
Chronic total occlusion (CTO) of a coronary artery remains a challenging condition with regard to percutaneous coronary intervention (PCI). Whilst approximately 20%1 of patients with coronary disease undergoing diagnostic angiography have a documented CTO, only 5% of PCI is for CTO lesions across different healthcare systems, with little change in the overall percentage attempted over the last eight years2,3. Success rates have increased at a rate of 1%4 per year overall and are now over 90% in experienced centres. At the same time, complication rates have fallen steadily4. Often the main reason for not offering a CTO PCI to an individual patient is based on the expectation of procedural success rather than the underlying clinical indication.
The Japanese CTO (J-CTO) score is simple to calculate. It is also the most widely used, validated, preprocedural clinical and angiographic scoring system to assess lesion complexity5. In the Multicenter CTO Registry from Japan5, the predictors of prolonged procedures were the proximal cap appearance (tapered or blunt), lesion length (greater or less than 20 mm), tortuosity within the CTO (defined as a >45° bend), calcification within the CTO (any amount), and a previous unsuccessful attempt.
In the initial report, a J-CTO score of 0 or 1 (a straightforward CTO, often short in length and without calcification or tortuosity) was crossed with antegrade wire-based strategies within 30 minutes >90% of the time5. Other CTO registries have also reflected very high procedural success rates for these simpler lesions. Higher J-CTO score lesions (>2) indicate a more complex anatomy where wire-based antegrade strategies are less effective in long, calcified and tortuous lesions. The need for more specialised techniques, such as the retrograde dissection and re-entry (RDR or reverse CART) and the antegrade dissection and re-entry (ADR) using dedicated equipment (e.g., CrossBoss™ Catheter/Stingray™ System; Boston Scientific, Marlborough, MA, USA), increases overall success rates in these lesions in our experience (Figure 1)6.
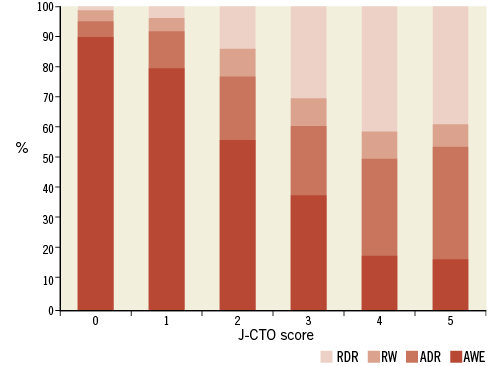
Figure 1. As J-CTO score increases (longer, tortuous and more calcific anatomy) there is a greater need for additional CTO techniques to maintain high success rates. ADR: antegrade dissection re-entry; AWE: antegrade wire escalation; RDR: retrograde dissection re-entry; RW: retrograde wire escalation.
There is a well-recognised reduction in success rates and increased procedural time, contrast and radiation use as the J-CTO score increases. In the current issue of the journal7, Tanaka et al add to this by showing that, in addition to crossing times, the J-CTO score appears to correlate with long-term success.
Despite its simplicity and effectiveness, the J-CTO score has only recently been used in some registries. It is not routinely used in clinical practice.
A major change in approach to CTO lesions in recent years has been to introduce a structured approach to these complex lesions. The hybrid approach is a systematic algorithm-led PCI strategy based on the identification of key anatomical features on baseline angiography8. The main aim is to provide a reproducible and teachable approach to CTO PCI (Figure 2). In addition, procedures should be targeted to be safe, with minimal exposure to contrast and radiation. Recently, the Asia-Pacific CTO group developed an algorithm which shares similar aims, although this integrates regional variance in practice whilst recognising the geographic and financial reality that new equipment will not be available in some regions. This was presented in oral format at the most recent TCT meeting. Interestingly, the authors propose that if the J-CTO score is >2 then the case should be referred to an expert or be performed with an expert present, hopefully increasing overall success rates. They also adhere to the ethos that a systematic approach using reproducible and teachable techniques is desirable for roll-out.
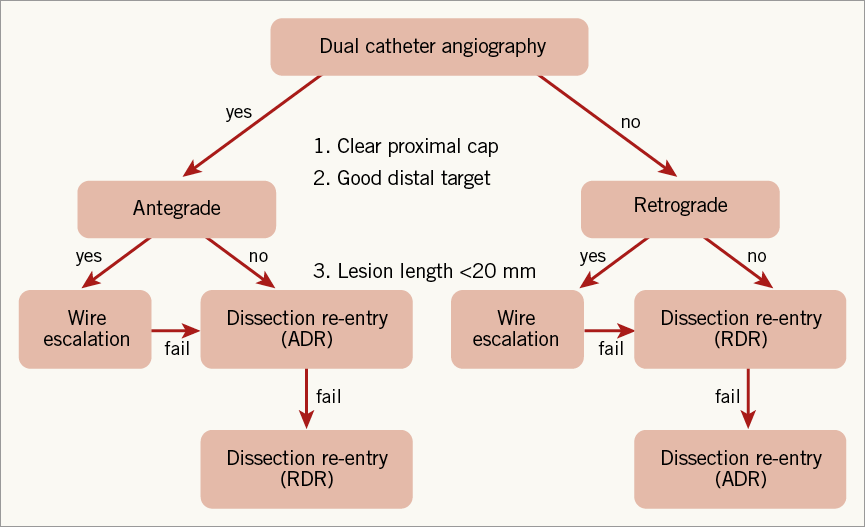
Figure 2. The hybrid algorithm for CTO PCI. The initial approach is based on anatomical features, with a switch from a failing strategy advised at an early stage. The main role is in novice rather than experts’ hands. ADR: antegrade dissection re-entry; RDR: retrograde dissection re-entry
We have recently demonstrated that it is possible to increase not only the procedural success rates but also the overall number of patients treated in a relatively short period of time (six months) after physician education, and in particular proctoring9. This was driven mainly by an increase in success for patients with J-CTO scores ≥2 (70.7% vs. 49.5%, p=0.0003) (Figure 3).
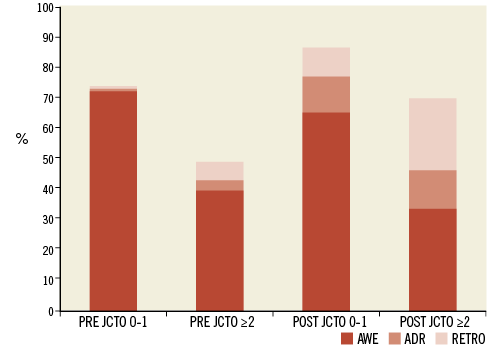
Figure 3. Physician education and proctor-based training result in not only additional numbers being treated but also increased success rates for patients, especially in the more complex anatomical groups. ADR: antegrade dissection re-entry; AWE: antegrade wire escalation; RETRO: combined retrograde techniques (wire escalation and dissection re-entry). Reprinted with permission. © (2015). BMJ. All rights reserved
In our opinion, the key elements to successful CTO PCI are the following: 1) the development of a programme with full team involvement and moving away from ad hoc CTO PCI; 2) physician and staff education to help understand lesion complexity, techniques and objectives that have procedural safety as the central core; 3) learning from live or recorded cases and workshops to enhance understanding of equipment and techniques; and 4) proctoring – preferably with the proctor able to scrub-in for the case to move beyond technically challenging or potentially limiting steps in the procedure and thus allow the host physician to gain hands-on experience from all aspects of the CTO PCI, particularly the parts of the procedure that may not have been reached otherwise.
Many groups, including the Euro CTO Club, US, UK and European hybrid operators, plus the Japanese experts, have been involved in teaching and training for many years, which is having a very positive effect on practice. However, further work is still required. In our view, the ultimate aim must be to increase the total number of patients offered a CTO PCI rather than focusing on marginal increases in success rates in expert and subspecialist centres10. Thereby, a greater total number of patients will be treated, leading to a reduction in symptoms and an improved quality of life for a much broader cohort.
Conflict of interest statement
The authors have no conflicts of interest to declare.

