Abstract
Aims: The retrograde approach to CTO is promising, but questions remain with regard to its wider application and the potential risks. This study evaluated the feasibility and efficacy of retrograde recanalisation of chronic total occlusion (CTO) of the coronary arteries.
Methods and results: A total of 378 consecutive patients (previously failed PCI 32.0%) who enrolled in 27 institutions in Japan underwent retrograde recanalisation for CTO. We analysed the data on lesion characteristics, procedural materials, technique used, complications and clinical outcomes. Successful retrograde recanalisation was achieved in 70.4% and the overall procedural success was 83.6%. Collateral crossing was achieved via a septal route in 68.9%, epicardial in 27.2% and bypass grafts in 2.6%, respectively. The retrograde approach was completed with implementation of reverse CART in 42.5%, direct wire crossing in 23.1%, bilateral wiring in 22.7%, and CART in 11.7%. Major and minor collateral injuries and coronary perforations were noted in 1.3%, 10.3% and 2.9% of cases, respectively. Stroke occurred in 0.3%, QWMI and emergency PCI in 0.3% of patients with successful recanalisation.
Conclusions: Wider application of retrograde CTO PCI achieved a high rate of success in recanalisation with an acceptable rate of complications in Japan.
Abbreviations
CABG: coronary artery bypass grafting
CART: controlled antegrade and retrograde subintimal tracking
CPK: creatine phosphokinase
CTO: chronic total occlusion
MI: myocardial infarction
PCI: percutaneous coronary intervention
TIMI: thrombolysis in myocardial infarction
Introduction
Despite the recent wider availability of certain devices, such as dedicated CTO wires, microcatheters, and re-entry devices1, and novel strategies, such as the parallel wire method2, intravascular ultrasound-guided PCI3,4 and the STAR technique5, they are used mainly by dedicated CTO operators. With the advent of drug-eluting stents and antiplatelet therapy, a marked reduction of target vessel revascularisation has been achieved compared with bare metal stents6. The same holds true in CTO PCI, from the procedure when the CTO was crossed with a guidewire and implanted with DES7.
Conventional antegrade CTO PCI remains suboptimal with a success rate of 65-70% worldwide8, 9, mainly due to the inability to pass the guidewire into the distal true lumen. A retrograde approach through well-developed collateral arteries was introduced to improve further the success rate of complex CTO10-12. In 2005, the CART (controlled antegrade and retrograde subintimal tracking) method was developed by Dr Osamu Kato: this consists of antegrade guidewire placement through the CTO site where retrograde balloon dilation creates a local subintimal dissection in order to facilitate wire crossing to the distal true lumen13. However, this novel approach is still limited in application to well-developed, accessible septal collateral channel cases. By 2008, the concept of a channel dilator materialised as the Corsair microcatheter (Asahi Intecc Co., Ltd, Aichi, Japan), which enables the operator to pass a guidewire to the distal end of the CTO through any type of collateral channel14. With this new microcatheter, reverse CART has gained popularity. Therefore, we studied how this series of evolving retrograde techniques has, in practice, been adopted in CTO centres in Japan, and we analysed the widespread utility with regard to the success rate, procedure-related complications and in-hospital outcomes.
Methods
PATIENT POPULATION AND STUDY PROTOCOL
From January 2009 to December 2009, planned PCIs were conducted in a total of 14,381 cases among the 27 institutions in Japan, and 1,542 (10.7%) cases were CTO PCI. Among them, 378 cases (24.5%; 378 CTO lesions) utilised a retrograde approach (Appendix 1). CTO PCI was indicated either for symptomatic relief or in the presence of ischaemia in the CTO distribution. The procedures were performed by board-certified interventional cardiologists, who had at least several years’ experience of CTO PCI and who had completed the retrograde course (the live demonstration and lectures) held in Japan. Informed consent was obtained in all cases according to the protocol of each institution.
DEFINITIONS
CTO was defined as a lesion with TIMI flow grade 0 of >3 months duration, estimated from symptom onset, change in angina status, history of MI and previous angiography. Q-wave and non-Q-wave myocardial infarctions (MI) were defined as consistent ECG changes, of a greater than threefold increase of a cardiac enzyme (creatine kinase-myocardial band, CK-MB), with or without the development of Q-waves, respectively.
CTO anatomy was evaluated by simultaneous double injection. Major collateral channel injury was defined as a collateral channel rupture or perforation which required specific treatment, such as coil or own-tissue embolisation, or surgical treatment, whereas minor injury was defined as requiring no further treatment. Major adverse cardiac events (MACE) were defined as any of the following at the time of admission: death, stroke, Q-wave MI, or emergency target vessel revascularisation. The CK-MB was not measured routinely post procedure, unless symptomatic recurrence or haemodynamic instability developed. The retrograde approach was defined as CTO PCI with an effort to cross the collateral channels with a guidewire so as to reach the distal CTO. The procedural decision was completely at the operator’s discretion. Technical success was defined as an achievement of patent vessels, <30% residual stenosis and a TIMI flow grade 3. All CTOs, once crossed with a guidewire, were treated by DES unless otherwise indicated. The Corsair (Asahi Intecc Co., Ltd) is a microcatheter specifically designed for facilitating collateral channel crossing, retrograde wire control and CTO crossing.
PROCEDURAL TECHNIQUES
All patients were pretreated with aspirin and clopidogrel or ticlopidine, and weight-adjusted heparin was administered to maintain activated clotting time (ACT) for >300 seconds. Double guide catheters (7 Fr or 8 Fr) were introduced both for the CTO and for the donor side of the coronary arteries. Contrast was injected simultaneously to evaluate CTO morphology and to focus on a potential collateral channel reaching the distal CTO. A soft polymer jacket wire over a microcatheter, an OTW balloon or a Corsair was inserted in alternating fashion through the collateral channel to reach the distal CTO segment, where a retrograde CTO crossing was performed with either softer polymer jacket wires or stiffer CTO wires. Some of the cases were treated with direct wire crossing, bilateral wiring (including kissing and knuckle wire techniques), but the wire tended to go into a CTO false lumen in most cases.
The technical details of the CART and reverse CART methods are provided elsewhere14-16. In brief, CART is defined as re-entry of the antegrade wire by retrograde balloon dilation inside the CTO, while reverse CART is defined as re-entry of the retrograde wire by antegrade balloon dilation. When a retrograde wire fails to enter the CTO, other methods are undertaken at the discretion of the operator, including re-application of the antegrade approach.
DATA COLLECTION
The baseline demographics, angiographic characteristics, procedural data and in-hospital events were prospectively collected on a standardised data sheet and retrospectively analysed. Data submission was on a voluntary basis, but data collection was encouraged to reflect all of the consecutive CTO PCI using the retrograde approach. Results were compared between patients who underwent successful retrograde PCI (retrograde success [RS], n=266) and those without successful PCI (retrograde failure [RF], n=112).
STATISTICAL ANALYSIS
Descriptive analyses were used. Discrete variables are presented as counts and percentages, while continuous data are presented as mean±SD. Differences were compared by two-tailed tests, using Student’s t-test and χ2 test or Fisher’s exact test when appropriate. All analyses were performed using StatView 5.0 (Abacus Concepts, Berkeley, CA, USA).
P-values of <0.05 were considered statistically significant and a logistic regression model was applied to identify the factors which contributed to retrograde procedural success.
Results
In total, 378 cases of retrograde CTO PCI were performed in 2009 at the 27 institutions in Japan, including 32.0% (121) previously failed cases. Adoption of the retrograde approach and the success rate varied among the institutions (range: 2-47, 42.6-100%, respectively), as did the volume of CTO PCI cases (Figure 1, range: 25-140). Of these, 284 cases used a primary retrograde approach, while 94 cases were performed immediately after a failed antegrade approach. There was no statistical difference between retrograde and overall CTO PCI success rates among the three different subgroups of institutional retrograde volumes (Figure 1).
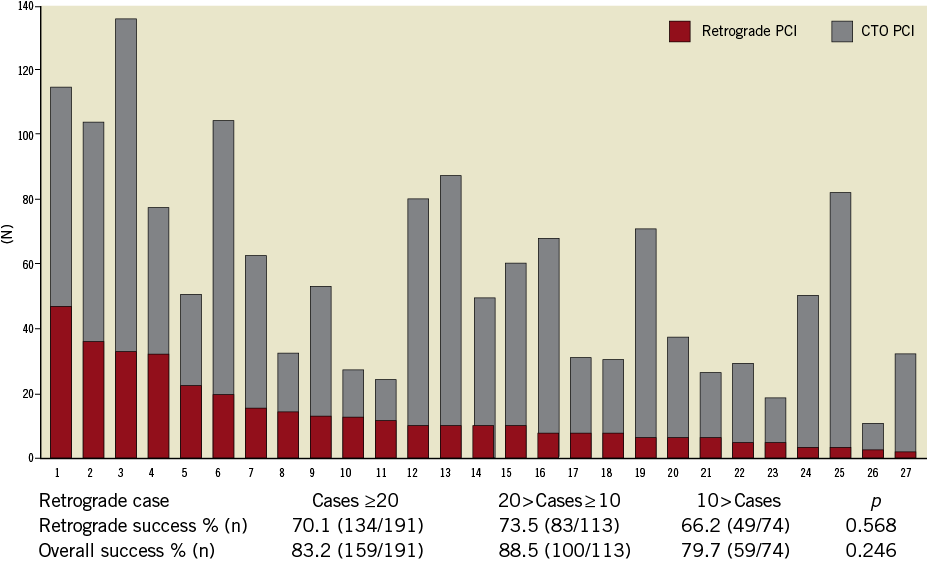
Figure 1. Number of CTO PCI & retrograde procedures per hospital.
SUCCESS RATES
The success rate of each step is shown in Figure 2. The collateral channel was crossed successfully in 81.7% (309), CTO in 91.6% (283) and retrograde in 94.0% (266) of the cases. Re-attempt of the antegrade approach was undertaken in 76.8% (86/112) of cases in RF, with a success rate of 58.1% (50/86). Overall CTO recanalisation was, therefore, achieved in 83.6% (316/378, range: 50-100%, Appendix).
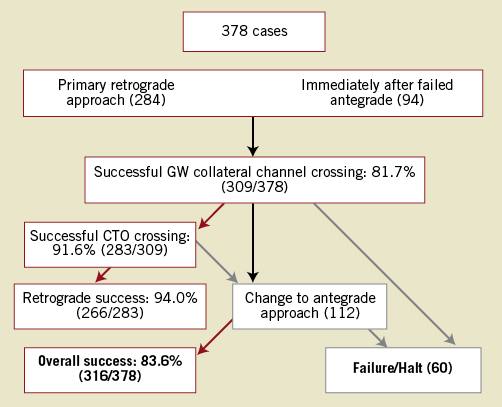
Figure 2. Overall CTO PCI procedural outcome.
BASELINE DEMOGRAPHICS
The baseline characteristics of RS (n=266) and RF (n=112) are shown in Table 1. The mean age of the patients was 65.7 years, and 89.2% were male. Diabetes mellitus (DM) was found in approximately 40% and previous MI in approximately 50%, both of which were similar in the RS and RF groups, respectively. A history of CABG tended to be higher in RF (10.5% vs. 17.9%, p=0.0506), but previous PCI was similar in both.
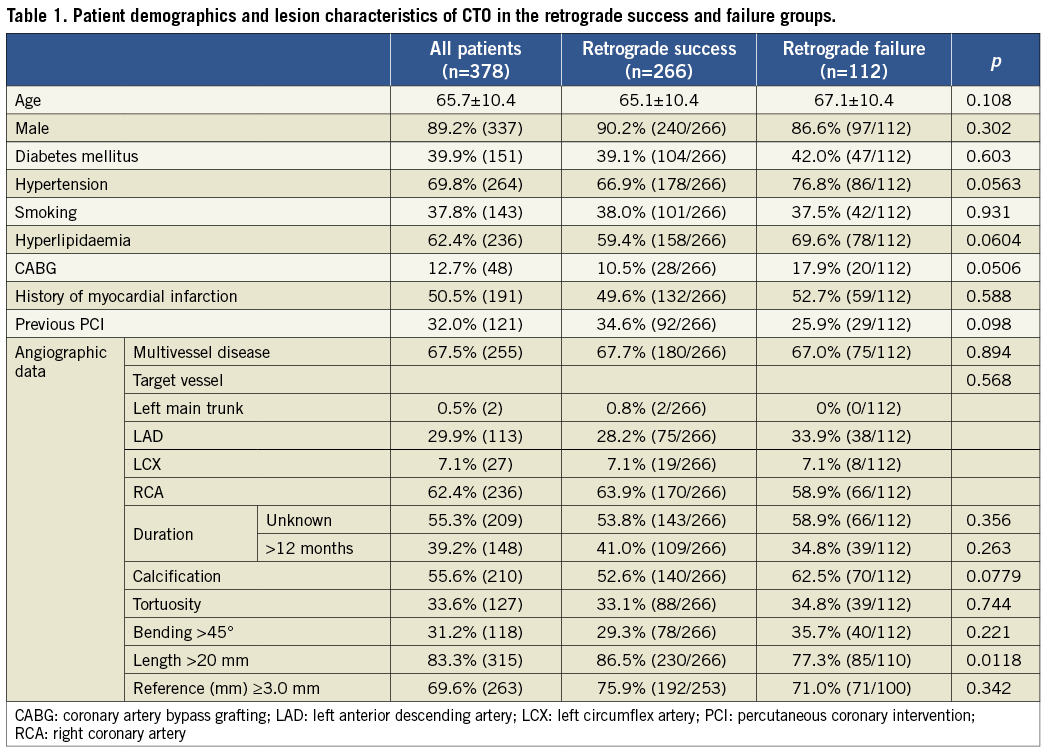
ANGIOGRAPHIC CHARACTERISTICS
The angiographic characteristics of the RS and RF groups are shown in Table 1. More than half had an age-indeterminate occlusion (53.8% vs. 58.9%), and two thirds had multivessel disease (67.7% vs. 67.0%), both groups therefore being similar. The target vessel was predominantly the RCA (63.9% vs. 58.9%), followed by the LAD (28.2% vs. 33.9%), the LCX (7.1% vs. 7.1%) and the LMT (0.8% vs. 0%), respectively. There were no differences in calcification (55.6%), tortuosity (33.6%), bending ≥45° (31.2%) with a reference vessel size ≥3.0 mm (69.6%) in both groups. A significant difference was noted in the CTO length ≥20 mm in the RS group compared with the RF group (86.5% vs.77.3%, p=0.0118).
COLLATERAL CHANNEL CROSSING
The procedural details are shown in Table 2. The most frequently used collateral channel was the septal, followed by epicardial and bypass graft, in 68.9%, 27.2% and 3.9%, respectively. The trend was similar in both. There were significant differences between the RS group and the RF group, with more frequent use of polymer jacket wires (94.0% vs. 83.7%, p=0.0174), Fielder FC wires (Asahi Intecc Co., Ltd) (71.4% vs. 46.5%, p=0.0012), less frequent use of Fielder XT wires (Asahi Intecc Co., Ltd) (22.6% vs. 37.2%, p=0.0384) and more use of the Corsair (42.1% vs. 25.9%, p=0.0029).
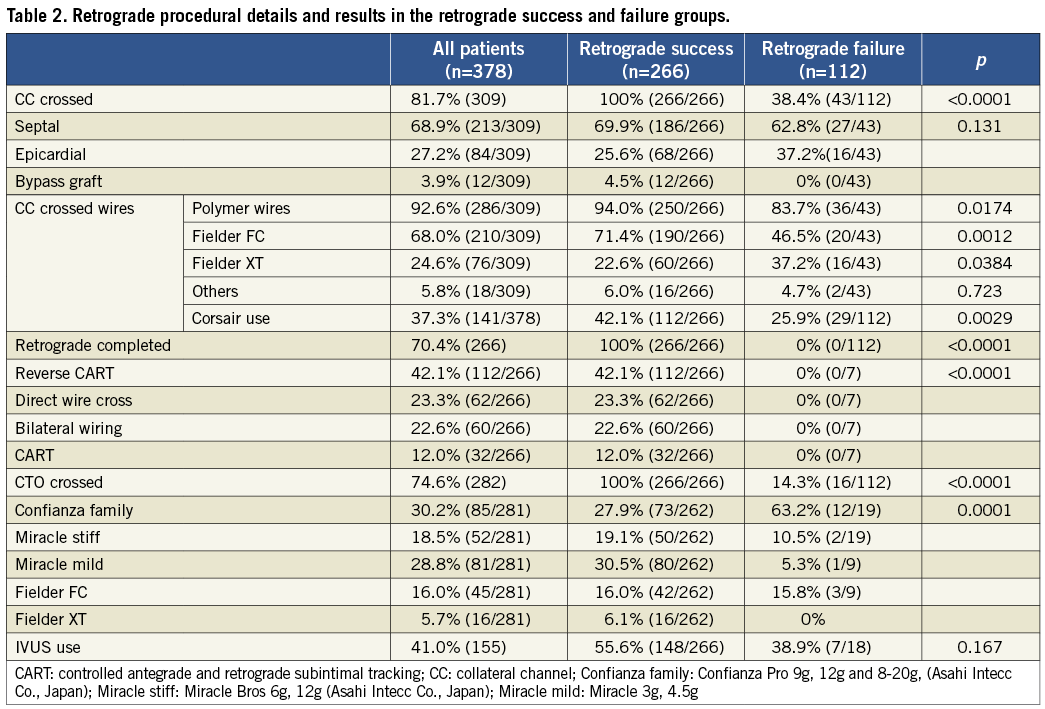
RETROGRADE IMPLEMENTATION IN CTO CROSSING
A variety of retrograde approaches was attempted, as shown in Table 2. The predominant approach was the reverse CART (30.4%), followed by direct wire crossing (16.7%), bilateral wire crossing (16.4%) and CART (8.5%). CTO crossing with a guidewire was achieved in 74.6%. Overall successful retrograde recanalisation was achieved in 70.4% (reverse CART [42.1%], direct wire crossing [23.3%], bilateral wiring [22.6%] and CART [12.0%]). Among the patients in the RF group, an antegrade approach was re-attempted in 76.8% (86), resulting in 58.1% (50) successful recanalisation. A significant difference was noted between the RS and RF groups with regard to the stiffest guidewire crossing the CTO (Table 2). There was a more common use of softer wires (Miracle mild: 30.5%, Fielder FC: 16.0% and Fielder XT: 6.1%; Asahi Intecc Co., Japan) in the RS group, compared with stiffer wires (Confianza Pro: 63.2% and Miracle stiff: 10.5%; Asahi Intecc Co., Japan) in the RF group (p=0.0001). There was a significant reduction in contrast volume and fluoroscopic time in the RS group (299.4±122.3 ml vs. 350.3±164.4 ml, p=0.0014, 94.4±49.1 min vs. 108.4±65.5 min, p=0.0415), but no difference in the whole procedure time (199±80.6 min vs. 211.6±91.4 min, p=0.244).
PROCEDURAL COMPLICATIONS AND IN-HOSPITAL EVENTS (Table 3)
Major collateral channel injury occurred in 0.8% (2) and 2.7% (3) in the RS and RF groups, respectively (p=0.134). All were treated by coil embolisation. There was a significantly higher incidence of minor collateral channel injury in the RF group (17.0% vs. 7.5%, p=0.0058), but these injuries did not require any further treatment.
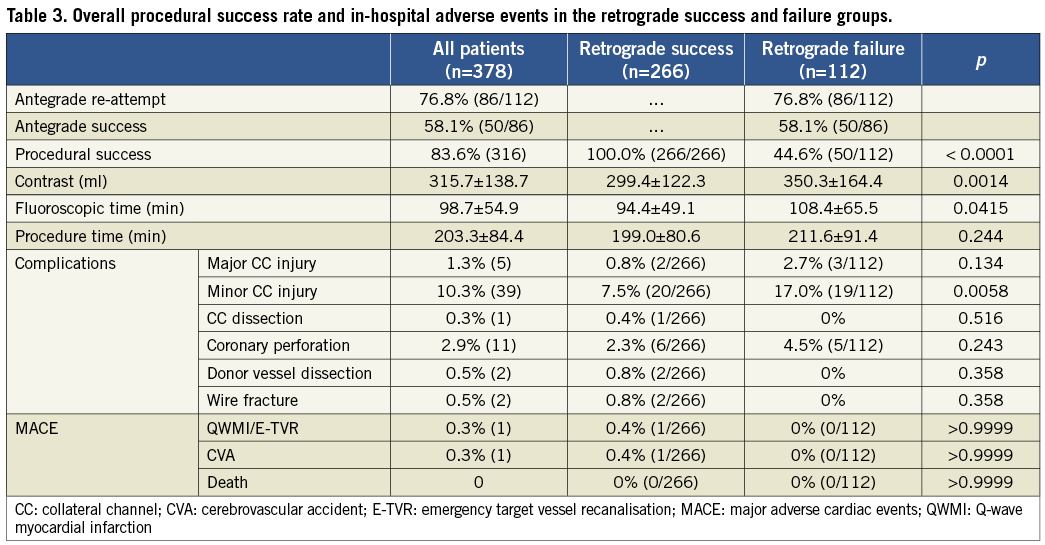
Coronary perforation developed in 2.3% (6) in the RS group, three treated by prolonged balloon inflation, two by covered stents, and one by clot embolisation. Among the 4.5% (5) in the RF group, four were treated by balloon inflation and one by a covered stent (p=0.243). None of them required emergency pericardiocentesis. Collateral channel dissection was noted in 0.4% (1), donor vessel dissection in 0.8% (2) and wire tip fracture in 0.8% (2) in the RS group, without any clinical sequelae.
MACE (Table 3)
MACE did not differ between the groups, with 0.9% (3) in the RS group and 0% in the RF group. Q-wave MI developed in 0.3% (1) in the RS group due to closure of the donor artery, which required emergency PCI. Cerebellar infarction developed in 0.3% (1) in the RS group, which required prolonged admission. There was no mortality in either group.
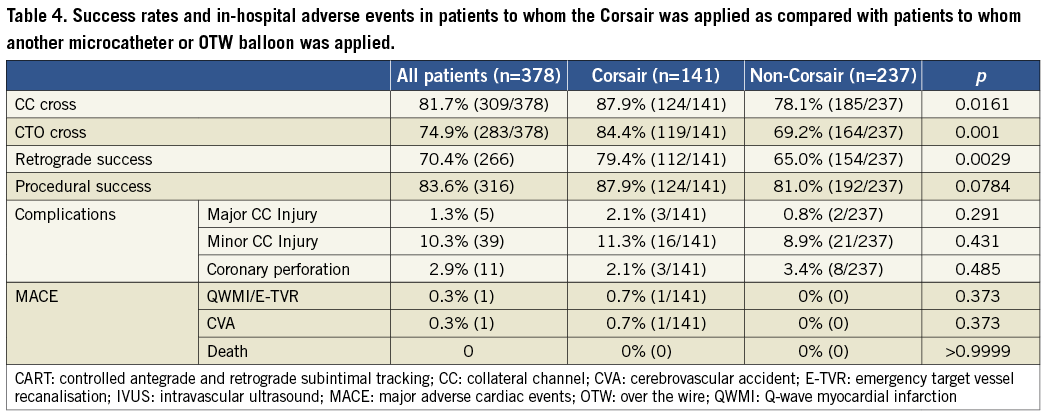
USE OF THE CORSAIR VS. OTHER SYSTEMS (Table 4)
There was higher success with the Corsair in collateral channel crossing (87.9% vs. 78.1%, p=0.0161), CTO crossing (84.4% vs. 69.2%, p=0.001) and retrograde (79.4% vs. 65.0%, p=0.0029), respectively.
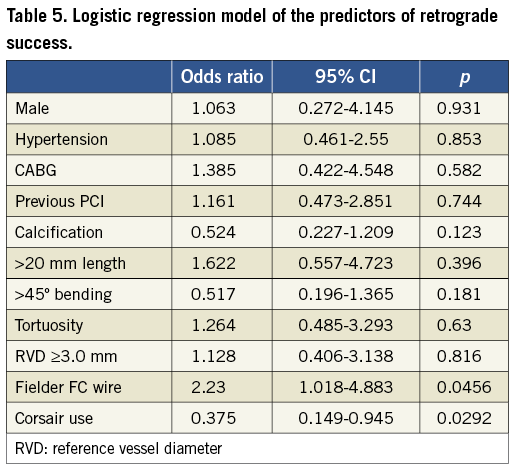
PREDICTORS OF RETROGRADE PROCEDURAL SUCCESS (Table 5)
The results of logistic regression analysis are shown in Table 5. There was no difference between the groups in gender, hypertension, CABG, previous PCI, calcification, >20 mm lesion length, >45° bending, tortuosity, RVD ≥3.0 mm and use of the Fielder FC wire. Corsair use was, however, found to be a significant contributor to successful recanalisation (p=0.0292, CI: 0.149-0.945).
Discussion
This is the largest retrograde CTO PCI series, involving 27 Japanese institutions across the country. A wide application of contemporary retrograde PCI achieved a high rate of recanalisation in complex CTOs with few in-hospital complications in experienced hands. Although use of the Corsair was not randomised, it appears to have been a contributor to retrograde procedural success. Despite the difference of CTO and retrograde volume in each institution, the success rate did not differ significantly in the three separate classes (Figure 1).
PROCEDURAL SUCCESS
In 2008, Sianos et al reported retrograde CTO PCI in 175 cases (24.6% previously failed PCI) from seven European centres, with 80.6% successful collateral channel crossing and 83.4% overall success15. These results are consistent with our findings of collateral channel crossing in 81.7% and overall success in 83.6%. In 2009, Rathore et al reported retrograde CTO PCI in 157 cases (75.2% previously failed PCI) from a CTO centre in Japan, with collateral channel crossing in 73.2%, retrograde success in 65.5% and overall success in 84.7%16. Their predominant methods of retrograde re-entry were CART in 40% and direct wire crossing in 25%.
Kimura et al reported the results of a 224-case CART registry (64.7% previously failed PCI) of two highly experienced CTO operators, and demonstrated collateral channel crossing in 87.7%, retrograde success in 83.5%, and overall success in 90.6%17. Despite differences in retrograde (re) entry, however, multicentre registries with multiple operators tend to have a lower success rate in overall recanalisation, probably due to operator experience, case selections and difference in management when the initial attempt failed. Limited operator performance could have explained the lower than anticipated success rate of antegrade (re) entry (58.1%) in the RF group, once the procedure had developed in an unfavourable direction.
PROCEDURE-ASSOCIATED COMPLICATIONS
In reported retrograde CTO PCI series, MACE was remarkably low at 4.6% (MI: 4.0%, CVA: 0.6%) in Sianos et al15, at 4.5% (MI: 3.8%, emergency CABG: 0.6%) in Rathore et al16, at 1.8% (death: 0.4%, MI: 0.9%, emergency CABG: 0.4%) in Kimura et al17, and at 0.8% in our series (MI: 0.3%, MI and emergency PCI: 0.3%, CVA: 0.3%).
The major collateral injury did not differ (0.8% (2) and 2.7% (3), p=0.134) in the RS and RF groups, respectively, nor did coronary perforation (2.3% (6) and 4.5% (5), p=0.234); however, a significant difference was noted in minor collateral injury (7.5%[20] and 17.0%[19], p=0.0058) in our series, and operator skills might have been associated with the avoidance of serious complications. This is reflected in the fact that none of the patients developed cardiac tamponade.
In terms of CTO crossing wires, the RS group was characterised by a significantly greater use of softer wires, compared to stiffer wires in the RF group, suggesting a potential advantage of retrograde implementation in CTO crossing.
In the Sianos series, 8.6% developed retrograde-related complications, including collateral channel perforation or haematoma in 6.9%, donor artery dissection in 1.1%, and wire entrapment in 0.6%15. In the Rathore series, 15.6% developed retrograde complications, including collateral channel dissection in 10.6%, septal perforation in 3.9% (0.6% (1) required coil embolisation), dissection in 0.6%, and delayed cardiac tamponade in 0.6%, the last of which necessitated pericardial drainage16.
Both groups had very large contrast volume and long fluoroscopic times, with significantly unfavourable profiles in the RF group.
NEWER DEVICES AND TECHNICAL IMPROVEMENTS
Tsuchikane et al reported that application of the newly developed Corsair microcatheter achieved a higher recanalisation rate in 98.8% (n=93), compared with the non-Corsair group (92.5%; n=93) after successful wire crossing through the collateral channel (p=0.030)14. The study reported that the Corsair was also associated with a higher collateral channel crossing in 96.8% and CTO crossing in 84.0%, without increasing major or minor collateral channel injuries, quite consistent with our findings. They applied a retrograde approach, predominantly via reverse CART in 60.9%, retrograde crossing in 20.6% of the Corsair group, whereas CART was used in 64.0% and retrograde wire crossing in 24.4% of the non-Corsair group (p<0.0001). They reported that total fluoroscopic time and the whole procedure time tended to be shorter in the Corsair group (60.1±26.3 vs. 67.8±29.1 min, p=0.087 and 135.6±57.4 vs. 155.5±65.0 min, p=0.078, respectively). This report also found the same trend in favour of the RS group, which suggests a potential refinement of the retrograde approach by using dedicated devices.
In a logistic regression model, use of the Corsair was found to be the only factor associated with successful retrograde recanalisation, thus emphasising the potential benefit of new device technology.
LIMITATIONS
This was a retrospective observational study, which inherently had certain shortcomings. The major disadvantage was the lack of standardised protocol for measuring the post-PCI CPK and detailed analysis of collateral channels, which may have led to the underestimation of the rate of MI and contributor(s) of successful collateral crossing, respectively. Also, use of the Corsair was not randomised. The procedure time was a poor indicator of irradiation dose, since actual calculated doses of radiation could have been recorded in terms of Air Kerma with modern digital equipment. Lack of long-term follow-up beyond hospital admission is another disadvantage, especially in terms of contrast-induced nephropathy and late irradiation injuries. Nonetheless, a wider application of the retrograde approach may change the way we treat CTO, considering the similar high success rate across the globe in dedicated CTO centres in Europe and the US15,18. Further larger prospective studies, based on consecutive patient enrolment with a rigorous protocol, are required to determine the optimal PCI approach in patients with CTO and persistent ischaemia.
Conclusions
Wider application of the retrograde CTO approach provides an excellent chance of successful recanalisation with very few serious complications. However, this requires dedicated devices and advanced technical skills to minimise adverse events. Implementation of the reverse CART method, in conjunction with Corsair, will facilitate the retrograde procedure with less contrast and radiation in properly trained hands.
Acknowledgement
We sincerely appreciate the dedicated CTO pioneering efforts of Drs Osamu Kato, Takahiko Suzuki and the late Hideo Tamai for the development of the modern retrograde approach to CTO PCI.
Appendix
Principal investigators, the enrolled cases in registered institutions, retrograde success (%) and overall procedural success rates (%).
Makoto Muto (47/63.4/80.8), Saitama Cardiovascular and Respiratory Center; Masahisa Yamane (36/86.1/88.9), Sayama Hospital; Etsuo Tsuchikane (33/78.8/90.9), Toyohashi Heart Center; Tetsuo Matsubara (32/68.8/87.5), Nagoya Heart Center; Shigeru Nakamura (23/52.2/73.9), Kyoto Katsura Hospital; Toshiya Muramatsu (20/65.0/70.0), Saiseikai Yokohamashi Tobu Hospital; Akitsugu Oida (16/81.3/94.8), Takase Clinic; Yasumi Igarashi (15/93.3/93.3), Hokkaido Social Insurance Hospital; Mikihiro Kijima (13/100/100), Hoshi General Hospital; Yoichi Nozaki (13/46.2/69.2), Hokko Memorial Hospital; Takahiro Tanaka (12/66.7/88.3), Showa General Hospital; Atsunori Okamura (11/100/100), Sakurabashi Watanabe Hospital; Tsutomu Fujita (11/54.5/100), Sapporo Cardio Vascular Clinic; Ryouhei Yoshikawa (11/63.6/90.9), Sanda Municipal Hospital; Yuji Oikawa (11/45.5/63.6), The Cardiovascular Institute Hospital; Eiji Nozaki (9/55.6/55.6), Iwate Prefectural Central Hospital; Kyo Eisho (9/77.8/100), Kusatsu Heart Center; Yuji Hamazaki (9/77.8/100), Showa University Hospital; Satoru Otsuji (7/85.7/100), Higashi Takarazuka Satoh Hospital; Mitsunori Abe (7/42.9/71.4), Yotsuba Circulation Clinic; Kinzo Ueda (7/42.9/42.9), Rakuwakai Marutamachi Hospital; Masaharu Okada (6/100/100), Shiga Medical Center for Adults; Kenji Wagatsuma (6/50.0/66.7), Toho University Omori Medical Center; Hiroshi Ohira (4/50.0/75.0), Edogawa Hospital; Tomohiro Kawasaki (4/100/100), Shinkoga Hospital; Mutsuo Nakayama (4/50.0/75.0), Hamada Medical Center; Mamoru Nanasato (2/50.0/50.0), Nagoya Daini Red Cross Hospital.
Conflict of interest statement
The authors have no conflicts of interest to declare.
EuroIntervention 2013;9:102-109 published online ahead of print March 2013 DOI: 10.4244/EIJV9I1A15

