Abstract
Aims: The aim of this study was to assess the incidence and impact on midterm outcomes of intimal versus subintimal tracking with both antegrade and retrograde approaches in patients undergoing successful percutaneous coronary intervention for chronic total occlusion (CTO).
Methods and results: In 2012, a total of 1,573 CTO cases from 30 hospitals were enrolled in the Japanese CTO registry. Successful guidewire crossing was performed in 1,411 cases (89.7%). Among them, the guidewire penetration position was clearly identified using intravascular ultrasound (IVUS) imaging in 352 cases, and clinical follow-up at 12 months was performed in 323 cases. These 323 cases were enrolled in this retrospective study: 242 cases were treated with the antegrade approach (antegrade group) and 81 cases were treated with the retrograde approach (retrograde group). The endpoint of this study was target vessel revascularisation (TVR) and major adverse cardiac events (MACE) at 12-month follow-up. Subintimal tracking occurred more frequently in the retrograde group (11.6% vs. 30.9%, p<0.01). TVR was more frequent in the subintimal tracking group in the retrograde group (7.1% vs. 16.0%, p=0.03) but not in the antegrade group (2.8% vs. 3.6%, p=0.99). Although the occlusion length was similar, the subintimal tracking group required a longer stent length compared to the intimal tracking group in the retrograde approach (59.7±24.4 mm vs. 74.0±24.4 mm, p<0.01).
Conclusions: Subintimal tracking was more frequent in the retrograde approach. Intimal tracking should be recommended in the retrograde approach to reduce stent length and to improve follow-up outcomes.
Abbreviations
CART: controlled antegrade retrograde tracking
CTO: chronic total occlusion
CVIC: Cardiovascular Imaging Center
EES: everolimus-eluting stent
IVUS: intravascular ultrasound
MACE: major adverse cardiac events
PCI: percutaneous coronary intervention
TIMI: Thrombolysis In Myocardial Infarction
TSL: total stent length
TVR: target vessel revascularisation
Introduction
Since the introduction of the retrograde approach via native collateral channels and the controlled antegrade retrograde tracking (CART) technique1,2, this technique has been widely adopted and has contributed to an improved success rate of percutaneous coronary intervention (PCI)3-5. Recently, the procedures for the retrograde approach have been refined and have almost been standardised with the development of new dedicated devices6. The reverse CART technique is commonly used with the retrograde approach, but this technique is associated with the possibility of subintimal tracking7,8. Limited information is available regarding the clinical outcomes of subintimal wire tracking. In our previous study (the J-PROCTOR study), there was no apparent negative clinical impact of subintimal tracking at one year after everolimus-eluting stent (EES) implantation with either the antegrade or retrograde approach, although the number of patients enrolled was small (163 patients)9. Therefore, we conducted the present retrospective study to investigate these issues in a larger population (323 patients) by using intravascular ultrasonography (IVUS) to identify intimal and subintimal tracking in patients receiving second-generation drug-eluting stents after successful antegrade or retrograde chronic total occlusion (CTO) intervention.
Methods
STUDY DESIGN
The J-PROCTOR 2 study was a retrospective multicentre study involving 30 hospitals in Japan. From the Japanese CTO registry (Retrograde Summit Registry 2012), cases that satisfied the following three conditions were extracted: (1) the guidewire successfully crossed the occlusion with either an antegrade or retrograde approach, and the position of guidewire penetration (intimal or subintimal tracking) was clearly identified from IVUS images; (2) an EES was deployed to completely cover the occlusion; and (3) clinical follow-up 12 months after the procedure was available.
The definition of a CTO and inclusion criteria have been previously reported7. Exclusion criteria were renal failure (serum creatinine level of 3.0 mg/dL or higher), haemodialysis, saphenous vein graft lesions, and in-stent restenosis. The CTO treatment strategy was selected by operators at their discretion. In each patient, IVUS examination and predilatation were performed followed by EES implantation. The technique used for the retrograde approach has been described previously6,8.
Procedural success was defined as recanalisation of the target lesion with the restoration of grade 3 Thrombolysis In Myocardial Infarction (TIMI) flow and <50% residual stenosis. Antiplatelet therapy, aspirin (100 mg/day) and ticlopidine (200 mg/day) or clopidogrel (75 mg/day), commenced at least three days before PCI, and was continued for at least one year after the procedure. Patients underwent clinical follow-up at 12 months after PCI. The primary endpoint was the target vessel revascularisation (TVR) rate at 12 months after PCI, whereas the secondary endpoint was major adverse cardiac events (MACE) at 12 months. MACE were classified as TVR, Q-wave myocardial infarction (MI), and cardiac death. Non-Q-wave MI was diagnosed when the creatinine kinase-MB level exceeded three times the upper limit of the normal range.
The study protocol was approved by the institutional review board of each participating hospital, and informed consent was obtained from all patients. The safety committee for this study was independently established by a third-party organisation (Itabashi Chuo Hospital, Tokyo, Japan).
ANALYSIS OF ANGIOGRAPHIC AND IVUS IMAGES
The angiographic analysis of baseline angiograms was performed by trained angiographic technicians or physicians at each institution. The analysis of IVUS findings was performed at an independent core laboratory (Cardiovascular Imaging Center [CVIC], Aichi, Japan). Recorded IVUS images were also analysed by an independent expert (Satoru Sumitsuji, MD) who categorised patients into an intimal plaque tracking group or subintimal tracking group (intimal and subintimal groups, respectively). The definitions and IVUS images of intimal plaque tracking and subintimal tracking have been reported previously9.
In patients who underwent TVR, the location and pattern of angiographic restenosis were analysed by the CVIC. The site of restenosis was evaluated in relation to the original occluded site by careful retrospective analysis of the baseline and follow-up angiograms. If TVR was required in patients from the subintimal group, the site of restenosis was evaluated in relation to the subintimal tracking segment by comparing post-procedural IVUS and angiographic images with follow-up angiography findings.
STATISTICAL ANALYSIS
Categorical variables are reported as percentages, and continuous variables are shown as a mean±standard deviation. Either the chi-square test or Fisher’s exact test was used to analyse categorical variables, whereas the unpaired Student’s t-test and Wilcoxon test were used to analyse continuous variables. Logistic regression analysis was performed to identify independent predictors of subintimal tracking by entering baseline patient and lesion characteristics, including qualitative comparative analysis data. All statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC, USA), and p<0.05 was considered to indicate statistical significance.
Results
BASELINE CHARACTERISTICS AND PROCEDURAL OUTCOMES
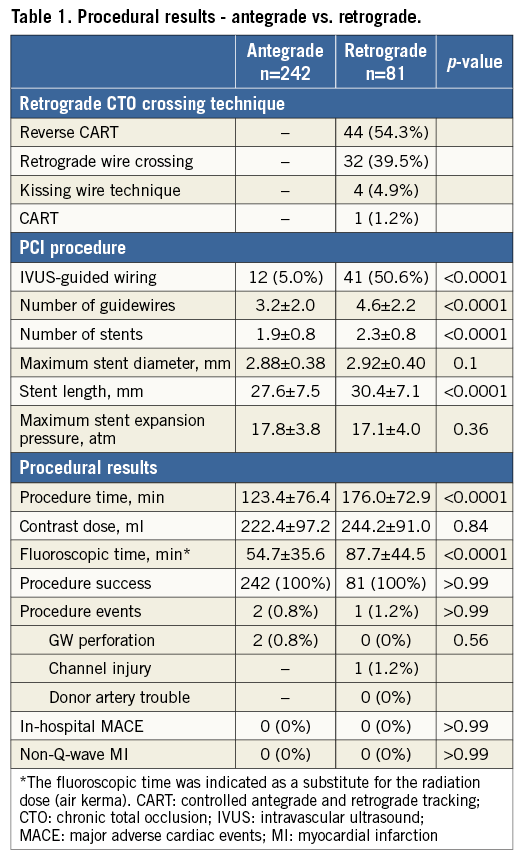
From January 2012 to December 2012, 1,573 cases of CTO from 30 hospitals were enrolled in the Japanese CTO registry (Retrograde Summit Registry 2012). Successful guidewire crossing was obtained in 1,411 cases (89.7%). Among them, the position of guidewire penetration was clearly identified from IVUS images in 352 cases. Clinical follow-up was performed at 12 months in 323 cases. These 323 cases were enrolled in this retrospective study, including 242 patients treated with PCI using an antegrade approach (antegrade group) and 81 patients treated with a retrograde approach (retrograde group). Subintimal tracking occurred more frequently in the retrograde group than in the antegrade group. Compared to those in the antegrade group, patients in the retrograde group had more complicated lesions with calcification and longer occlusion, and they were more likely to undergo repeat PCI. Table 1 summarises the procedural data for both approaches. A reverse CART technique was used in 54.3% of patients in the retrograde group. A larger number of guidewires and stents was necessary in the retrograde group, and the total stent length was also longer in the retrograde patients. Procedural success was achieved in all patients treated by both approaches, and there were no differences in procedural events or in-hospital MACE.
COMPARISON OF GROUPS CATEGORISED BY IVUS (INTIMAL VS. SUBINTIMAL)
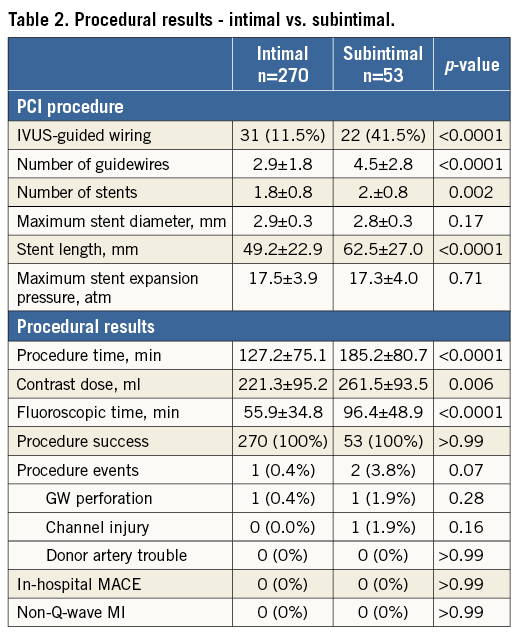
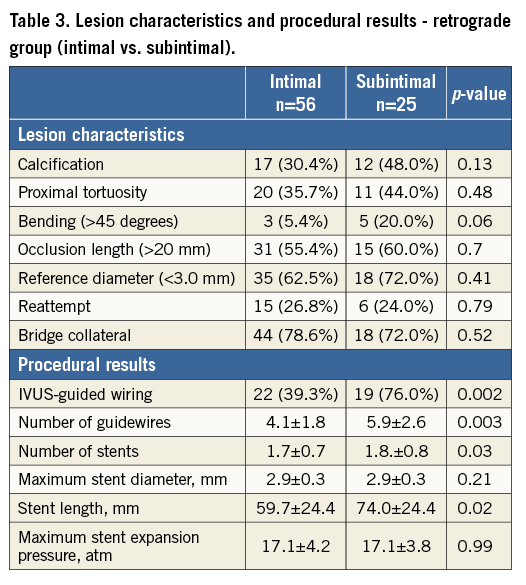
A total of 323 cases were categorised into the intimal tracking group (270 cases) and the subintimal tracking group (53 cases) according to IVUS classification. The intimal tracking group comprised 214 antegrade and 56 retrograde cases. On the other hand, the subintimal tracking group consisted of 28 antegrade cases and 25 retrograde cases. Compared to those in the intimal group, patients in the subintimal group had more complicated lesions with calcification, bending, and a smaller reference diameter, and they were more likely to undergo repeat PCI. Table 2 compares the procedural outcomes between these two groups. IVUS-guided wiring was necessary more often in patients in the subintimal group than in the intimal group. The number of guidewires and stents needed for the procedure was significantly larger in the subintimal group than in the intimal group. The total stent length was much longer in the subintimal group than in the intimal group. The procedure time was longer in the subintimal group; additionally, much more contrast media and a longer fluoroscopic time were required in the subintimal group than in the intimal group. The frequency of procedural events such as wire perforation, donor artery trouble, and channel injury was very low in both groups. Procedural success was achieved in all patients in both groups, and there were no differences in procedural events or in-hospital MACE.
COMPARISON OF GROUPS CATEGORISED BY IVUS (INTIMAL VS. SUBINTIMAL IN THE RETROGRADE GROUP)
Among the 81 retrograde cases, intimal tracking was performed in 56 cases and subintimal tracking was performed in 25 cases. Table 3 shows results of the comparison between these groups. Although the occlusion length was similar between the groups, the subintimal group required a longer stent length compared to the intimal group when using the retrograde approach.
TWELVE-MONTH FOLLOW-UP RESULTS
Twelve-month follow-up data were acquired in all patients. The rate of MACE was higher in the retrograde patients due to the high rate of TVR (Table 4A). A comparison of the 12-month follow-up results between the intimal and subintimal groups is shown in Table 4B. The rates of MACE and TVR tended to be higher in the subintimal group than in the intimal group. Subintimal tracking resulted in increased TVR in the retrograde group, but not in the antegrade group (Figure 1). The site and pattern of restenosis in patients who underwent TVR was examined. Although TVR was performed in five of 53 patients (9.4%) in the subintimal group (four cases of focal restenosis and one case of diffuse restenosis), occlusion-related restenosis only occurred in one patient. In this case, the restenosis site appeared to be located in the subintimal tracking segment after comparing post-procedural IVUS and angiographic images with follow-up angiography findings.
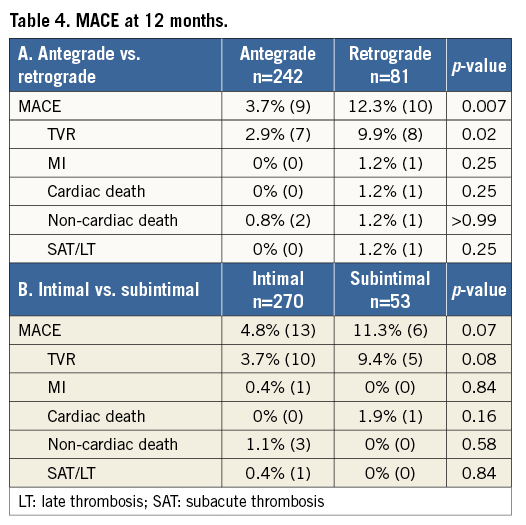
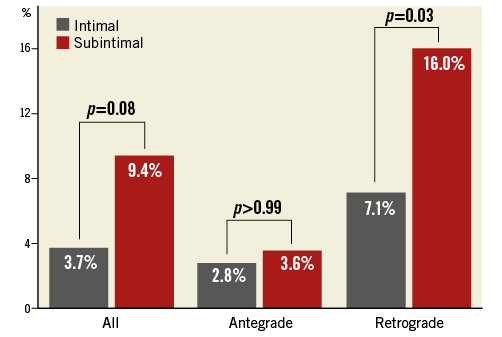
Figure 1. TVR at 12 months. All (intimal vs. subintimal). Antegrade (intimal vs. subintimal). Retrograde (intimal vs. subintimal).
RESULTS OF MULTIVARIATE ANALYSIS
Independent predictors of subintimal wire tracking in the antegrade group are indicated in Figure 2A. CTO lesions with a small reference diameter (<3.0 mm) and proximal tortuosity were prone to subintimal tracking in the antegrade group. Cases in which the CTO intervention was reattempted were also prone to subintimal tracking. However, bending more than 45 degrees was an independent predictor of subintimal wire tracking in the retrograde group (Figure 2B).
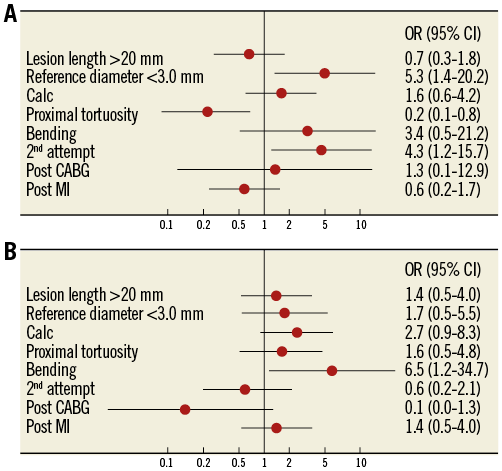
Figure 2. Independent predictors of subintimal tracking. A) Antegrade group. B) Retrograde group.
Discussion
The main findings of this study can be summarised as follows. 1) Among patients undergoing successful CTO intervention, subintimal wire tracking more frequently occurred with the retrograde approach than with the antegrade approach. 2) Bending in the occlusion was an independent predictor of subintimal wire tracking in the retrograde group. Although the occlusion length was similar, the subintimal group required a longer stent length compared to the intimal group in the retrograde approach. 3) With the retrograde approach, TVR was more frequently required in the subintimal tracking group. 4) The restenosis site did not necessarily correspond with the subintimal tracking segment.
Limited information has been reported regarding the frequency of subintimal tracking during CTO interventions9-11. According to previous reports, the frequency of subintimal tracking ranges from 8.7% to 45.5% with the antegrade approach, and from 24.2% to 50.0% with the retrograde approach. In each report, the frequency was higher for the retrograde approach than for the antegrade approach. The tendency previously reported was similar to that found in our present study, although the treatment strategy and number of subjects were different (230 cases in three previous studies vs. 323 cases in the present study). Although intentional subintimal tracking and re-entry techniques12,13 were not used in our study population, the frequency of subintimal tracking was not low when using the antegrade approach.
Next, we review the process in which subintimal wire tracking occurs in CTO interventions. Regarding the antegrade approach, intimal tracking in the occluded site is a key to successful wire re-entry. Unlike open vessel interventions, an accurate course of the vessel cannot be visualised during CTO interventions. Therefore, we advanced the guidewire through the occlusion by imagining the proper vessel course, often assisted by contralateral injection or the identification of calcium around the vessel by fluoroscopy. If we faced difficulty in identifying the proper vessel course or performing accurate wire manipulation, the guidewire was easily placed into the subintimal space. Once the antegrade guidewire appeared to be in the subintimal space, the parallel wire technique or IVUS-guided wire manipulation was used to correct the wire course and, if this failed, penetration into the distal target from the subintimal space or conversion to the retrograde approach was attempted. Therefore, during antegrade CTO intervention, operators should tolerate the fact that the subintimal space sometimes extends beyond the distal end of the occlusion.
In the present study, proximal tortuosity was an independent predictor of subintimal wire tracking in the antegrade approach, because it impeded wire manipulation. In the retry cases, wire manipulation was also difficult due to the previously created subintimal space.
Regarding the retrograde approach, subintimal tracking differed depending on the type of procedure, such as the reverse CART, kissing wire, retrograde wire cross, or CART technique. If the kissing wire or retrograde wire cross technique was used to recanalise the occlusion, the morphosis of the subintimal space was similar to the antegrade wiring. However, during the reverse CART technique, the connection between the antegrade and retrograde guidewires created in the subintimal layer rather than in the intraplaque often led to subintimal wire tracking. Theoretically, the site of subintimal wire tracking was limited within the CTO segment and this fact justifies the complexity of the retrograde procedure. In the present registry, more than half of the cases in the retrograde group were treated with the reverse CART technique. Bending more than 45 degrees was an independent predictor of subintimal wire tracking in the retrograde group, mainly because an intraplaque connection was difficult to create with the reverse CART technique in such cases.
Limited information has also been reported about the prognosis of subintimal wire tracking. In our previous study, there was no apparent negative clinical impact of subintimal wire tracking one year after EES implantation with either the antegrade or retrograde approach9. However, in the present study, TVR was more frequently required in the subintimal group than in the intimal group using the retrograde approach. This difference may be caused by the fact that the rate of subintimal wire tracking in the retrograde group was higher in this study than that in the previous study. Considering the follow-up result that the TVR sites were not necessarily related to the subintimal tracking segment, we think the main reason for the negative clinical impact was not the subintimal wire tracking itself but the longer stent requirement. Recently, the impact of total stent length (TSL) after EES implantation on long-term clinical outcomes has been reported14. Hiromasa et al determined that the cumulative three-year target lesion revascularisation was significantly higher in the long TSL group (>28 mm) than in the short TSL group (<28 mm) (14.6% vs. 6.4%, p<0.01). In our study, the TSL of the retro-subintimal group was 74.0±24.4 mm. Taking these findings together, the higher TVR rate in the retro-subintimal group was caused by the longer EES implantation, with no direct relationship to subintimal wire tracking. Therefore, proper wire manipulation with available technologies must be utilised to minimise subintimal tracking and required stent length.
Limitations
The limitations of this study were as follows. 1) This study was a retrospective, observational study, not a randomised study. 2) Most procedures were performed by skilled and experienced interventional cardiologists. Thus, the results may have been different if less experienced operators had been involved. 3) Qualitative comparative analysis was not performed at an independent core laboratory. 4) The angiographic follow-up rate was relatively low (36.8%). Therefore, there was a possibility that silent restenosis or re-occlusion was overlooked. 5) The number of enrolled patients was relatively small. 6) The clinical follow-up period of one year may have been insufficient.
Conclusions
Although the occlusion length was similar between groups, the subintimal group required a longer stent length than the intimal group using the retrograde approach. Subintimal tracking resulted in increased TVR in the retrograde group, not in the antegrade group. The restenosis site did not necessarily correspond with the subintimal tracking segment. Further evaluation is required to confirm these findings and to assess the safety of various types of CTO intervention.
| Impact on daily practice In the present study, in the subintimal tracking group TVR was more frequent in the retrograde group than in the antegrade group. The restenosis site did not necessarily correspond with the subintimal tracking segment. Although the creation of a subintimal space is sometimes inevitable during antegrade and retrograde CTO intervention, proper wiring techniques with available technologies and dedicated devices must be utilised to minimise subintimal tracking for the purpose of reducing stent length and improving follow-up outcomes. |
Acknowledgements
The authors would like to thank S. Sumitsuji, Osaka University, for his assistance and important contributions.
Conflict of interest statement
E. Tsuchikane is a consultant for Asahi Intecc, Abbott Vascular, and Boston Scientific. T. Fujita is a consultant for Terumo Corp. The other authors have no conflicts of interest to declare.