- chronic total occlusion
- computed tomography coronary angiography
- radiation exposure
Abstract
Aims: We investigated the use of the CROSSER catheter, a CTO crossing device based upon high frequency mechanical vibration, as a first resort to treat patients with chronic total occlusions (CTO) while describing angiographic and computed tomography coronary angiography (CTCA) serving as predictors for success.
Methods and results: Eighty consecutive patients were enrolled in this prospective multicentre registry of patients treated for a CTO. For 76.3% of the patients, this was the first attempt to open the CTO. Overall success rate was 75%. By conventional coronary angiography, the length of the occlusion was 26.7±14.1 mm and there was a difference in successful vs. unsuccessful cases (24.5±13.9 and 32.8±13.1, p=0.02). The presence of angulation, as defined qualitatively, was more prevalent in failed cases (60.0% vs. 32.2%, p=0.03). The mean ratio CROSSER distance within the occlusion site and length of the occlusion showed a trend towards statistical significance in successful procedures (0.56±0.90 vs. 0.30±0.34, p=0.08). During hospitalisation, two patients had a non-fatal myocardial infarction. One patient experienced delayed onset of tamponade six hours postprocedure. At 30 days, two patients had PCI in a non-treated vessel and one patient had a transient ischaemic attack. Relation to the CROSSER catheter was inconclusive.
Conclusions: The success rate of the use of a dedicated-CTO device –the CROSSER catheter– as a first choice to open a chronic total occlusion was 75%. By multivariate analysis, in a subset of patients that were imaged with computed tomography coronary angiography, the absence of angulation was related with higher success rate.
Abbreviations
CCA conventional coronary angiography
CTCA computed tomography coronary angiography
CTO chronic total occlusion
PCI percutaneous coronary intervention
Introduction
Since success rate has remained unchanged over the last decade, there has been a decrease in the number of attempted percutaneous coronary interventions (PCI) in patients with chronic total occlusions (CTO).1 In the search for new therapeutic approaches to re-open the occluded vessel many new CTO-dedicated guidewires and devices have become available.2
Recently, the CROSSER catheter (Bard Peripheral Vascular, Tempe, AZ, USA) has emerged as an adjunctive therapy to facilitate crossing of totally occluded lesions. The CROSSER system utilises high-frequency mechanical vibration to penetrate atherosclerotic plaque material to cross CTOs in patients.3,4 This high frequency vibration has the power to penetrate plaque with a limited amplitude which prevents vessel perforation. The CROSSER catheter is mechanically connected to a generator that converts AC current into high-frequency vibration (20 kHz) that is propagated to the 1.1 mm blunt, stainless steel tip on the CROSSER catheter. Vibration is propagated from the generator to the tip through a tapered nitinol transmission wire. The CROSSER catheter is advanced over any standard 0.014-inch wire to the proximal cap of the occlusion. The wire is then withdrawn into the monorail guidewire lumen of the catheter and the system is activated by depressing a footswitch. Saline is infused through the central lumen of the catheter during activation at a rate of 18 ml per minute to provide cooling of the system and a medium for cavitation at the tip. Gentle forward pressure is applied to the catheter to cross the occlusion. Once the CROSSER tip reaches the distal lumen, the guidewire is advanced and the CROSSER may be removed, leaving the 0.014-inch guidewire in place for delivery of subsequent therapeutic devices.
The CROSSER has been studied previously as a device to be utilised following failed guidewire attempts. To better define the role of the CROSSER in the treatment of patients with CTOs, we studied this device as a first choice; that is, before any guidewire was used, in a consecutive cohort of eligible patients who were scheduled for percutaneous recanalisation of a CTO. We investigated also angiographic and computed tomographic predictors of success.
Material and methods
Study population
Between February 2006 and June 2007, those eligible for this study included all consecutive patients presenting with symptomatic coronary artery disease due to a CTO. Specifically, patients without contra-indications for the CROSSER, suitable for percutaneous treatment who had provided written informed consent, were included.
In a subset of 33 patients, computed tomography coronary angiography, (CTCA) was performed using a 64-slice CT scanner (Sensation64; Siemens, Munich, Germany) prior to the procedure, in order to better understand the CROSSER mechanism of action. CTCA was considered contra-indicated in the following situations: irregular heart rhythm, inability to sustain a sufficiently long breath hold (15 seconds with the 64-slice or dual-source CT scanner), renal dysfunction (creatinine clearance <60 ml/min as defined with the Cockroft formula)5, hearing disability, and known contrast allergy.
A CTO was defined as either an occlusion on angiography with no antegrade filling of the distal vessel other than via collaterals or minimal antegrade flow (TIMI flow 0 or 1).6,7 All included patients had a native vessel occlusion estimated to be at least of one month duration based on either a history of sudden chest pain, a previous acute myocardial infarction in the same target vessel territory, or the time between the diagnosis made on coronary angiography and PCI. The type of CTO was either de novo or due to in-stent restenosis.
All interventional procedures were performed by operators who were highly experienced in the treatment of CTOs, with the interventional strategy left to the discretion of the operator, except for the use of the CROSSER, which the protocol dictated as the first option. While the intent of the registry was to study the CROSSER as a technology to be used first, before any aggressive wire attempts, an audit of all patient records revealed that 23.8% (n=19) of the cases had a prior documented, failed attempt to cross the target occlusion.
Technical success was defined as advancement of the CROSSER system into or through an occlusion and achievement of distal vessel guidewire position with any conventional 0.014” guidewire. Procedural success was defined as successful opening of the chronic occlusion and restoration of flow (<50% residual stenosis and TIMI 2-3 flow). Procedural failure was defined as the inability to cross the occlusion with a guidewire.
All patients were pre-treated with 300 mg of clopidogrel, which was continued at a dose of 75 mg/day for six months. All patients were advised to maintain aspirin (≥80 mg/day) lifelong. Follow-up was conducted during hospitalisation and 30 days post index procedure via an office visit or detailed telephone interview.
The protocol was approved by the local ethics committee and was in accordance with the principles of Good Clinical Practice for Trials of Medicinal Products in the European Community and the Declaration of Helsinki. All patients signed a written informed consent.
Definitions
Type of CTO: defined according to two characteristics, location (native vessel vs. graft) and quality (de novo or in-stent restenosis).
Occluded length: defined as the non-contrast enhanced segment of the vessel from the proximal to the distal end of the occlusion in the least foreshortened view on angiography or the 3-dimensional measurement of the occlusion using a dedicated software program (Circulation®; Siemens, Munich, Germany) of the CT workstation (Leonardo).
Stump morphology: defined as the entry site of the occlusion that has either a tapered (central or eccentric) or a blunt appearance.
Side branch at the entry site: defined as the presence of any side branch, irrespective of the size, within 3 mm proximal to the entry of the occlusion.8
Rentrop classification9: grading of collateral filling was as follows: 0=none, 1=filling of side branches only, 2=partial filling of the epicardial segment, 3=complete filling of the epicardial segment. This classification only applies for conventional angiography since in CTCA the distal part of the vessel is almost always filled with contrast and thus can be regarded as Rentrop class 2 or 3.
Tortuosity was defined as the presence of bends proximal to the lesion. By angiography, this feature was only scored in a binary fashion (yes/no), i.e., < or > than 45 degrees, while by CT, the angle of all the separate vessel bends was measured (Figure 1).
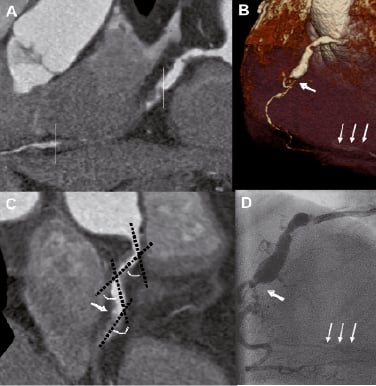
Figure 1. A) CT image (curved multiplanar reconstruction) of the right coronary artery (RCA). The proximal and distal part of the occlusion is marked by two lines. B) Volume-rendered CT image, showing the proximal (thick arrow) part of the occlusion and reappearance of the distal non-occluded part of the vessel (thin arrows). C) CT image (multiplanar reconstruction) showing the tortuosity of the vessel proximal to the occlusion. D) Appearance of the RCA on conventional coronary angiography. The proximal part of the occlusion is shown (arrowhead), while the distal part of the vessel is faintly visible (arrowheads).
Calcification was defined as follows:
–by conventional angiography, defined as mild, moderate or severe.
–by CTCA, the number of separate calcium spots was counted and their length measured (Figure 2).
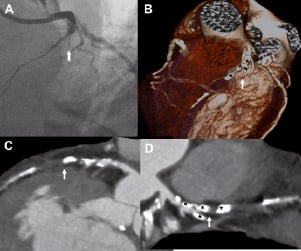
Figure 2. A) Conventional coronary angiogram, showing an occlusion of the proximal left anterior descending artery (LAD) (arrowhead). B)Volume-rendered CT image, showing that the LAD and second diagonal branch (D2) are occluded. The asterisks correspond to calcifications in the occluded parts of the vessel. C)CTimage (curved multiplanar reconstruction) of the LAD showing severe calcification in the proximal part of the occlusion. More distally the occlusion is non-calcified. D) Multiplanar CT reconstruction showing the location of the calcium deposits (asterisks) in the LAD and D2, corresponding to the findings in panel B.
Angulation was defined as the presence of bends within the occluded segment. By angiography, only a binary scoring system was used (presence of at least one bend or not), while by CT, the angle was measured in subsequent bends within the occlusion.
Conventional coronary angiography (CCA)
Angiographic analysis was performed by an independent corelab (Cardialysis, Rotterdam, The Netherlands) that was unaware of the results of the CT scans. Procedure films were available for all 80patients. In all these patients, quantitative angiographic analysis (CAAS II; Pie Medical, Maastricht, The Netherlands) was performed. The length of the occluded vessel segment was also quantified. The other variables, i.e., location of the occlusion, morphology of the stump, the presence of a side branch in the vicinity of the entry (<3 mm), collaterals and calcification were reported qualitatively.
CTCA patient selection, scan protocol and image reconstruction
A cardiac CT scan was performed in the fortnight before PCI. During the described study period, two successive scan generations were used in our centre. CT data were initially acquired using a 64-slice CT scanner (Sensation 64; Siemens, Munich, Germany) and from April 2006, on the latest dual-source CT scanner (Somatom Definition; Siemens, Munich, Germany) was used. Up to March 2006 we systematically slowed down the heart rate in patients with a heart rate above 65 bpm, using 100 mg metoprolol or a non-dihydropyridine calcium-antagonist (diltiazem 60-120 mg) orally one hour before the scan. An additional IV bolus of metoprolol (5-10 mg) was occasionally administered if the heart rate remained above 65 bpm. After that period we did not use extra medication to slow down the heart rate. Instead, nitrates were systematically given as a sublingual spray (0.4 mg) to all patients five minutes before initiation of the scan provided the systolic blood pressure was above 100 mmHg.
Scan parameters for each of the two scanner types were as follows:
– 64-slice CT scanner: collimation 64×0.6 mm, tube rotation time 330 ms, tube voltage of 120 kV, table feed 3.8 mm per rotation. For the non-enhanced scan we used a tube current of 150 mAs and applied prospective x-ray tube modulation. For the angiographic scan we used a tube current that ranged between 850 and 960 mAs without the use of dose pulsing.
– dual-source CT scanner: collimation 64×0.6 mm, tube rotation time 330 ms, tube voltage of 120 kV. For the non-enhanced scan we used a tube current of 84 mAs per tube and full X-ray tube current was given during 50-70% of the RR interval. For the angiographic scan we used a tube current of 412 mAs per tube and limited this amount of tube current to 25-70% of the RR-interval. Pitch values were adapted to heart rate (minimal pitch value of 0.2 for slow heart rates, up to a maximal pitch value of 0.45 with higher heart rates).
The contrast-enhanced scan was obtained after the intravenous injection of 70-100 ml of contrast material (iomeprol, 400 mg iodine/ml, Iomeron® with the 64-slice CT scanner or iopromide, 370 mg iodine/ml, Ultravist® with the dual source CT scanner) through a large antecubital vein at a flow rate of 4-5 ml/sec, followed by 40 ml of saline flush at 4 ml/s. A bolus tracking technique was used to monitor the appearance of contrast material in the ascending aorta. Once the signal in the ascending aorta reached a predetermined density level of 100 Hounsfield units, CT acquisition was automatically started during an inspiratory breath hold. Images were reconstructed using ECG-gating to obtain optimal, motion free image quality.
The scan data were reconstructed at various phases of the cardiac cycle using medium-to-smooth (B26f) and sharp (B46f) convolution kernel. Image reconstruction was retrospectively gated to the ECG. The position of the reconstructed window within the cardiac cycle was individually optimised to minimise motion artefacts. Datasets containing no or minimal motion artefacts were transferred to a remote workstation (Leonardo workstation, Siemens, Munich, Germany) for further evaluation.
CT data analysis
Two experienced observers independently evaluated the CT data sets on both the original axial images and on multiplanar reformatted reconstructions for the presence of an occluded vessel. This initial assessment was performed blinded to the angiographic data. Subsequently, the observer was provided with the angiographic information, i.e., the occluded vessel in which PCI was performed, without having access to the angiographic images. After confirmation of the right vessel, further CT analysis was performed without knowledge of the angiographic characteristics of the occluded vessel. On occasion, especially in case of heavy calcifications of the vessel, angiographic information on the start and end of the occlusion was provided to allow calculation of the occlusion length. To measure the length of the occlusion on CT, we used a dedicated software program (Circulation®, Siemens, Munich, Germany), that allows creating a central lumen line through the vessel. By rotating the vessel around this line the exact entry and exit point of the occlusion can be visualised, thus allowing measurement of the length of the occlusion along the 3-dimensional vessel path without foreshortening.
Statistical analysis
Assumptions for normality were checked by Kolmogorov-Smirnov test and by visual assessment of Q-Q plots of residuals. According to their distribution, the comparison of variables between groups was done with parametric or not parametric tests. Continuous variables are presented as mean ±1SD and differences were compared using the Student t test or Mann Whitney test, as appropriate. Categorical variables are presented as counts and percentages and differences were assessed by the Fisher exact test or chi-square test, as appropriate. A two-sided p value of less than 0.05 indicated statistical significance.
The following variables were included in the multivariable analysis dataset: conventional angiographic characteristics (TIMI flow pre [0 or 1], duration of occlusion [one or more than one month], ostial location, stump morphology, presence of bridging collaterals, presence of a side branch at the entry of the occlusion, degree of calcification and tortuosity [yes/no]), and CTCA characteristics (ostial location, stump morphology, presence of side branch at the entry of the occlusion, calcification, angulation, tortuosity and length of the occlusion). For the remainder of the variables, we ran a forward selection procedure. Statistical analyses were performed with use of SPSS 12 (SPSS Inc., Chicago, Il, USA).
Results
Baseline characteristics
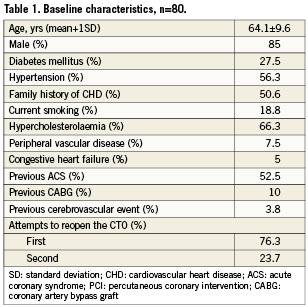
Eighty (80 CTOs) consecutive patients were enrolled in this prospective registry of patients treated for a chronic total occlusion.
The mean age was 64.1±9.6 years, and most of the patients were male (85%) (Table 1). For 76.3% of the patients, this was the first attempt to open the CTO. Most of the occlusions were de novo lesions and the most frequently treated coronary artery was the right coronary (61%) (Table 2). The minimum age of occlusion considered for inclusion in the protocol was one month. The average was 17 months with a majority of the patients (n=59) with documented evidence of occlusion age greater than three months. The success rate in patients with occlusions documented to be greater than three months was 74.6%. The overall success rate was 75%.
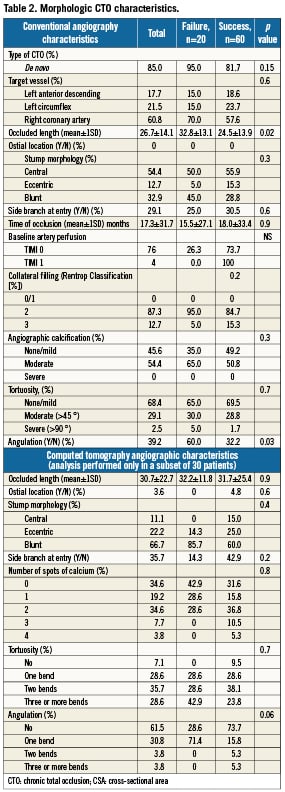
CTO characteristics by conventional coronary angiography and CTCA
By conventional coronary angiography, the length of the occlusion was 26.7±14.1 mm and there was a difference in successful vs. unsuccessful cases (24.5±13.9 and 32.8±13.1, p=0.02). The presence of angulation, as defined qualitatively, was more prevalent in failed cases (60.0 vs. 32.2%, p=0.03).
In the subset of patients who underwent CTCA imaging, the mean occlusion length was 30.7±22.7 mm. The occlusion length did not differ in successful as compared to failed cases (31.7±25.4 and 32.2±11.8, p=0.9). When using CTCA as an analysis tool, the absence of angulation in the occlusion showed a trend towards a favourable outcome: procedural success was 73.7% in CTOs without angulation as compared to 28.6% in angulated CTOs (p=0.06). By CTCA, calcium was present in 65.4% of the treated lesions. The number of calcium spots was not statistically different between the two groups (p=0.8).
In the multivariable analysis the only variable that remained asignificant predictor of procedural success, was the absence of angulation as defined by CTCA. (Table 2)
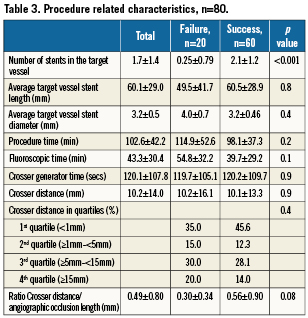
Procedure related characteristics (Table 3)
The fluoroscopic time was higher in the failed cases as compared to the successful cases, 54.8 versus 39.7 minutes, respectively, p=0.1. The mean ratio between the length of the occlusion crossed by CROSSER and the total length of the occlusion showed a trend towards statistical significance in successful procedures (0.56±0.90 vs. 0.30±0.34), p=0.08. In the successful procedure, stiff wires and micro catheters were used in 21.1% and 81.5% of the cases, respectively, while parallel wires and retrograde techniques were used in 27.2% and 6.1% of the cases, respectively, to gain complete success. In 14 patients a false lumen was observed after the use of CROSSER catheter. In three patients a perforation of the coronary vessel was observed during the recanalisation attempt but none during or immediately after use of the CROSSER. One patient had mild blush in the myocardium, while the other two had free flow into the pericardium. One patient required atamponade drain 6-7 hours after the procedure with no additional complications following. The other perforations required no additional clinical treatment beyond reversal of anticoagulation.
Clinical follow-up
During hospitalisation, two patients had a non-fatal myocardial infarction. At 30 days, two patients had PCI in a non-treated vessel and one patient had a transient ischaemic attack.
Discussion
In this registry of 80 patients we evaluated the possible role of the CROSSER catheter as a first choice when attempting PCI of CTOs. Despite the protocol requirement of using the CROSSER as a first attempt, 23.8% of the patients had a documented prior attempt with conventional wires. The overall success rate was 75%. Not unexpectedly, CTCA was more accurate than CCA for defining the complex morphological features of CTOs. In particular, we found that the assessment of angulation by CTCA, which by multivariate analysis was the only predictor of procedural success versus failure, was more reliable than by CCA.
Treatment of chronic total occlusions still remains one of the most demanding procedures in the field of interventional cardiology. In order to reduce the risk of complications for the patients and for the operators due to long-lasting procedures, new approaches and dedicated devices have been introduced. CTO wires (i.e., tapered-tip) appeared to be useful in selected cases.10 New strategies to treat CTOs such as the retrograde approach seem promising11; however, this procedure requires suitable anatomy, a specific armamentarium and generally are challenging procedures. However, these new tools and approaches need to be used thoughtfully and in our view in the right anatomical context by a careful evaluation of the operator. The CROSSER catheter is an interesting tool that may play a role in crossing some CTO lesions. In particular, in the present study, the absence of angulation, by CTCA, was the only independent predictor of CROSSER success. In light of these results, it appears that this device can be used, in association with other devices, in CTO lesions that appeared not to be severely angulated at a previous CTCA evaluation. It is noteworthy to consider, however, that the CTCA evaluation was obtained in a small subset of patients.
In a previous report8, the most common location of calcification was at the entry of the occluded segment. In this study it is interesting to note, that the CROSSER catheter, as measured by conventional angiography, could break the proximal cap and progressed as far as 50% of the occluded length. The further the device progressed the more likely it was to open the lesion. However, this may have been underestimated, because cineangiograms were not routinely performed when the CROSSER device was in its most distal position in the occlusion.
Clinical implications
In a registry in which all patients with CTOs were treated irrespective of anatomical characteristics of the occluded segments, several dedicated guidewires and devices were used with a success rate of 60.6%2. Recently, the CROSSER system has been used in patients in whom conventional guidewire methods have failed with a similar success rate (60.8%).12 The angiographic assessment in this study showed complex anatomical characteristics of the occluded segment; that is severe calcification, tortuosity, angulation or major branch at the site of occlusion and blunt occlusion shape. However, none of these angiographic variables appeared to be an independent predictor of success. This is at variance, with the finding in this report in which angulation by CTCA was found to be an independent predictor of success. We have found in two previous reports13,8 that severe calcification by CTCA is also an independent predictor. Thus, it appears that evaluation of CTO lesions is more accurate by CTCA. However, a word of caution should be mentioned, the cost/benefit of the incremental radiation exposure and contrast use by the routine evaluation by CTCA is not yet known.
In the present report, the CROSSER system was used as a first resource to open CTOs. The success rate was 75%, without any fatal procedure-related complications and excellent short-term clinical follow-up. In particular, the incidence of complications at 30 days (3.7%) was in line with other reports, ranging from 0% to 8.8%.12,14 These results may encourage the use of this device as a first choice in de novo as well as in refractory CTOs.
Limitations of the study
This study focuses on the angiographic predictors of success by conventional and CT angiography. However, only a subset of patients underwent CT angiography.
Conclusion
Use of the CROSSER device to penetrate the calcified cap of the occlusion prior to manipulation of any guidewires appears to be an effective strategy to recanalise long segment, calcified, chronic occlusions. In experienced centres the success rate of a percutaneous CTO recanalisation attempt is on average 70%7,15. In this study the overall success rate was 75% using the CROSSER device as the first technology to penetrate the CTO. In the absence of severe angulation by computed tomography coronary angiography, the CROSSER should be considered as the first option to treat chronic total occlusions.
Conflict of interest statement
The authors have no conflict of interest to declare.