Abstract
During recent years, equipment and techniques for percutaneous coronary intervention (PCI) of chronic total occlusions (CTO) have improved significantly. The retrograde approach remains critical to the improved success of CTO PCI. Currently, the reverse controlled antegrade and retrograde tracking (CART) technique has become the dominant retrograde wire crossing technique. In this article, we propose a standardised terminology and classification for this technique divided into three subtypes: a) conventional reverse CART, usually involving the use of large balloons on the antegrade wire to achieve re-entry within the CTO segment; b) “directed” reverse CART, which is characterised by small antegrade balloon size and more active, intentional vessel tracking and penetration with a controllable retrograde wire, still within the CTO segment; and c) “extended” reverse CART, in which the intimal/subintimal dissection is extended proximal or distal to the CTO segment, achieving re-entry outside the CTO segment. The proposed standardised terminology will facilitate the communication, teaching and adoption of the reverse CART techniques.
Abbreviations
CART: controlled antegrade and retrograde tracking
CTO: chronic total occlusions
IVUS: intravascular ultrasound
PCI: percutaneous coronary intervention
Introduction
Chronic total occlusions (CTO) are one of the most challenging lesion subsets in percutaneous coronary intervention (PCI)1. During the past two decades, there has been significant progress in equipment and techniques2-7, resulting in significant improvements in success rates of CTO PCI8-15. One of the most important advances was the introduction and subsequent evolution of retrograde techniques.
The retrograde approach was first applied for the treatment of CTO by the expert Japanese CTO PCI operator Dr Osamu Katoh in the early 1990s. Early retrograde approaches focused on direct retrograde wire crossing and the kissing wire technique. However, the modern era of retrograde CTO PCI began in the mid 2000s when Katoh’s group reported the development of the controlled antegrade and retrograde tracking (CART) technique5 and the septal dilatation technique16.
In the CART technique, a balloon is advanced over the retrograde guidewire and inflated to create a localised subintimal dissection within the CTO segment. The antegrade guidewire is then advanced from the proximal true lumen into this subintimal space and subsequently into the distal true lumen. Although the CART technique is often successful, the technique has a number of limitations. First, it is sometimes impossible to cross or dilate small and tortuous septal channels. Then, septal dilatation carries the risk of septal injury, and retrograde passage of balloons through epicardial collateral channels carries considerable risks of channel rupture or balloon trapping and should generally be avoided. Finally, in the CART technique, retrograde balloon inflation is performed within the CTO segment to make a subintimal dissection without information about vessel size or the position of the retrograde guidewire. In the CART technique, formation of the retrograde subintimal dissection cannot be confirmed by intravascular ultrasound (IVUS), resulting in technical uncertainty and potentially increased risk.
The introduction of the Corsair microcatheter (Asahi Intecc, Aichi, Japan)17 resulted in a major improvement of the retrograde approach along with development of the reverse CART technique. Use of the Corsair or other microcatheters for retrograde channel crossing largely eliminates the need for balloon dilatation of collateral channels, reducing the risk of septal injury and allowing greater use of epicardial channels. In addition, these microcatheters facilitate exchange of the retrograde guidewire, improve retrograde guidewire support and improve guidewire handling. In the reverse CART technique, a balloon is advanced into the CTO segment over the antegrade guidewire and inflated to create a localised subintimal dissection inside the CTO segment. The retrograde guidewire supported by the retrograde microcatheter is then advanced from the distal true lumen into this subintimal space and then into the proximal true lumen. As the reverse CART technique is quicker, easier and safer than the CART technique, it has become the dominant guidewire crossing technique in current retrograde CTO PCI, as summarised in Table 1 18-26.
Since the introduction of the reverse CART technique, several subtypes of the technique have been developed to improve procedure success and efficiency. Most recently, the introduction of the Gaia series of guidewires (Asahi Intecc), which have excellent torque control, has led to a novel modification of the reverse CART technique. However, the present terminology for these techniques does not necessarily reflect the concept behind each retrograde technique, which can result in confusion and inappropriate technique and equipment selection. During the 18th Seminar of Angioplasty of Chronic Total Occlusion (CTO Club) held on 3 June 2017 in Nagoya, Japan, new terminology for the current reverse CART techniques was discussed by experienced CTO PCI operators from Europe, Asia-Pacific and the USA. The aim of this article is to define the major subtypes of the reverse CART technique currently in use and to propose a standardised terminology that appropriately reflects the concept of each technique.
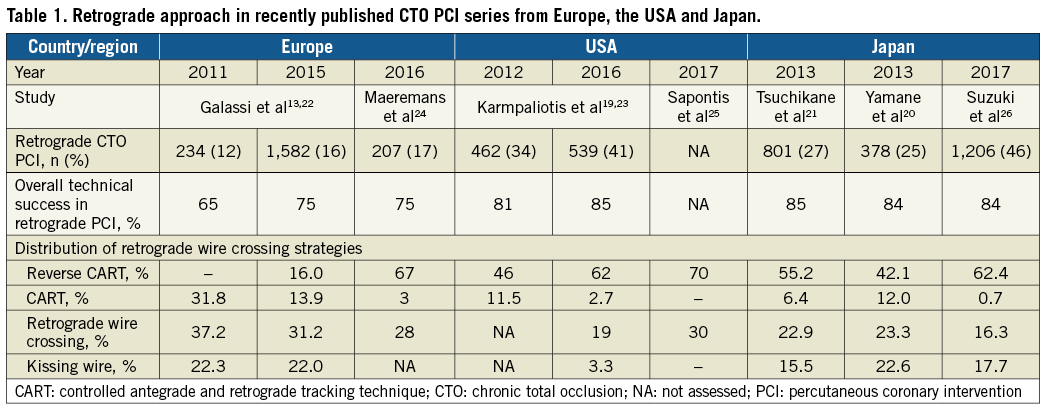
NEW CLASSIFICATION AND TERMINOLOGY FOR THE CURRENT REVERSE CART TECHNIQUES
We propose a standardised terminology and classification of the reverse CART technique divided into three major subtypes: a) conventional reverse CART, in which increasingly larger antegrade balloons are used to achieve re-entry within the CTO segment; b) “directed” reverse CART, which is characterised by the use of small antegrade balloons and more active, intentional vessel tracking and penetration with a controllable retrograde wire still within the CTO segment (this technique is currently referred to as “contemporary reverse CART”); and c) “extended” reverse CART, in which the intimal/subintimal dissection is extended proximal or distal to the CTO segment, achieving re-entry proximal or distal to the CTO segment (Figure 1).
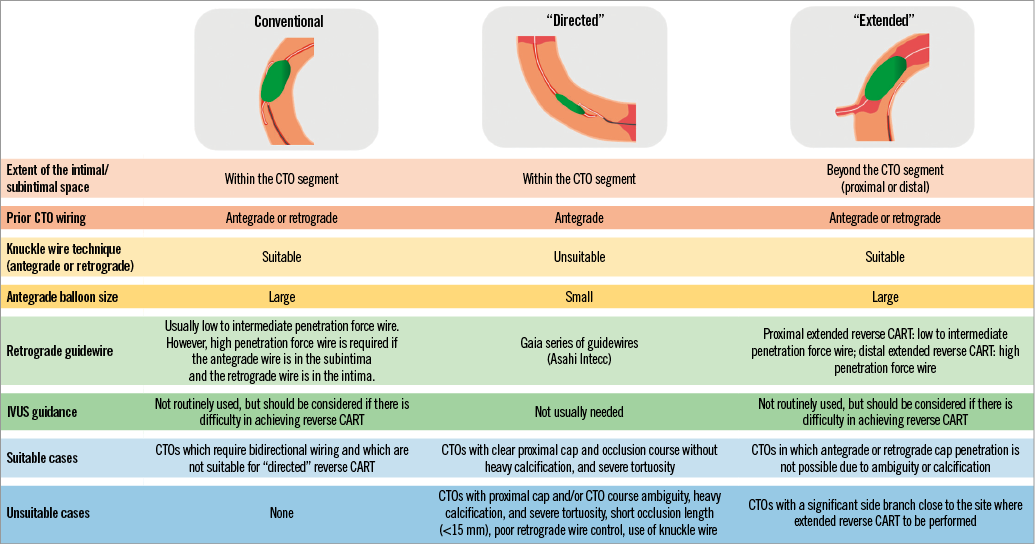
Figure 1. Overview of the three subtypes of the reverse CART technique. The essential elements of each technique are described in terms of extent of the intimal/subintimal space, prior CTO wiring, use of knuckle wire technique, antegrade balloon size, necessity of IVUS guidance, suitable and unsuitable cases.
a) CONVENTIONAL REVERSE CART TECHNIQUE
The first step of the conventional reverse CART technique (Figure 2, Supplementary Figure 1, Moving image 1) is to make a longitudinal overlap of the antegrade and retrograde guidewires. Where a vessel course within a CTO segment is unambiguous, conventional wiring in both an antegrade and a retrograde manner is feasible to make an overlap. However, where there is vessel course ambiguity, severe tortuosity or heavy calcification within the CTO segment, conventional wiring not only takes time but also carries the risk of vessel perforation. In these cases, knuckle wiring with low to intermediate penetration force polymer-jacketed guidewires can be more efficient and safer, as recommended in the Asia Pacific Chronic Total Occlusion Club main algorithm27. After achieving overlap of the guidewires, an antegrade balloon sized based on angiography is delivered into the CTO segment to the point of guidewire overlap and inflated. Balloon inflation makes or enlarges intimal/subintimal dissection and creates a connection between the spaces within which both guidewires are lying. In the conventional reverse CART technique, a large size antegrade balloon is selected to maximise the chance of creating a connection between the antegrade and retrograde spaces. Usually, a low to intermediate penetration force wire is used as the retrograde wire to track the created connection. However, if the antegrade wire is in the subintimal space and the retrograde wire is in the intimal space, a high penetration force wire is needed to advance through the intimal plaque into the subintimal space.
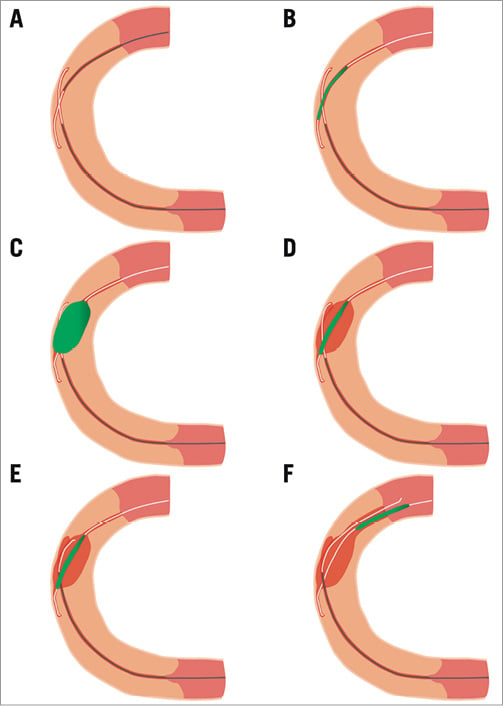
Figure 2. Illustration of procedural steps of the conventional reverse CART technique. A) A case of proximal RCA CTO. A longitudinal overlap of the antegrade and retrograde guidewires is made. B) A balloon is delivered over the antegrade guidewire to the point of guidewire overlap. C) The balloon is inflated. D) After balloon dilatation, a connection is created between the spaces containing both guidewires. E) A retrograde guidewire is advanced through the connection. F) The retrograde guidewire is subsequently advanced into the proximal true lumen.
If there is difficulty in achieving reverse CART, antegrade IVUS examination should be considered. IVUS provides information about the position of antegrade and retrograde guidewires (intimal or subintimal), vessel size within the CTO segment, plaque characteristics between both guidewires (soft, dense fibrous, calcific), and it can help to determine the optimal balloon size and the most favourable longitudinal point where an intimal/subintimal dissection and a subsequent connection can be created. Moreover, IVUS provides confirmation that the antegrade and retrograde spaces are connected after balloon inflation and allows real-time guidance of the retrograde guidewire passage through the intimal/subintimal connection (IVUS-guided reverse CART technique)6.
b) “DIRECTED” REVERSE CART TECHNIQUE
In the conventional reverse CART technique, as the intimal/subintimal space is intentionally dilated usually with a large balloon, excessive intimal/subintimal dilatation carries the risks of distal extension of the subintimal haematoma and vessel perforation. Recent reports have suggested that the CART and conventional reverse CART techniques could be associated with subsequent coronary artery aneurysm formation and increased risk for target vessel revascularisation due to longer stent length28,29. Moreover, excessive manipulation of the retrograde guidewire or use of a knuckle wire technique to achieve guidewire overlap can create a large space around the retrograde guidewire, which may hinder the directional control of the retrograde guidewire. The solution to this challenge in the conventional reverse CART dogma is intimal/subintimal dilatation with a larger balloon and tracking with low to intermediate penetration force guidewires. However, this can often be difficult and time-consuming.
The “directed” reverse CART technique (Figure 3, Supplementary Figure 2, Moving image 2) was introduced to minimise trauma to the vessel wall and to make the procedure more efficient through excellent directional control of the retrograde guidewire. The three key characteristics of this technique are the following: 1) antegrade preparation is performed first; 2) use of a small antegrade balloon as a target for the retrograde wire; and 3) retrograde intentional vessel tracking using a guidewire with high torque control.
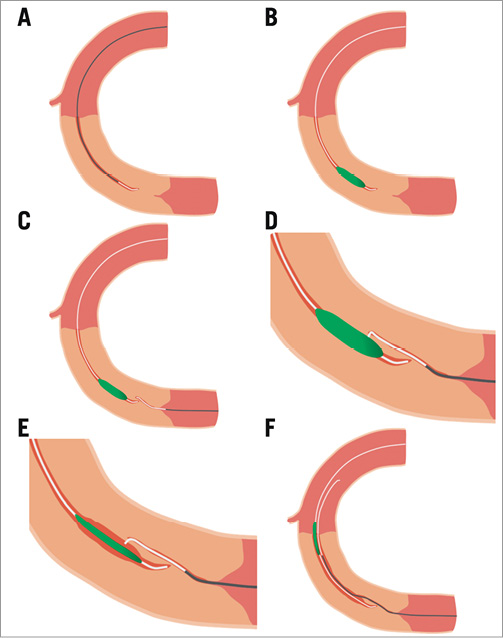
Figure 3. Illustration of procedural steps of the “directed” reverse CART technique. A) A case of mid RCA CTO. Antegrade preparation: an antegrade guidewire is advanced through the occlusion until 5-10 mm proximal to the distal cap with the support of a microcatheter. B) A small balloon is advanced to the tip of the antegrade guidewire. C) After the collateral channel crossing by a guidewire and a microcatheter, the retrograde guidewire is advanced towards the antegrade balloon. D) The retrograde guidewire is directed towards the antegrade balloon catheter (the lateral side of the balloon in this Figure) and gently pushed. E) After balloon deflation, the retrograde guidewire is advanced into the space created by the balloon. F) The retrograde guidewire is advanced into the proximal true lumen with sequential antegrade balloon inflation within the CTO segment proximal to the connecting point.
The first step of the “directed” reverse CART technique is antegrade preparation. After simultaneous dual contrast injection from the antegrade and retrograde guiding catheters, an antegrade guidewire is advanced through the occlusion with the support of a microcatheter to within 5 to 10 mm of the distal cap. The antegrade guidewire should not be advanced beyond the CTO segment to minimise the risk of distal haematoma formation. Next, the microcatheter is exchanged for a small balloon (2.0 mm diameter in most cases) which is advanced towards the tip of the guidewire. Unless there is proximal cap ambiguity that cannot be overcome with IVUS or if availability of collateral channel crossing is deemed uncertain, antegrade preparation first is reasonable as it reduces donor artery risk and ischaemic time of the CTO territory, and encourages going directly to reverse CART after retrograde channel crossing.
The retrograde approach is then commenced. After collateral channel crossing by guidewire and microcatheter, retrograde CTO segment wiring is performed using a guidewire with good torque control and high penetration efficiency. The Gaia guidewires are the preferred guidewires as they encompass these characteristics. The retrograde guidewire should be advanced without excessive torqueing and directed towards the antegrade balloon catheter as follows: 1) the shaft of the antegrade balloon and the retrograde guidewire should be as coaxial as possible at the point of puncture; and 2) retrograde puncture should be attempted towards the end of the balloon first (the so-called end balloon wiring technique) and, if this fails, towards the lateral side of the antegrade balloon. Fluoroscopy in two orthogonal projections or rotational fluoroscopy is useful to confirm the positional relationship between the retrograde guidewire and the antegrade balloon. After gently pushing the retrograde guidewire, the antegrade balloon is deflated, allowing the retrograde guidewire to puncture into the space created by the antegrade balloon.
In this technique, IVUS guidance is not usually required as the retrograde wire is intentionally directed towards and then into the space created by the antegrade balloon under fluoroscopic guidance. However, if there is difficulty in achieving a connection, it is reasonable to move on to an IVUS-guided reverse CART technique.
We suggest that the “directed” reverse CART should be considered as the first-line subtype of current reverse CART techniques in cases with suitable anatomy due to increased efficiency and reduced trauma to the vessel wall. As this technique requires antegrade preparation before starting the retrograde CTO segment wiring, and the knuckle wire technique cannot be used to advance the antegrade or retrograde guidewire as it creates large spaces around the guidewires resulting in reduced retrograde wire control, the “directed” reverse CART technique is not recommended in CTO cases with proximal cap and/or CTO course ambiguity that cannot be resolved, severe tortuosity, and heavy calcification. Also, CTOs with short occlusion length (<15 mm) are not suitable for the “directed” reverse CART technique, because antegrade preparation is difficult without extending the haematoma beyond the distal cap. Short CTOs may be best approached with antegrade or retrograde wire escalation. Similarly, if torque control of the retrograde guidewire is poor due to tortuosity of collateral channels or strong cardiac motion, the “directed” reverse CART may not be feasible. A long occlusion length alone is not necessarily a contraindication to the “directed” reverse CART technique, because antegrade preparation can be performed safely with conventional wiring if the vessel course within the CTO segment can be defined with landmarks such as calcification, previous stents, visible channels, or information from coronary computed tomography angiography.
c) “EXTENDED” REVERSE CART TECHNIQUE
In the “extended” reverse CART technique (Figure 4, Supplementary Figure 3, Moving image 3), the antegrade balloon is inflated proximal or distal to the CTO segment (outside the CTO segment) and the intimal/subintimal dissection is extended beyond the CTO segment. Thereafter, the retrograde guidewire is advanced through the connection created between the proximal true lumen and the retrograde intimal/subintimal space beyond the CTO segment. To create an intimal/subintimal dissection efficiently with antegrade balloon inflation, it is important to identify the ideal point with diffuse plaque and to determine an appropriate balloon size based on angiography. As with the “directed” reverse CART technique, IVUS guidance is not routinely required in this technique. However, if there is difficulty in achieving reverse CART, IVUS guidance can be helpful to facilitate successful wire crossing.
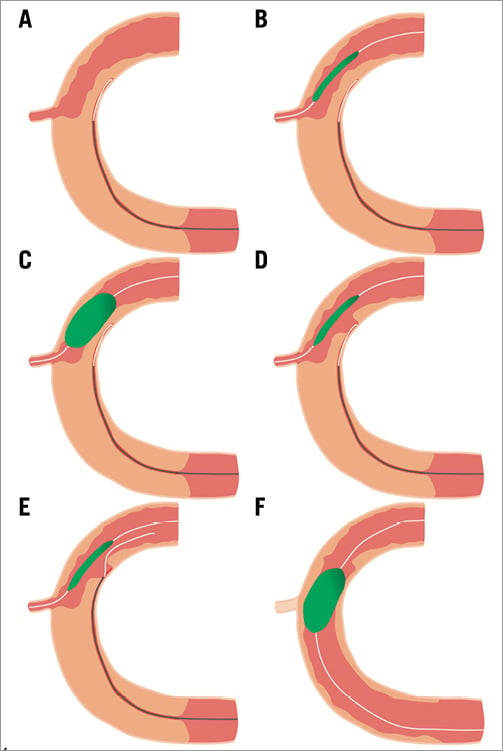
Figure 4. Illustration of procedural steps of the “extended” reverse CART technique. A) A case of mid RCA CTO with a small side branch around the proximal cap. A retrograde guidewire is advanced into the subintimal space. B) An antegrade balloon is delivered to the planned connecting point. C) The antegrade balloon is inflated in an attempt to create a medial dissection. D) After balloon deflation, a connection is created between the retrograde subintimal space and the proximal true lumen. E) The retrograde guidewire is advanced into the proximal true lumen through the created connection. F) After guidewire externalisation and balloon dilatation, the small branch is often compromised.
Alternatively, this technique can also be applied if there is failure of retrograde penetration of a calcified distal cap or if the retrograde microcatheter cannot pass severe calcification. In such scenarios, the antegrade guidewire can be placed in the subintimal space beyond the distal cap. After antegrade balloon inflation, often supported by guide-extension catheters, a high penetration force guidewire is used retrogradely to puncture into the dilated subintimal space.
We suggest using the “extended” reverse CART technique in cases where antegrade preparation or retrograde cap penetration is not possible and where there are no significant side branches close to the site of the “extended” reverse CART technique. CTOs with significant side branches between the points where we intend to create the intimal/subintimal dissection with the antegrade balloon and the proximal cap may not be appropriate for the “extended” reverse CART technique, as the branches may be lost after the retrograde guidewire re-enters into the proximal true lumen through the connection.
USEFULNESS OF STANDARDISED TERMINOLOGY AND CLINICAL IMPACT OF PROPOSED SUBTYPES OF THE REVERSE CART TECHNIQUE
The definitions and standardised terminology which are proposed in this article more accurately reflect the procedural concepts and characteristics compared to existing terminologies. This standardised terminology for the current reverse CART techniques will facilitate communication between CTO operators, and teaching and adoption of appropriate wire crossing techniques, but prospective validation will be needed.
Though the efficiency of the “directed” reverse CART technique is anticipated to be superior to that of the conventional reverse CART technique, it has not been examined. The “directed” reverse CART technique may help to prevent some of the potential complications of the conventional reverse CART technique such as coronary artery aneurysm formation and increased risk for target lesion revascularisation due to extended stent length, but this remains to be proven. Future studies are required to validate this technique.
Conclusions
The reverse CART technique has evolved significantly over time with the introduction of new dedicated equipment and techniques. We propose a new classification of the current reverse CART techniques divided into three major subtypes and a standardised terminology to describe these: conventional reverse CART, “directed” reverse CART, and “extended” reverse CART. We believe that this new classification and terminology will reduce confusion and help operators to understand the underlying concepts and the procedural steps of each technique. This in turn will aid appropriate selection and application of these wire crossing techniques and also facilitate communication and teaching. Prospective validation of the usefulness of the classification and terminology and examination of the clinical impact of the proposed techniques are required.
| Impact on daily practice The proposed definitions and standardised terminology for the current reverse CART techniques will help operators to select wire crossing techniques appropriately and also facilitate communication and teaching of the reverse CART techniques. |
Conflict of interest statement
E. Tsuchikane is a consultant for Boston Scientific, Asahi Intecc and Nipro. S. Harding has received speaker and consultancy fees from Boston Scientific, Medtronic, Bio-Excel and Asahi Intecc. E. Wu has received proctoring fees from SJM and has stock ownership in Abbott and Medtronic. E. Brilakis has received consulting/speaker honoraria from Abbott Vascular, ACIST, Amgen, Asahi, Elsevier, CSI, GE Healthcare, Medicure and Nitiloop and research support from Boston Scientific and Osprey. K. Mashayekhi has received consulting/speaker honoraria from Asahi Intecc and Vascular Solutions. G. Werner has received speaker’s honoraria from Abbott Vascular, Asahi Intecc, Boston Scientific, IMDS, and Terumo. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary Figure 1. A case example of the application of the conventional reverse CART technique.
Supplementary Figure 2. A case example of the application of the “directed” reverse CART technique.
Supplementary Figure 3. A case example of the application of the “extended” reverse CART technique.
Moving image 1. Application of the conventional reverse CART technique for the proximal RCA CTO.
Moving image 2. Application of the “directed” reverse CART technique for the proximal LAD CTO.
Moving image 3. Application of the “extended” reverse CART technique for the proximal RCA CTO.
To read the full content of this article, please download the PDF.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Application of the conventional reverse CART technique for the proximal RCA CTO.
Moving image 2. Application of the “directed” reverse CART technique for the proximal LAD CTO.
Moving image 3. Application of the “extended” reverse CART technique for the proximal RCA CTO.