Chronic total occlusions (CTO) continue to be one of the most challenging coronary lesion subsets to recanalise. However, CTO percutaneous coronary intervention (PCI) has evolved substantially during recent years, with improvements in equipment, techniques, and available data, as eloquently summarised in the 2019 EuroCTO Club consensus statement1.
The present
CTO PCI should be performed when the anticipated benefits (such as improvement of symptoms and myocardial function, reduction in the risk for arrhythmias, and better tolerance of subsequent acute coronary syndromes) exceed the potential risks (periprocedural and long-term complications) and when the likelihood of success is high (which in turn depends on operator experience and angiographic lesion complexity)1,2,3.
Although there are local differences in preferred techniques, there has been remarkable convergence on how CTO PCI should be performed from operators all around the globe, recently distilled in seven key principles:
1. Ischaemic symptom improvement is the primary indication for CTO PCI.
2. Dual coronary angiography and in-depth and structured review of the angiogram are key for planning and safely performing CTO PCI.
3. A microcatheter should be used for guidewire support.
4. All CTO crossing strategies (antegrade and retrograde) are complementary and important.
5. Changing of crossing strategy facilitates success.
6. CTO PCI is best performed by experienced operators and centres.
7. Stent deployment should be optimised.
Minor differences still exist, for example on the role of parallel wiring vs. dissection/re-entry in case of subintimal guidewire entry, or the use of intravascular ultrasound and computed tomography for clarifying proximal cap ambiguity. Moreover, the EuroCTO document outlines some specialised “tips and tricks”, such as the “parallel sheath” technique for overcoming iliac tortuosity. All three CTO PCI documents published to date (EuroCTO1, Asia Pacific algorithm4, and hybrid algorithm5) are remarkably consistent, highlighting the growing maturity of CTO PCI, which in turn has enabled success rates of 85-90% at experienced centres around the world2 (Figure 1).
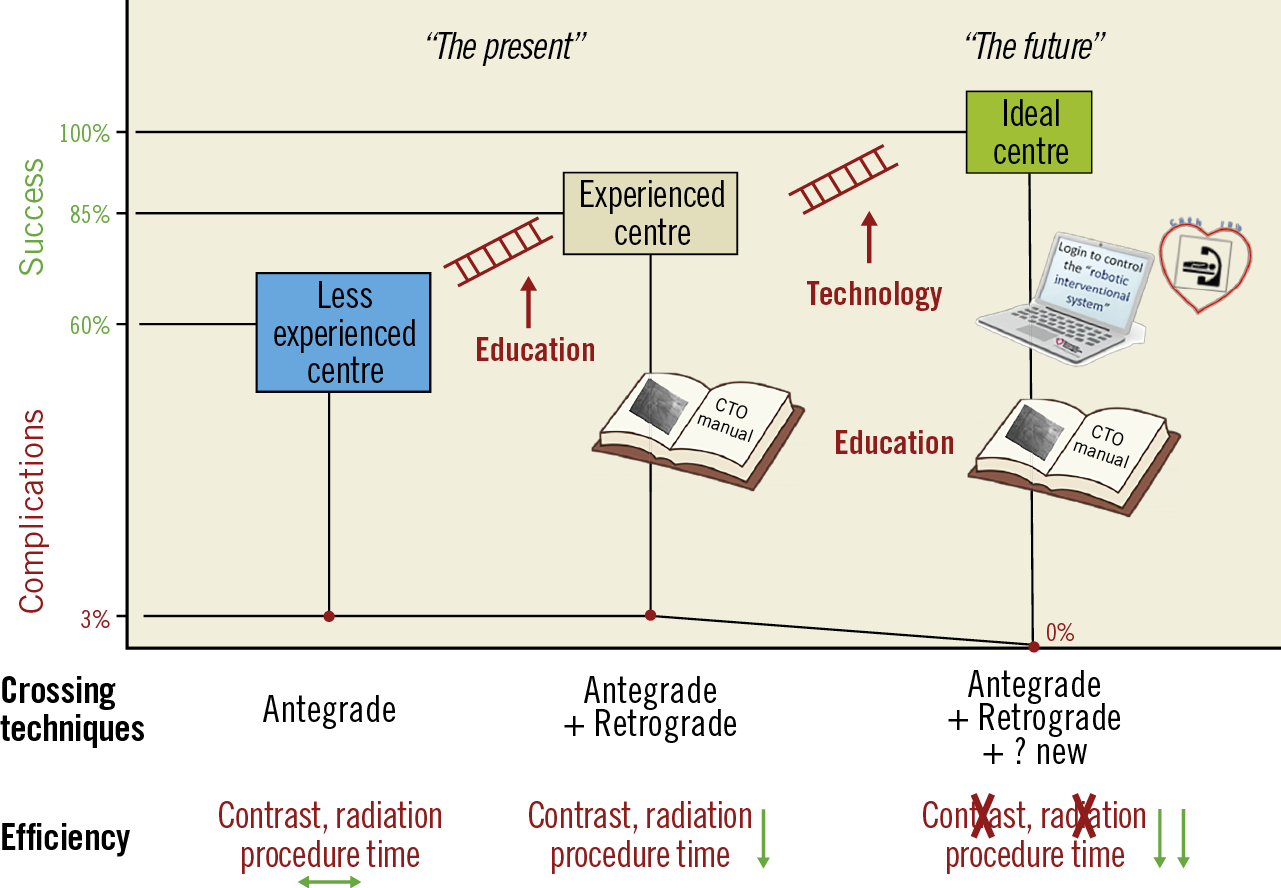
Figure 1. The present and the future of chronic total occlusion percutaneous coronary intervention.
Several challenges remain. First, success is still not 100% and the risk of complications can increase significantly with aggressive manipulations in complex CTOs. Second, complications still occur (in approximately 3% of cases), including death. Third, success rates at less experienced centres are 20-30% lower. Fourth, CTO PCI can still be laborious, requiring long procedure time, and high radiation and contrast doses. Fifth, although five randomised controlled trials have recently examined the potential benefits of CTO PCI, the evidence base remains relatively limited, with few new studies on the horizon. Sixth, in-stent restenosis still occurs in approximately 10% of patients.
The future
We have a dream: CTO PCI will be performed in patients who will all derive benefit, with 100% success and 0% complication rates, within 30 minutes with zero radiation dose and zero contrast, anywhere in the world and with 0% subsequent restenosis or stent thrombosis rates!
How can this dream become a reality? Innovative technology will clearly play a major role. Incremental improvements in guidewire and microcatheter design have already increased antegrade CTO PCI success rates and new solutions are on the horizon for treating calcified occlusions. Development of novel, simple to learn and perform, and highly efficacious and safe re-entry devices is needed, as is enhanced crossing guidance, either by intravascular or extravascular imaging. What is needed is a “game-changer”, such as a mini robot that locates the proximal cap, penetrates and advances through the occlusion with perfect precision, carrying with it the guidewire into the distal true lumen, and pre-treats the lesion to facilitate balloon and stent expansion. Such transformative technology, however, is not yet in sight and may be difficult to develop given the large variation in CTO anatomy and patient characteristics. New technologies are also needed for reducing radiation and contrast dose and increasing the efficiency of the procedure.
The value of education in CTO PCI cannot be overemphasised and can bridge the discrepant outcomes between experienced and less experienced centres. CTO PCI is a complex subspecialty of interventional cardiology and requires specialised training and practice to maintain competence: the EuroCTO Club is proposing an annual volume of 50 and 100 CTO PCIs per year for experienced and expert operators, respectively1. The CTO operator needs to develop and continually expand expertise in all CTO crossing techniques, as well as techniques to treat complex lesions (such as calcified and tortuous lesions), and complications. He or she should build a local catheterisation laboratory team dedicated to excellent outcomes and should also work closely with the advanced imaging and advanced heart failure teams.
Last, but not least, clinical research in CTO PCI needs to continue and expand, examining both the indications as well as the techniques and outcomes of the procedure. Determining whether CTO PCI can help to improve left ventricular function will require studying patients with decreased function at baseline and viable myocardium. The time for a sham-controlled CTO PCI trial is now. Studies on “hard outcomes” will be much more difficult to perform given the large number of high-risk patients that will need to be enrolled, many of whom (probably the ones with the highest risk) will likely decline participation in clinical studies. The ongoing NOrdic-Baltic Randomized Registry Study for Evaluation of PCI in Chronic Total Coronary Occlusion (NOBLE-CTO, NCT03392415) and Nordic and Spanish Randomized Trial on the Effect of Revascularization or Optimal Medical Therapy of Chronic Total Coronary Occlusions With Myocardial Ischemia (ISCHEMIA-CTO, NCT03563417) may provide some answers, but results are not anticipated until after a decade.
Making the journey from less experienced to experienced, and from experienced to ideal will take time (Figure 1). That is why now is the time to start! Using the EuroCTO consensus document and the multiple widely available resources can help make the ideal CTO PCI dream a reality!
Conflict of interest statement
E. Brilakis reports consulting/speaker honoraria from Abbott Vascular, American Heart Association (associate editor Circulation), Boston Scientific, Cardiovascular Innovations Foundation (Board of Directors), CSI, Elsevier, GE Healthcare, Infraredx, and Medtronic, research support from Regeneron and Siemens, being a shareholder in MHI Ventures, and being on the Board of Trustees of the Society of Cardiovascular Angiography and Interventions. M.N. Burke reports being a consultant to Abbott Vascular and being a shareholder in MHI Ventures. The other author has no conflicts of interest to declare.

