This issue of EuroIntervention concentrates on percutaneous coronary intervention (PCI) for coronary chronic total occlusions (CTO). This is a welcome development and reflects increasing interest in this topic.
The manuscript of Watanabe highlights the adverse prognostic implications of a bystander CTO as a non-culprit lesion in ST-elevation myocardial infarction (STEMI)1. These data support the hypothesis of potential for survival benefit for complete revascularisation for STEMI patients.
Developments within CTO PCI have led to success rates exceeding 90% per lesion in expert hands, without anatomical exclusions to case selection2. The manuscript of Dautov adds to data on the procedural approach to CTO PCI, confirming the safety and utility of “septal surfing” to assist crossing collateral channels3. Retrograde approaches represent an important component of CTO PCI and will often facilitate successful revascularisation where other strategies have failed2,4.
A consistent message from the literature is that the need for subintimal tracking increases with the anatomical complexity of the CTO lesion. This facilitates a high rate of procedural success without case selection2,4. It is within this context that the data of Hasegawa et al, examining the potential impacts of varying strategies used for CTO PCI5, should be interpreted. The retrospective identification of subintimal tracking is associated with a subset that required substantially more procedural (almost three hours on average per case) and fluoroscopy time (almost 90 minutes per case). Whilst case complexity is suboptimally described, it appears probable that subintimal tracking was a reflection of more challenging lesions. Subsequently, the authors have demonstrated a higher rate of repeat revascularisation in this small cohort of patients where a subintimal approach occurred (n=53)5. Whether this was planned or not is unclear from the presented data.
Historically, dissection-based approaches were associated with poor outcomes with “subintimal tracking and re-entry” (STAR) procedures. However, contemporary CTO PCI with retrograde dissection and re-entry (RDR) should limit dissection to within the confines of the CTO lesion. Similarly, controlled antegrade dissection and re-entry (ADR) limits any dissection plane from within the CTO segment to just beyond the distal cap. With STAR, re-entry was uncontrolled, unpredictable and run-off was frequently poor, leading to a high likelihood of re-occlusion of the target vessel. The key difference between current procedures and historical STAR is that run-off after successful hybrid CTO PCI is good and, crucially, to all distal branches.
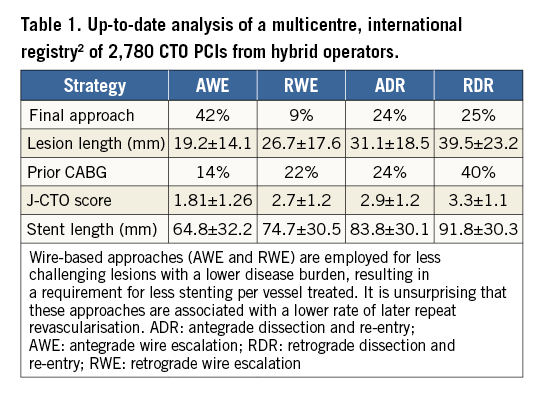
Experience from a larger cohort of contemporary hybrid CTO cases (n=805, 47% revascularised by dissection and re-entry) demonstrates that lesion complexity, length of occlusion and disease burden are markers of a subintimal approach for CTO PCI (Table 1)6. This is consequent on the lack of efficacy of standard techniques of wire escalation in very complex disease2,6. As a result, disease burden is a key driver and confounder towards adverse events at one year, with more target vessel revascularisation required in RDR approaches. RDR cases had the heaviest burden of disease and thus stent lengths (71% of RDR cases required >75 mm of stent)6. Irrespective of this, the rate of major adverse cardiovascular events (MACE) for the population was low at 12 months (8.6%), and 88% of patients had durable symptom relief with no or minimal angina despite the approach to revascularisation6.
One key and often unspoken question for those with a coronary CTO is what lesion or which patient will not be offered a PCI. Previous data have shown that, of all patients with a CTO at angiography, only 10% had an attempt at CTO PCI, with only 7% revascularised7. Therefore, bias in case selection is inherent. Many operators can reflect on sending 10 or more patients’ angiograms ahead of a forthcoming visit from a CTO PCI expert, but having only two or three of these patients accepted for treatment. Similarly, this practice does not offer a solution to the majority of people who suffer from a substantial burden of symptoms caused by the CTO lesion.
Hybrid CTO operators select cases based on clinical indications and not anatomical features. Once cases have been chosen on clinical need, the hybrid CTO approach is an algorithm-based strategy (Figure 1), where the CTO anatomy determines the choice of approach that aims to achieve the safest (and most efficient) successful outcome8. Efficiency in CTO PCI emphasises that radiation and contrast doses should be minimised. Whilst some operators question the adoption of an up-front dissection-based strategy to treat CTO lesions, the hybrid algorithm encourages the early and limited use of more complex approaches, where needed, to open the artery. Thus, all patients can potentially be treated successfully, including those with very challenging anatomy (Table 1).
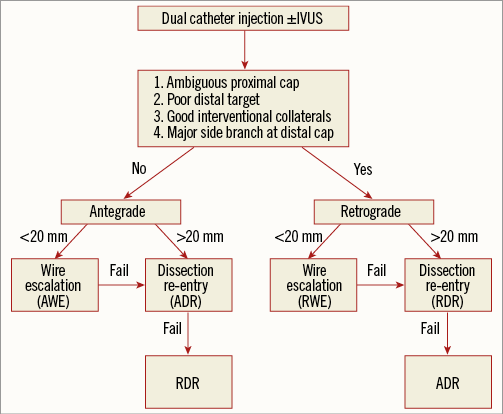
Figure 1. The hybrid algorithm, where anatomical features based on four key questions guide the operator towards the initial strategy for CTO PCI. Early switches in strategy are then encouraged if the case stalls or enters a failure mode.
Many lesions can be approached with two (or three or even four) initial strategies4, with the first strategy employed often dictated by operator experience and/or available technology. Nevertheless, it is clear that pursuing wire-based approaches for long and complex occlusions is frequently futile4, wasting radiation, contrast and catheter laboratory time whilst risking unnecessary complications. A “hybrid CTO PCI” thought process offers the potential for a successful procedure with much lower use of lab time and less radiation exposure. It recognises that the prospective use of controlled dissection strategies in complex disease (thus preventing case selection based on a lack of perceived feasibility) improves case efficiency and success.
When interpreting data that compare approaches and outcomes for patients treated by CTO PCI, it is imperative that operators understand that they are often being presented with information that describes outcomes for “apples and oranges”. With the understanding that treatment of patients should be based on clinical parameters (supplemented with functional and physiological data), irrespective of complexity, it is clear that more complex strategies are often required. It is reassuring to note, therefore, that durable outcomes can be obtained with low in-hospital and long-term complication rates2,4,6 and an efficient use of catheter laboratory time and radiation. A structured and algorithm-based approach now affords successful CTO PCI for the vast majority of patients.
Education and training9 can help the operator arrive at a good procedural outcome for the patient and both should be encouraged. The “hybrid approach”8 to CTO lesions has been proven effective in thousands of CTO procedures across multiple geographies2,4,10,11. In the absence of a validated alternative, we suggest that this is the best current in-case guide for procedural approaches in CTO PCI if all patients are to be offered treatment.
Conflict of interest statement
S. Walsh and C. Hanratty are consultants to Abbott Vascular, Boston Scientific, Medtronic and Vascular Solutions. J.C. Spratt is a consultant to Abbott Vascular, ASAHI Intecc, Boston Scientific and Vascular Solutions.