The controlled antegrade and retrograde subintimal tracking (CART) technique - this is indeed the story of legends1. It was the beginning of a revolution – retrograde techniques – which addressed an unmet need in interventional cardiology that is still evolving. Their impact on outcomes has been tremendous. For the first time we have reached a 90% plus success rate, closing the gap between CTO and non-occlusive coronary artery disease. This was the boost necessary to move forward after decades of stagnation with a belief that was kept alive in the soul and mind of only a few. The journey for those involved from the beginning has been wonderful. Thirteen years of innovation when techniques and technology evolved together in a “chicken and egg” fashion finally leading to an explosion of both – from sporadic publications to a powerful waterfall of new data. An evidence-based medicine build-up that was inevitable and required, necessitating consistency in the definitions of both techniques and outcomes. Without these, the confusion of the long past “parallel wire”, “seesaw”, “telescopic”, and “side branch” techniques would look like a joke compared to what can be heard in contemporary dedicated CTO meetings – “IVUS-guided, confluent balloon, guiding catheter extension facilitated reverse CART with the ping-pong and rendezvous externalisation technique”!!
The subintimal tracking and re-entry (STAR) technique2 preceded the CART technique and its evolution, the reverse CART3; however, they both address the same concept which is using – or, to be more accurate, dissecting – the subintimal space. Both of them require re-entry to reach the distal or proximal true lumen. The evolution of both was also similar. STAR evolved to mini-STAR4 (smaller knuckle with soft wires, both for occlusive tissue tracking and re-entry) and the limited antegrade subintimal tracking (LAST) technique (very stiff wires for re-entry after soft knuckle wire dissection of the occluded segment). The proposed classification by Matsuno et al5 of the reverse CART technique as “conventional”, “directed” and “extended” follows the same concept as STAR: how much you respect the proximal or the distal preserved true lumen and how much you traumatise the occluded segment (big or small knuckle for the STAR or big or small balloon for the reverse CART).
The main concern in our attempt at clarity and simplicity in terms of definitions should not be the sub-categorisation of CART but whether this term is still contemporary based on the evolution of the techniques and technologies.
The answer, in my view, is definitely not.
The proposed terminology aims “to facilitate the communication, teaching and adoption” of the techniques, but also to determine its clinical relevance that still has to be prospectively validated. The evolution in the proposed techniques was possible due to an accompanying evolution in technology with the introduction of guidewires with high torque control. My prediction is that a further evolution in technology will push our techniques even more before we can clinically evaluate the proposed classification. The best example is the already widely used guiding catheter extension reverse CART that is not included in this classification, not to mention the PlasmaWire™ (RetroVascular, Pleasanton, CA, USA) which has reached initial human evaluation6 and other emerging technologies.
Any attempt at “quantification” of subintimal space injury in everyday life is an exercise in futility and carries with it the risk of arbitrary interpretation based on angiographic review, or even more operator “misinterpretation” of the procedure that was just performed. IVUS imaging has indicated a higher involvement of subintimal wire position compared to that evaluated by angiography7. We have learned that dissection-re-entry techniques are not always subintimal and that all the wire escalation ones are not always intimal, contrary to the currently existing perception. IVUS, at least in Europe, is, for various reasons, not routinely used and not recommended as such8. While IVUS can clarify the longitudinal length of the subintimal involvement, how can we quantify the barotrauma caused by small or big/bigger balloons as in the proposed reverse CART classification? How can we relate that to the clinical outcomes? There are so many confounders that any meaningful interpretation related to clinical outcomes would be very difficult.
After all these years we have come to realise that antegrade and retrograde are not CTO body crossing techniques but the way to reach the proximal or distal cap. They are not competitive but complementary techniques and there is no consensus as to their implementation during a CTO procedure. Algorithms9,10 try to provide guidance, but the mere fact that more than one exists demonstrates the disagreement of opinion, even among experts. There is not even agreement as to when a procedure should be declared as retrograde, with some proposing it should be when the wire touches the collateral channels, others when it reaches the distal cap and others, again, when both wire and microcatheter are successfully advanced through the collateral channels.
Where do we stand today?
“... Since their definition that a procedure was indeed an AWE, ADR or retrograde procedure is ambiguous (e.g., a procedure starts AWE, then switches to retrograde or ADR, fails to cross the CTO, then switches back to AWE which is successful: is this really a retrograde or ADR procedure?) ...”.
This was the commentary recently received by one of the reviewers on a submitted manuscript. An explanation of the abbreviations was not even considered. This is what an author has to address if he wants to publish his research and it is indicative of the confusion in the field. “WE” is the abbreviation for wire escalation, and “DR” stands for dissection re-entry. These are the main CTO body crossing techniques. “A” is the abbreviation for antegrade and “R” the abbreviation for retrograde, the routes to the target or “base of operations” as the Americans are now proposing9. The combination is easy - AWE, RWE, ADR, RDR. These four abbreviations are more or less where we stand today for wire-based techniques and they have been very nicely illustrated in Figure 1. They are widely used but have never been published as a global consensus of experts.
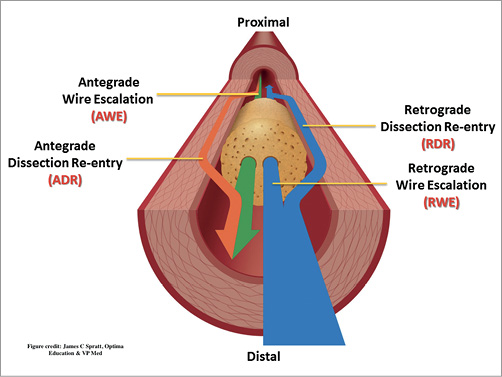
Figure 1. CTO crossing wire-based terminology.
CTO PCI has exceeded its purpose. It has managed to escape its hard shell as an isolated anatomical entity with few believers. The tips and tricks, the techniques developed and, above all, the devices invented, have moved on to a broader audience of interventional cardiologists who are not necessarily CTO operators. These are the complex anatomy operators and those dealing with the top end of the complex high-risk procedures (the CHIP concept). More and more operators are embarking in this field where the contribution of the lessons learned working with CTOs has made these procedures much more efficient and safe, providing patients with percutaneous treatment options not available in the recent past.
Conflict of interest statement
The author has no conflicts of interest to declare.