Abstract
Aims: The aim of the present study was to compare the midterm clinical outcomes of patients undergoing successful chronic total occlusion (CTO) percutaneous coronary intervention (PCI) according to the crossing technique used, in a large multicentre registry.
Methods and results: We compiled a multicentre registry of consecutive patients undergoing successful CTO PCI. Patients were divided into three groups: true-to-true (TTT) approach, modern dissection/re-entry (DR) techniques (CrossBoss/Stingray, reverse CART), and old DR techniques (LAST, STAR, CART). Cox regression was used to identify independent predictors of major adverse cardiac events (MACE: cardiac death, myocardial infarction and target vessel revascularisation). We included 924 patients (TTT, n=571; modern DR, n=258; old DR, n=95). Patients in both DR groups had a higher prevalence of comorbidities, angiographic and procedural complexity. The 12-month MACE rate was higher in old DR (22.1%) than in modern DR (8.9%) and TTT (9.1%, p<0.001). Old (hazard ratio [HR] 2.02, 95% confidence interval [CI]: 1.12 to 3.61, p=0.02) but not modern (HR 0.98, 95% CI: 0.54 to 1.79, p=0.96) DR techniques were associated with a higher adjusted risk of MACE compared to TTT.
Conclusions: The use of old but not modern DR techniques was associated with a higher risk of MACE. Therefore, CrossBoss/Stingray and reverse CART might be considered as first-line strategies for antegrade and retrograde DR-based CTO PCI, respectively.
Abbreviations
CART: controlled antegrade and retrograde subintimal tracking
CTO: chronic total occlusion
DR: dissection/re-entry
LAST: limited antegrade subintimal tracking
MACE: major adverse cardiac events
MI: myocardial infarction
PCI: percutaneous coronary intervention
STAR: subintimal tracking and re-entry
TTT: true-to-true
TVR: target vessel revascularisation
Introduction
The introduction of dissection/re-entry (DR) techniques catalysed a remarkable improvement in success rates (>90%) and a wider adoption of chronic total occlusion (CTO) percutaneous coronary intervention (PCI)1. Indeed, both antegrade and retrograde DR techniques allow effective crossing of long, calcified and ambiguous occluded segments, thus facilitating the treatment of very complex CTO. DR techniques have, however, been associated with higher risk of periprocedural complications (including perforation and myocardial injury)2,3. Additionally, experience with the initial DR techniques (which are infrequently used at present) showed alarmingly high restenosis rates4,5.
Only a few recent studies have investigated the midterm outcomes of DR techniques, as compared with a conventional true-to-true (TTT) lumen strategy6-8. These reports suggested equipoise between the two approaches, but were limited by their small sample size and single-centre nature. The aim of the present study was to compare the midterm clinical outcomes of patients undergoing successful CTO PCI according to the crossing technique used, in a large multicentre registry.
Methods
PATIENT POPULATION
This multicentre registry included all consecutive patients who underwent successful CTO PCI in the dedicated programme of one of the four participating centres (San Raffaele Hospital, Milan, Italy; Quebec Heart and Lung Institute, Quebec City, QC, Canada; VA North Texas Healthcare System, Dallas, TX, USA; Reina Sofia Hospital, Cordoba, Spain) between January 2010 and May 2016. Analyses were performed according to the crossing strategy used (TTT approach vs. “modern” DR techniques vs. “old” DR techniques). Figure 1 shows the study workflow. Figure 2 outlines the techniques used for CTO recanalisation in our cohort and their relationship with procedural complexity. All procedures were indicated according to the presence of angina, ischaemia or both, and were performed electively (ad hoc PCI was discouraged)1. Baseline, procedural and hospitalisation data were recorded. Follow-up was performed by means of phone interview, review of hospital records or outpatient visit. The study was approved by the institutional review boards of the four participating hospitals, and study subjects gave written informed consent.
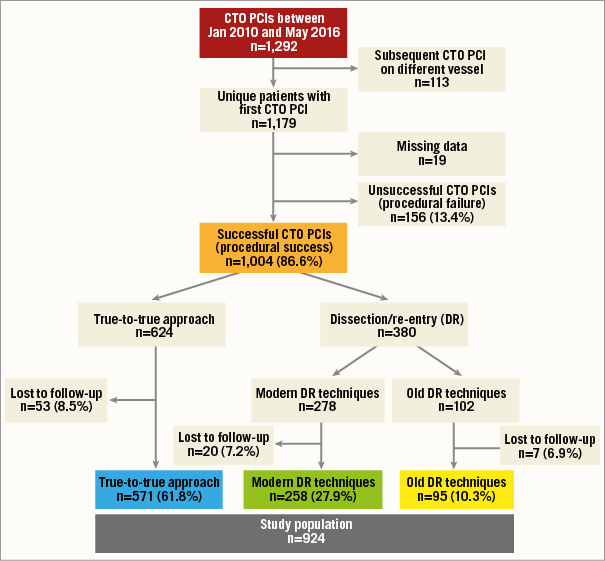
Figure 1. Study workflow. Procedural success was defined as a residual stenosis <30% with antegrade Thrombolysis In Myocardial Infarction (TIMI) 3 flow in the target vessel, in the absence of in-hospital adverse events (all-cause death, Q-wave myocardial infarction, stroke, recurrent angina requiring target vessel revascularisation, cardiac tamponade).
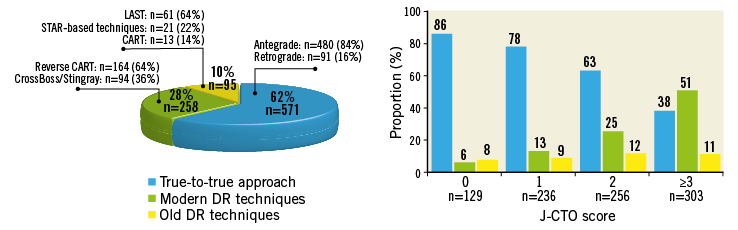
Figure 2. Techniques used in the study and their relationship to lesion complexity. A) Techniques used to recanalise chronic total occlusions (CTO) in this study. B) Relationship between CTO recanalisation techniques and lesion complexity (J-CTO score). CART: controlled antegrade and retrograde subintimal tracking; DR: dissection/re-entry; LAST: limited antegrade subintimal tracking; STAR: subintimal tracking and re-entry
DEFINITIONS
CTO was defined as a 100% stenosis with Thrombolysis In Myocardial Infarction (TIMI) 0 flow for >3 months9. The J-CTO score10 and the PROGRESS-CTO score11 were calculated for each lesion.
Old DR techniques included subintimal tracking and re-entry (STAR)-based techniques (including mini-STAR and contrast-guided STAR) and limited antegrade subintimal tracking (LAST) for the antegrade approach, and controlled antegrade and retrograde subintimal tracking (CART) for the retrograde approach.
Modern DR techniques included use of the Stingray™ system preceded or not by the CrossBoss™ catheter (both Boston Scientific, Marlborough, MA, USA) for antegrade DR, and reverse CART for retrograde DR.
TTT crossing was considered the most likely mechanism with the use of guidewire escalation (either antegrade or retrograde) or when the CrossBoss traversed the occlusion reaching the true lumen (i.e., without Stingray-facilitated re-entry).
Major adverse cardiac events (MACE) on follow-up were defined as the composite of cardiac death, target vessel myocardial infarction (MI: Q-wave and non-Q-wave) and ischaemia-driven target vessel revascularisation (TVR).
STATISTICAL ANALYSIS
Continuous variables are presented as mean±standard deviation and ANOVA was used for comparisons. Categorical variables are presented as frequency (percentages), and compared using the chi-square test.
Kaplan-Meier curves of MACE-free survival according to crossing strategy were plotted and compared using the log-rank test. Forest plots were used to ascertain the relationship between modern vs. old DR techniques and MACE, stratified by antegrade vs. retrograde approach. The results of this analysis are presented as unadjusted hazard ratios (HR) and 95% confidence intervals (CI).
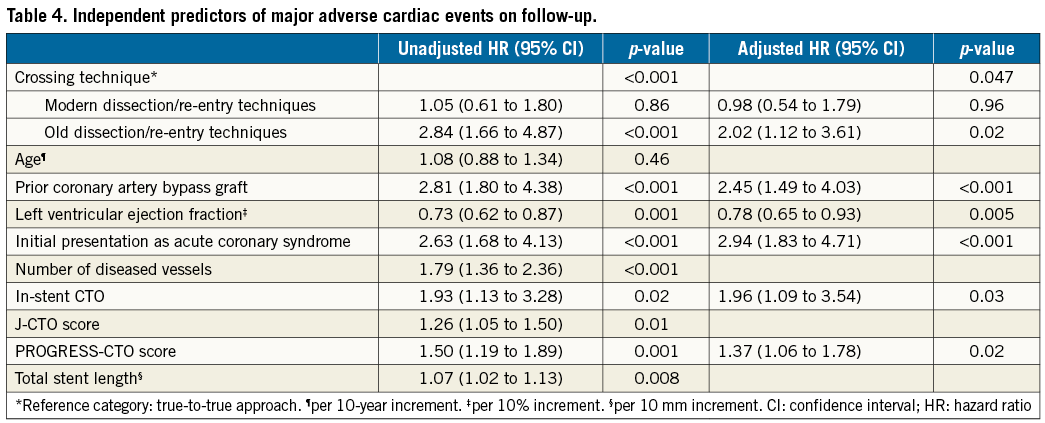
Finally, multivariable Cox regression analysis with a backwards-stepwise selection method (p-entry=0.05, p-exit=0.05) was used to ascertain whether the crossing strategy was associated with MACE during follow-up. Candidate variables were chosen among those that were unbalanced across crossing strategy groups (selected among those showing a p<0.20 in univariate analysis, as well as based on clinical judgement), using a ratio of 1:10 covariates-to-number-of-events, to avoid overfitting. The final model included crossing technique, age, prior coronary artery bypass graft (CABG), left ventricular ejection fraction (LVEF), initial presentation as acute coronary syndrome, number of diseased vessels, in-stent CTO, J-CTO score, PROGRESS-CTO score, and total stent length. The results of this analysis are presented as HR and 95% CI.
For all tests, a p<0.05 was considered significant. Statistical analysis was performed using SPSS, Version 24 (IBM Corp., Armonk, NY, USA).
Results
CLINICAL CHARACTERISTICS
Table 1 shows the clinical characteristics of the study population. Although demographics, as well as left ventricular and renal function and the prevalence of diabetes, did not differ across groups, patients in the two DR groups had a higher incidence of prior MI, PCI and CABG. Patients treated with modern DR techniques had a higher prevalence of dyslipidaemia and presented more often with angina symptoms, as compared with the other two groups.
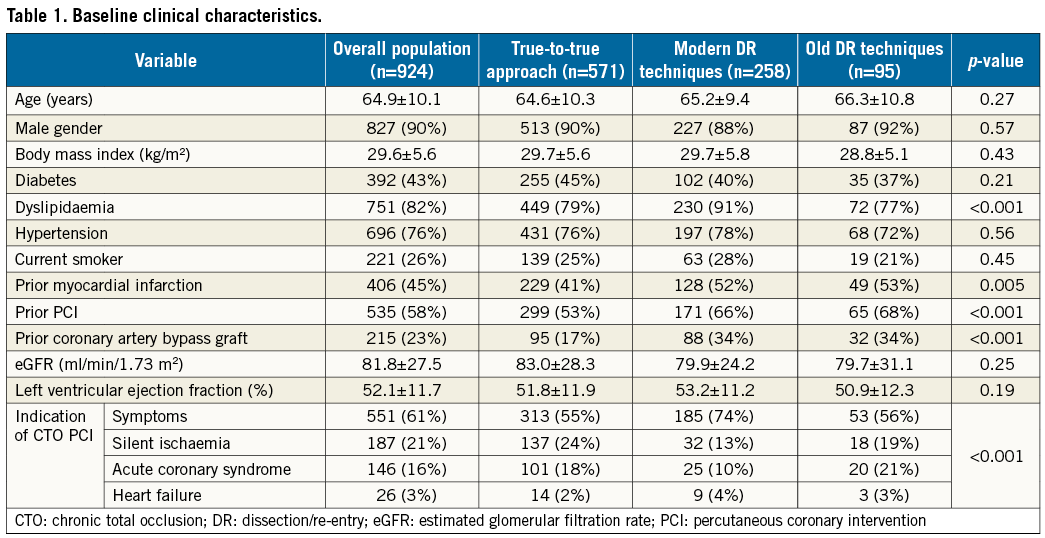
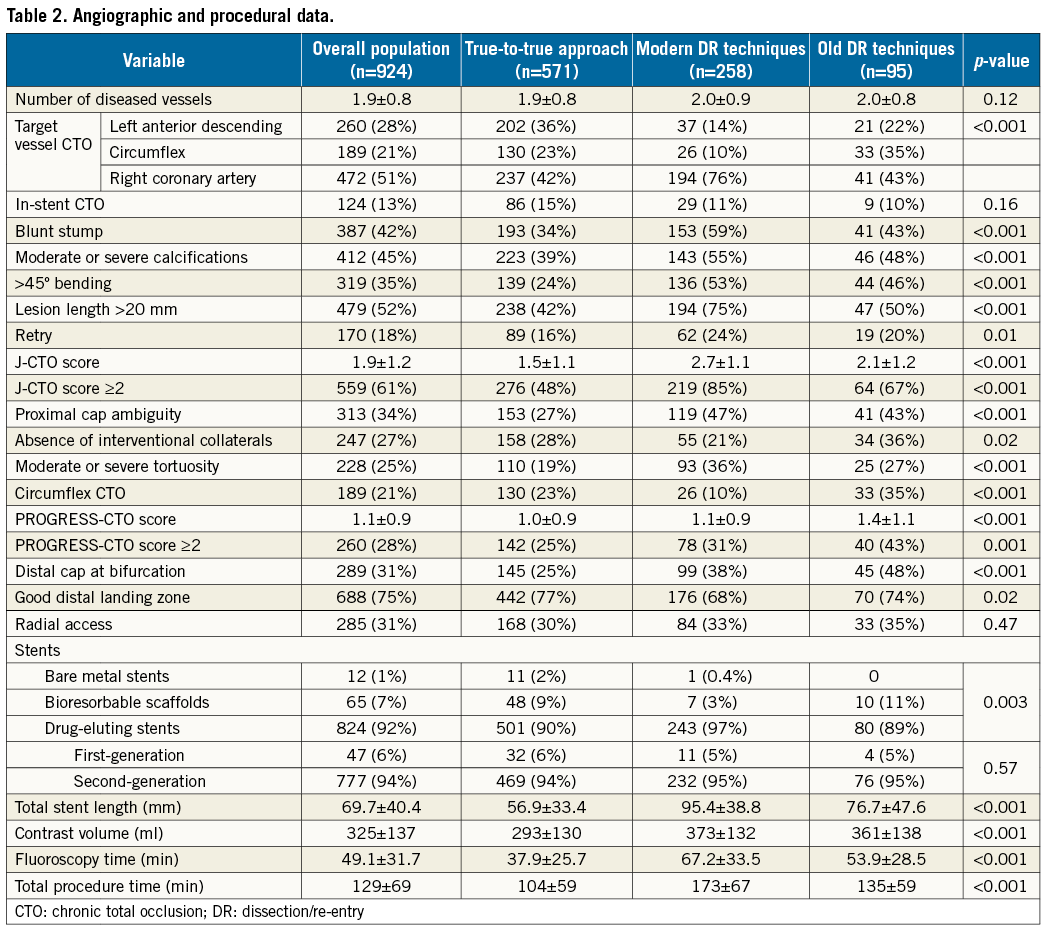
ANGIOGRAPHIC AND PROCEDURAL CHARACTERISTICS
Angiographic and procedural data are presented in Table 2. Although the right coronary artery (RCA) was the CTO target vessel most frequently treated in all groups (42%-76%), TTT patients were treated more frequently on the left anterior descending (LAD, 36%) than the two DR groups (modern DR 14%, old DR 22%; p<0.001). Occlusion complexity was higher in the two DR groups, as compared with TTT patients and as assessed with both the J-CTO score (TTT 1.5±1.1 vs. modern DR techniques 2.7±1.1 vs. old DR techniques 2.1±1.2, p<0.001) (Figure 2B) and PROGRESS-CTO score (1.0±0.9 vs. 1.1±0.9 vs. 1.4±1.1, respectively; p<0.001). Similarly, the presence of a bifurcation at the distal cap was higher and that of a good distal landing zone lower in the two DR groups, suggesting higher procedural complexity, as compared with patients undergoing a TTT-based PCI. Although drug-eluting stents (DES) were used in the majority of patients in all groups, DES use was highest in the modern DR group (97%, p=0.003). Among DES-treated subjects, there were no differences in the use of first- vs. second-generation devices. Total stent length was higher in the modern (95.4±38.8 mm) and old (76.7±47.6 mm) DR groups, as compared with TTT patients (56.9±33.4 mm, p<0.001). Similarly, procedural metrics indicated greater use of contrast, and longer fluoroscopy time and total procedural time in the two DR groups. Finally, no clear temporal trend was observed during the study period with regard to the specific crossing technique used (data not shown).
CLINICAL OUTCOMES ON FOLLOW-UP
Median follow-up was 414 (interquartile range: 287-746) days. Table 3 shows clinical outcomes at 12-month follow-up. While TTT and modern DR patients showed similar rates of adverse events, patients in whom old DR techniques were utilised had a markedly higher rate of TVR (old DR 18.1% vs. TTT 6.0% vs. modern DR 7.0%, p<0.001), driving a higher overall MACE rate (22.1% vs. 9.1% vs. 8.9%, respectively, p<0.001). In particular, pairwise comparisons indicated that old DR techniques were associated with higher incidence of TVR and MACE, and a trend towards higher incidence of MI, as compared with both modern DR techniques and a TTT approach separately. Kaplan-Meier curves showed a higher incidence of MACE throughout follow-up in old DR patients, as compared with the other two groups (p<0.001) (Figure 3).
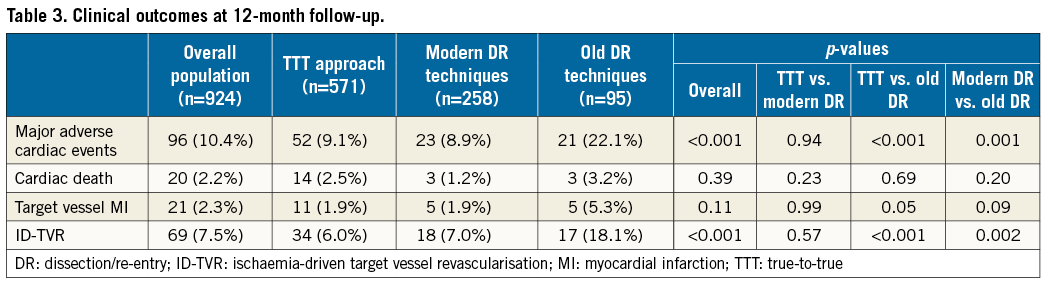
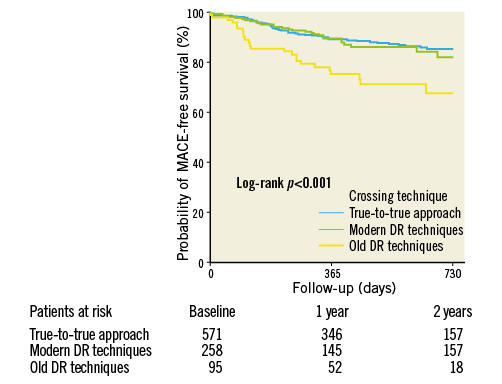
Figure 3. Kaplan-Meier curves of two-year survival free from major adverse cardiac events (MACE) according to crossing strategy.
As compared with old DR techniques, modern DR techniques were associated with lower unadjusted HR for MACE, regardless of the approach (antegrade, retrograde, combined antegrade and retrograde) (Figure 4). Adjusted Cox survival analysis (Table 4) indicated that old DR techniques (HR 2.02, 95% CI: 1.12 to 3.61; p=0.02), but not modern DR techniques (HR 0.98, 95% CI: 0.54 to 1.79; p=0.96), were associated with higher risk of MACE, as compared with a TTT approach. Other independent predictors of MACE were prior CABG, a lower LVEF, initial presentation as acute coronary syndrome, in-stent CTO, and a higher PROGRESS-CTO score.
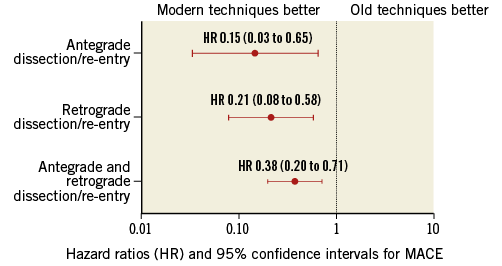
Figure 4. Forest plot of unadjusted hazard ratios and 95% confidence intervals of modern versus old dissection/re-entry techniques, stratified by approach (antegrade, retrograde, and both).
Discussion
We have found that modern DR techniques (Stingray system preceded or not by CrossBoss for antegrade DR, and reverse CART for retrograde DR) and a TTT approach are associated with similar rates of MACE on follow-up, following CTO PCI. However, old DR techniques showed a twofold increase in the adjusted risk of MACE, as compared with a TTT approach.
Historically, certain DR approaches have been linked to high risk of restenosis and are now rarely used in clinical practice. For example, STAR was used with higher success rates for the recanalisation of occlusions associated with low likelihood of success using a conventional TTT approach (especially long and tortuous occlusions). However, both the original STAR technique4 and its successive iterations (e.g., contrast-guided STAR5 and mini-STAR12) showed restenosis rates of 25-54% at two-year follow-up. This is probably related to poor distal run-off due to loss of side branches, secondary to extensive dissections. Indeed, recent studies have confirmed the importance of achieving final TIMI 3 flow following STAR12,13, an outcome that is not always predictable. Few data (mostly procedural description and acute results) support the use of other old DR techniques (e.g., LAST14 and CART15), and literature on midterm outcomes is scarce. Our data suggest that, despite the achievement of a normal final flow, the use of older DR techniques still remains associated with worse midterm outcomes compared to a TTT approach and newer DR techniques.
The introduction of a device-based approach to antegrade DR (CrossBoss/Stingray system) has allowed minimisation of vessel trauma during dissection, as well as geographically precise and predictable successful re-entry8. Mogabgab et al reported on the midterm outcomes in a single-centre study of 170 consecutive patients treated with either antegrade DR using the CrossBoss/Stingray system (n=60) or other strategies (n=110). During a mean follow-up of 1.81 years, there was no difference in MACE rates between the two groups (40.3% vs. 35.2%; p=0.42)8. Similarly, the adoption of reverse CART has allowed easier, more effective and possibly safer retrograde recanalisation of anatomically complex occlusions, as compared with CART16, but no long-term data are available on the specific outcomes of this technique (since pooled data for the retrograde approach are usually provided). Additionally, even state-of-the-art DR-based approaches are (albeit rarely) associated with unique challenges (e.g., need of creating a neo-ostium after RCA CTO recanalisation with reverse CART) and complications (e.g., stent luxation following subadventitial stenting)17. Therefore, a methodologically sound appraisal of the outcomes of DR techniques as compared with a TTT approach is warranted.
Only two studies have compared the midterm outcomes of DR-based recanalisation versus a TTT approach. Rinfret et al6 followed 187 consecutive patients undergoing successful CTO PCI at their institution (TTT approach 56%, DR techniques 44%). At a median follow-up of 398 days, there were no differences in the unadjusted rates of MACE (defined as in the present study) between DR techniques and a TTT approach (15.1% vs. 7.3%; p=0.17). Multivariable analysis confirmed that DR techniques had no significant impact on outcomes. Similarly, Amsavelu et al7 recently published their single-centre experience with such techniques in 173 consecutive patients undergoing successful CTO PCI (TTT approach 52%, DR techniques 48%). The 12-month incidence of death, MI, and the composite of acute coronary syndrome/target lesion revascularisation/TVR was 2.5%, 4.9%, and 24.4%, respectively, and was similar regardless of the crossing strategy used. Again, multivariable analysis indicated that DR techniques were not associated with target lesion revascularisation or the composite of death, MI, and any unplanned revascularisation on follow-up.
In comparison with these two reports, our study has several strengths. First, it is a multicentre registry with several high-volume operators involved, which confers external validity to our results. Second, our sample size is fivefold larger, which allowed us to perform a robust multivariable adjustment. Additionally, our follow-up was longer than in the aforementioned reports. Finally, our study separately analysed the outcomes of modern vs. old DR techniques, which represents a specific and novel aspect of the present report.
Our data indicate that old DR techniques should not be used in the recanalisation of chronically occluded coronary arteries. In the hands of experienced operators, modern DR techniques allowed successful recanalisation of very complex lesions and exhibited similar midterm outcomes as compared with a TTT approach, despite an almost twofold higher J-CTO score. However, such techniques were associated with markedly worse procedural metrics in our study (and also with a higher incidence of procedural MI according to other reports18). Therefore, modern DR techniques must be utilised only when anatomical considerations make the likelihood of success with a TTT strategy low and if the operator is familiar with such an approach.
We have also identified prior CABG, a lower LVEF, initial presentation as acute coronary syndrome, in-stent CTO, and higher PROGRESS-CTO score as independent predictors of MACE. Most of these associations had already been reported by others5,6,19,20. However, our observation that an angiographic variable such as the PROGRESS-CTO score predicts clinical outcomes in patients undergoing CTO recanalisation (analogously to the SYNTAX score in all-comers21) is novel and warrants further research. The PROGRESS-CTO score takes into account four features that have been associated with failed recanalisation attempts - proximal cap ambiguity, absence of interventional collaterals, moderate/severe tortuosity, and circumflex CTO11. It is possible that some of these variables identify a phenotype of more aggressive atherosclerosis, and might therefore be associated with a higher risk of adverse events on follow-up.
Limitations
Our study has several limitations. First, it is an observational study, and is thus susceptible to the effect of unidentified confounders. However, no randomised data are available on this topic. Second, the relatively small number of cases treated with each DR technique made more detailed analyses impossible to perform (e.g., direct comparisons between a specific technique and another). Third, we included only patients who underwent successful CTO PCI in an effort to maintain comparability with previous reports6,7 and since our study aim was to ascertain midterm (rather than procedural) outcomes of the different crossing techniques in our patient population. Fourth, all study patients underwent successful CTO PCI as per operator criterion. A blinded core laboratory analysis could have identified some patients as having TIMI 2 flow rather than 3. The identification of such a finding may have helped to understand the worse outcomes with old DR techniques, as final TIMI 3 flow is paramount to decreasing long-term TVR with such techniques12,13. However, such misclassification is probably random across all three groups, and in our view does not invalidate our findings. Finally, although this is a multicentre registry with several operators involved, our study findings might not be extrapolated to other institutions that do not have interventionalists experienced with the hybrid algorithm and various DR techniques.
Conclusions
In this multicentre registry of CTO PCI performed by operators experienced in a wide array of recanalisation techniques, the use of old DR techniques was associated with a higher adjusted risk of MACE as compared with a TTT approach. Therefore, such techniques should only be used as a last resort for the recanalisation of chronically occluded coronary arteries. On the other hand, modern DR techniques (Stingray preceded or not by CrossBoss for antegrade DR, and reverse CART for retrograde DR) and a TTT approach were associated with similar outcomes. Future techniques and devices for DR-based CTO recanalisation will be compared against the benchmark represented by CrossBoss/Stingray and reverse CART, for the antegrade and retrograde approach, respectively.
| Impact on daily practice The use of old dissection/re-entry (DR) techniques was associated with a twofold higher adjusted risk of major adverse cardiac events, while modern DR techniques (Stingray preceded or not by CrossBoss and reverse CART) showed similar outcomes as compared with a true-to-true approach. Our data suggest that the CrossBoss/Stingray system and reverse CART might be considered as first-line strategies for antegrade and retrograde DR-based CTO recanalisation, respectively. |
Conflict of interest statement
E. Brilakis has received consulting/speaker honoraria from Abbott Vascular, Asahi, Cardinal Health, Elsevier, GE Healthcare, and St. Jude Medical, research support from Infraredx and Boston Scientific, and his spouse is an employee of Medtronic. S. Rinfret has received consulting fees from Boston Scientific. The other authors have no conflicts of interest to declare.