an absolute guarantee of not suffering tamponade in the immediate post-procedural period. Besides these two cases, seven more patients suffered delayed-onset tamponade and required pericardiocentesis with/without intervention to seal the perforation. Globally, these observations suggest that coronary perforation during CTO PCI is a complex phenomenon, not always promptly and easily diagnosed, and it can subsequently have devastating consequences on patients undergoing such procedures.
Limitations
Our study has some limitations. First, it is an observational study, sharing all the limitations of this kind of design. Second, clinical follow-up was not available for all patients, although the proportion of subjects lost to follow-up was moderate (15%) and comparable to that of other CTO registries8. Finally, our observations derive from procedures performed by several operators with vast experience with the retrograde approach: therefore, the incidence of coronary perforation related to retrograde access use might be higher (and its consequences more severe) at less experienced centres.
Conclusions
In our large multicentre registry, coronary perforations were observed in a non-negligible proportion of CTO PCIs, often required intervention, and were associated with tamponade and mortality in a minority of patients. CTO vessel-related perforations were related to the highest burden of morbidity and mortality. Age, long occlusions, and the use of rotational atherectomy, antegrade dissection/re-entry and the retrograde approach were independently associated with the development of perforations. Patients with perforation suffered an increased incidence of TVF on short-term follow-up.
|
Impact on daily practice Coronary artery perforation was observed in 5.5% of CTO PCIs, required intervention in about half of the cases, and was associated with tamponade in 20% and mortality in 5.1%. CTO vessel-related perforations were related to the highest burden of morbidity and mortality. Age, long occlusions, and the use of rotational atherectomy, antegrade dissection/re-entry and the retrograde approach were independent predictors of developing coronary artery perforation during CTO PCI. Patients with perforation suffered an increased incidence of TVF on short-term follow-up. |
Conflict of interest statement
L. Azzalini has received honoraria from Abbott Vascular, Guerbet, Terumo, and Sahajanand Medical Technologies, and research support from ACIST Medical Systems, Guerbet, and Terumo. S. Ojeda has received honoraria from Terumo. M. Pan has received honoraria from Abbott Vascular and Terumo. K. Mashayekhi has received consulting/speaker/proctoring honoraria from Abbott Vascular, Asahi Intecc, AstraZeneca, Biotronik, Boston Scientific, Cardinal Health, Daiichi Sankyo, Guerbet, Medtronic, SIS Medical, Teleflex, and Terumo. The other authors have no conflicts of interests to declare.