Abstract
Aims: This study sought to demonstrate the incidence, predictors, and management of microcatheter collateral channel (CC) tracking failure in retrograde percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) lesions.
Methods and results: Prospectively collected data from 371 consecutive retrograde CTO-PCI procedures between March 2015 and January 2018 were retrospectively analysed. The incidence of initial microcatheter CC tracking failure was 22.5% in 280 procedures with wire CC tracking success. For septal collaterals, CC grade 0-1 collaterals (odds ratio [OR]: 8.3; p<0.001), channel entry angle <90° (OR: 13.0; p=0.001), channel exit angle <90° (OR: 44.3; p=0.004), and Finecross MG as initial microcatheter (OR: 2.7; p=0.032) were independently related to initial microcatheter CC tracking failure. Meanwhile, the only predictor for epicardial collaterals was CC 1 collaterals (OR: 26.9; p<0.001). Frequently applied solutions included microcatheter switching (61.9%), and microcatheter switching combined with GUIDEZILLA (14.3%) or anchoring balloon technique (6.3%).
Conclusions: Initial microcatheter CC tracking failure was found in nearly one quarter of procedures after wire CC tracking success. Independent angiographic predictors of initial microcatheter CC tracking failure included CC 0-1 collaterals, channel entry angle <90°, and channel exit angle <90° for septal collaterals, and CC 1 collaterals for epicardial collaterals.
Introduction
Chronic total occlusion (CTO) lesions have been observed in as many as 16~18% of patients with coronary artery disease (CAD) referred for a coronary angiogram1,2. Previous studies have demonstrated that successful percutaneous coronary intervention (PCI) for CTO yields beneficial effects including symptom relief, improving quality of life, and improving left ventricular function3,4,5,6. However, even with emerging new techniques and novel devices, percutaneous treatment of CTO lesions remains a major challenge7.
Over the last decade, the retrograde approach has improved the success rate of CTO-PCI remarkably8,9,10,11. Selection of a suitable collateral channel (CC) for both wire and microcatheter tracking is vital for retrograde intervention. Nevertheless, even after wire CC tracking success, retrograde microcatheter CC tracking remains a challenge in some cases. To the best of our knowledge, data on microcatheter CC tracking in retrograde CTO-PCI are very limited. Moreover, the management and procedural outcome of microcatheter CC tracking failure have not been well elucidated.
In the present study, we evaluated the incidence, predictors, and management of microcatheter CC tracking failure in retrograde CTO-PCI.
Methods
STUDY POPULATION
Prospectively collected data for patients who underwent retrograde CTO-PCI performed at the Shanghai Institute of Cardiovascular Diseases, Zhongshan Hospital, Shanghai, were retrospectively analysed. Between March 2015 and January 2018, 371 consecutive retrograde CTO-PCI cases were screened from the database of the Chronic Total Occlusion Club, China (CTOCC). No attempted retrograde case was excluded. According to current clinical practice, only when patients displayed symptoms of ischaemia or when ischaemia was confirmed by non-invasive assessments related to occlusive coronary arteries was recanalisation therapy performed12,13. A total of four high-volume operators (>100 total CTO-PCI cases per year) and seven non-high-volume operators participated in the present study. Baseline characteristics, angiographic characteristics, procedural parameters, and in-hospital events were collected via electronic case report forms. The study complied with the Declaration of Helsinki. All patients provided informed consent for both the procedure and subsequent data collection and analysis for research purposes. The research protocol was approved by the ethics committee of Zhongshan Hospital.
DEFINITIONS
CTO was defined as Thrombolysis In Myocardial Infarction (TIMI) grade 0 flow and the duration of coronary occlusion ≥3 months7,14,15. The J-CTO score was calculated according to the study reported by Morino et al16. CC grade was defined according to the report by Werner et al17. Tortuosity, as defined by McEntegart et al18 and CC score, as defined by Huang et al19 were adopted in the present study. Adverse channel entry and exit angles were defined using a cut-off angle <90°18. Morphological assessments of first attempted collaterals were recorded for retrograde wire tracking failure procedures. All of the angiograms were reviewed by at least two qualified interventional cardiologists. If there were any ambiguities in the evaluation of angiograms, the angiograms were then subjected to independent review by a third qualified interventional cardiologist.
Retrograde wire CC tracking success was defined as the retrograde wire crossing the collateral to reach the distal cap of the CTO segment19. Procedural success was defined as a restoration of TIMI flow grade 3 in the target vessel and a residual stenosis <30% by visual estimation. Clinical success was defined as achievement of procedural success without in-hospital major adverse cardiac and cerebrovascular events (MACCE), which included death from all causes, Q-wave myocardial infarction (MI), stent thrombosis20, ischaemia-driven revascularisation, and stroke. Procedural complications were defined as donor vessel dissection, vessel perforation21, cardiac tamponade, cardiac tamponade requiring pericardiocentesis, emergent PCI, and emergent coronary artery bypass grafting (CABG).
INTERVENTIONAL PROCEDURES
All patients without a contraindication received dual antiplatelet therapy (aspirin and clopidogrel/ticagrelor). Heparin was introduced intravenously to achieve an activated clotting time of 300 to 350 seconds during the procedure. Selection of vascular access site was at the operator’s discretion, and bilateral coronary injections were performed to evaluate CTO lesion morphology. The retrograde approach was used as the primary approach or after failure of the antegrade approach. The retrograde approach was initiated by manipulating a floppy wire into a CC supported by a 150 cm microcatheter22, such as the Corsair™ (Asahi Intecc, Aichi, Japan), Finecross® MG (Terumo Corp., Tokyo, Japan) or other microcatheters. The wires used for CC tracking included SION® (Asahi Intecc), SION® black (Asahi Intecc), SION® blue (Asahi Intecc), SUOH 03 (Asahi Intecc), Fielder™ XT-R (Asahi Intecc), Fielder™ FC (Asahi Intecc), and Runthrough® NS (Terumo Corp.). After wire CC tracking success, microcatheter advancement through the CC was attempted. Utilisation of the retrograde wire technique depended on the patient’s coronary anatomy and general condition during the procedure. Generally, retrograde wire crossing and the kissing wire technique were preferred for short lesions, and the reverse controlled antegrade or retrograde subintimal tracking (CART) technique9,23 for longer lesions. After recanalisation, drug-eluting stents were implanted to achieve procedural success.
STATISTICAL ANALYSIS
The data are expressed as the mean±SD for the continuous variables and as frequencies for the categorical variables. The comparison of continuous variables was performed by the independent Student’s t-test or the Mann-Whitney U test, as appropriate. Statistical analysis of the categorical variables was performed using Pearson’s chi-square or Fisher’s exact test (when at least 25% of values showed expected cell frequencies <5), as appropriate. Stepwise logistic regression analysis was conducted to identify the angiographic and procedural predictors. Univariate analysis was initially performed and univariate variables with p-values <0.05 were thereafter included in the multivariate model. P-values were two-tailed, and p<0.05 was considered statistically significant. The data were analysed using statistical software SPSS, Version 20.0 (IBM Corp., Armonk, NY, USA).
Results
BASELINE CHARACTERISTICS AND CLINICAL OUTCOMES
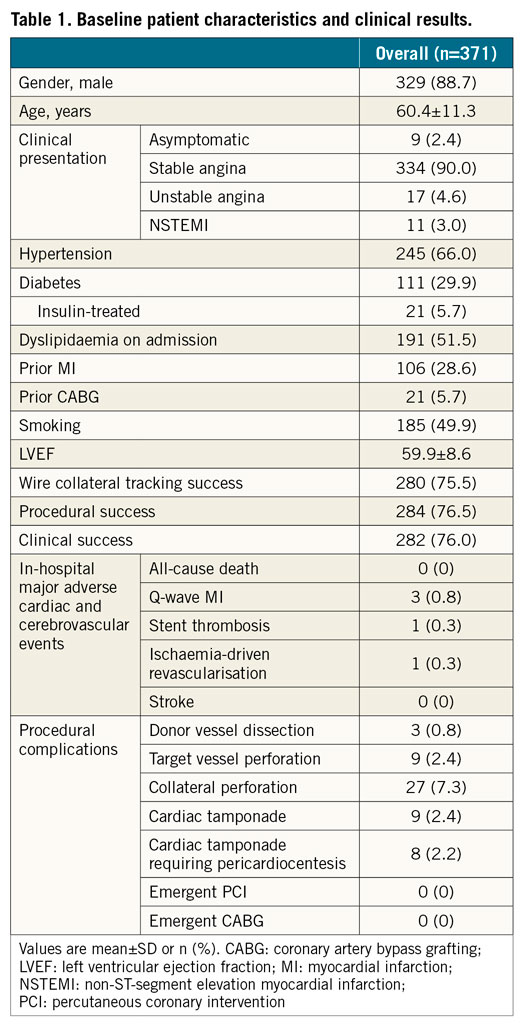
The baseline clinical characteristics are summarised in Table 1. In the present study, a procedural success rate of 76.5% (284/371) and a clinical success rate of 76.0% (282/371) were achieved. No deaths were observed. Three occurrences of Q-wave MI were adjudicated, two of which were related to the occlusion of diagonal branches proximal to left anterior descending artery CTOs; the third was due to stent implantation in the false lumen followed by subacute stent thrombosis. One patient was recommended for bypass surgery four days after the index procedure of a failed right coronary artery CTO-PCI. In terms of complications, the occurrence of donor vessel dissection and target vessel perforation was 0.8% (3/371) and 2.4% (9/371), respectively. Collateral perforations, consisting of 11 septal and 16 epicardial collateral perforations, occurred in 7.3% of all cases. A total of nine (2.4%) cases exhibited pericardial tamponade, and pericardiocentesis was performed in eight (2.2%) cases. One patient, in whom delayed pericardial tamponade was found, was only given conservative treatment due to gradually decreased pericardial effusion.
EVALUATION OF RETROGRADE WIRE CC TRACKING
The overall success rate of wire CC tracking was 75.5% (280/371). A detailed analysis of the retrograde wire CC tracking is shown in Supplementary Appendix 1 and Supplementary Table 1.
EVALUATION OF RETROGRADE MICROCATHETER CC TRACKING
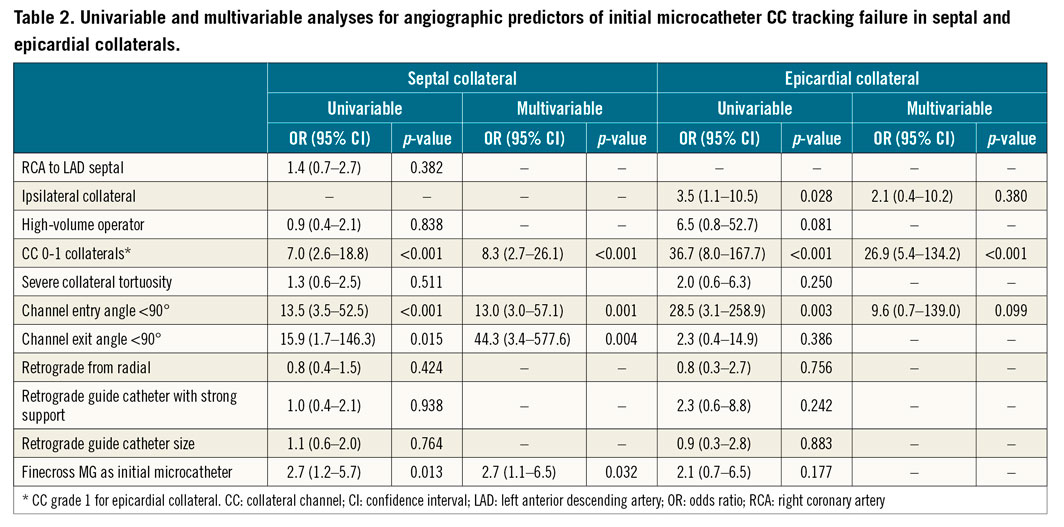
Among 280 procedures with wire CC tracking success, initial microcatheter collateral tracking failure occurred in 63 (22.5%) procedures. Stepwise logistic regression analysis was performed to identify angiographic factors for predicting initial microcatheter CC tracking failure (Table 2). A detailed incidence of serial variables is shown in Supplementary Table 2. For septal collaterals (n=199), CC 0-1 collaterals (odds ratio [OR]: 8.3, 95% confidence interval [CI]: 2.7-26.1, p<0.001), channel entry angle <90° (OR: 13.0, 95% CI: 3.0-57.1, p=0.001), channel exit angle <90° (OR: 44.3, 95% CI: 3.4-577.6, p=0.004), and Finecross MG as initial microcatheter (OR: 2.7, 95% CI: 1.1-6.5, p=0.032) were independently related to initial microcatheter CC tracking failure. Meanwhile, the only independent predictor for epicardial collaterals was CC 1 collaterals (OR: 26.9, 95% CI: 5.4-134.2, p<0.001) (n=76). After wire CC tracking success, several retrograde wire techniques were deployed - retrograde wire crossing (35.4%), kissing wire (15.4%), and reverse CART technique (41.1%).
In 63 initial microcatheter CC tracking failures, 51 procedures achieved final microcatheter CC tracking success after subsequent attempts; five procedures switched to kissing wire technique, and seven procedures failed to advance the microcatheter through collaterals after various attempts. Overall, the final success rate of microcatheter CC tracking achieved was 95.7% (268/280) after management. The detailed management of final microcatheter CC tracking success is illustrated in Figure 1 and Supplementary Table 3. Frequently applied solutions included simple microcatheter switching (61.9%, 39/63), and microcatheter switching combined with GUIDEZILLA™ (Boston Scientific, Marlborough, MA, USA) (14.3%, 9/63), anchoring balloon technique (6.3%, 4/63), or septal collateral dilation (3.2%, 2/63). Other measures included independent application of GUIDEZILLA support (4.8%, 3/63) or anchoring balloon technique (1.6%, 1/63). A detailed distribution of initial microcatheter selection in different collaterals is shown in Figure 2. In all 54 microcatheter switching attempts, 28 switched from Corsair to other microcatheters and 26 switched from Finecross MG to other microcatheters (Figure 1, Supplementary Table 3). No complications were related to microcatheter switching and the other measures mentioned above.
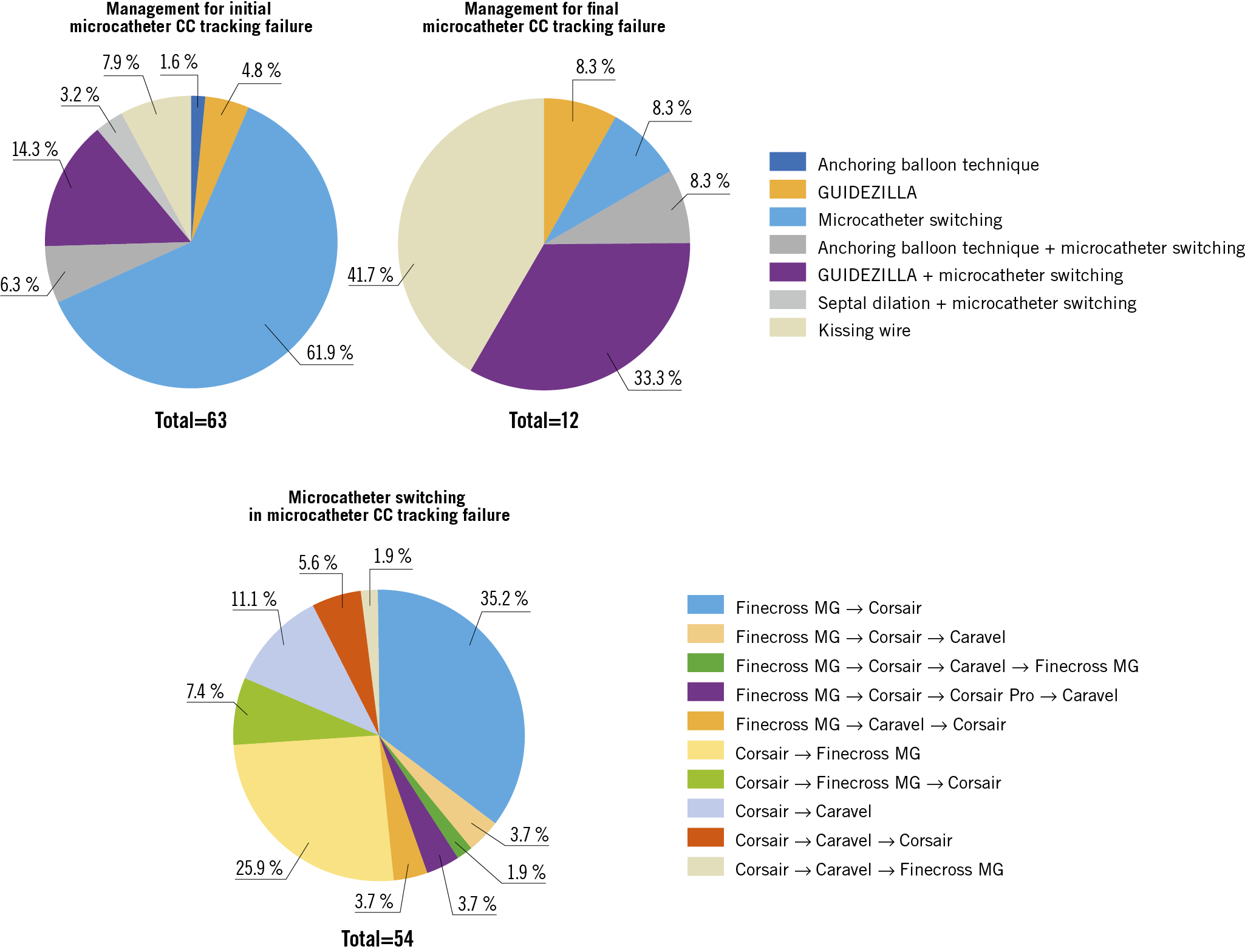
Figure 1. Detailed management of microcatheter CC tracking failure. CC: collateral channel
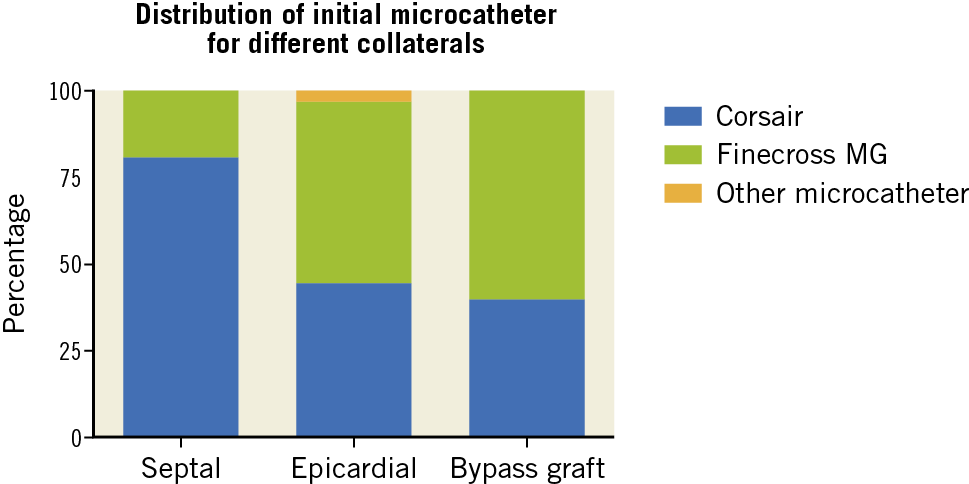
Figure 2. Distribution of the initial microcatheter for different collaterals in 280 procedures with wire CC tracking success. CC: collateral channel
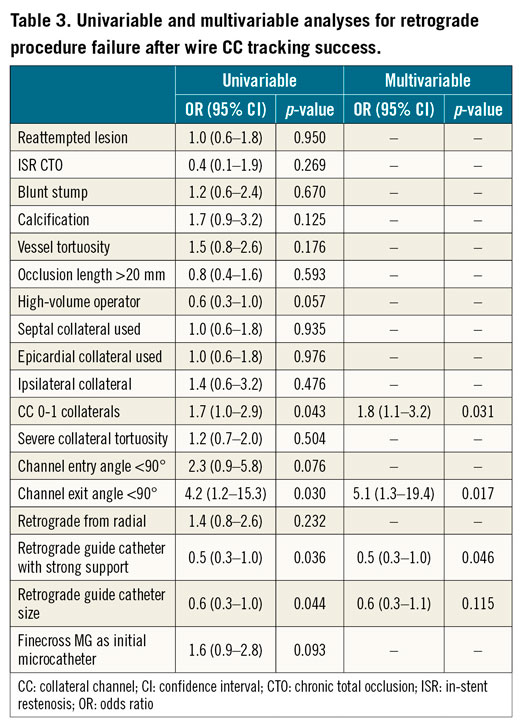
LOGISTIC REGRESSION ANALYSIS TO IDENTIFY POSSIBLE PREDICTORS OF RETROGRADE PROCEDURE FAILURE
Table 3 presents the stepwise logistic regression analysis performed to identify angiographic factors for predicting retrograde procedure failure after wire CC tracking success (n=280). In univariate analysis, CC 0-1 collaterals, channel exit angle <90°, retrograde guide catheter with strong support, and retrograde guide catheter size were related to the retrograde procedure outcome. A multivariate model showed that CC 0-1 collaterals (OR: 1.8, 95% CI: 1.1-3.2, p=0.031) and channel exit angle <90° (OR: 5.1, 95% CI: 1.3-19.4, p=0.017) were associated with retrograde procedure failure. Meanwhile, a retrograde guide catheter with strong support (OR: 0.5, 95% CI: 0.3-1.0, p=0.046) was revealed to be a negative predictor of retrograde procedure failure.
Discussion
The main findings of the present study can be summarised as follows: 1) initial microcatheter CC tracking failure was found in 22.5% of cases after wire CC tracking success; 2) for septal collaterals, initial microcatheter CC tracking failure was independently related to CC 0-1 collaterals, channel entry angle <90°, channel exit angle <90°, and Finecross MG as the initial microcatheter; 3) the only independent predictor of epicardial collaterals was CC 1 collaterals; and 4) microcatheter switching combined with support enhancement was an effective measure in managing the microcatheter CC tracking failure.
PREDICTORS OF INITIAL MICROCATHETER CC TRACKING FAILURE
Initial microcatheter CC tracking failure after wire CC tracking success may be related to: 1) the anatomical characteristics of the CC, especially entry and exit angle, CC grade, tortuosity, etc.; 2) weak back-up support supplied by the guide catheter; and 3) different microcatheter features. In the present study, we identified different predictors of microcatheter tracking for septal and epicardial collaterals. A previous study showed that CC grade 0-1 and severe tortuosity were related to wire CC tracking failure19. However, due to the different anatomical features of septal and epicardial collaterals, we usually adopted the following principles for CC selection in our daily practice: for septal collaterals, the straighter the better; for epicardial collaterals, the bigger the better. As a result, we often chose a less tortuous septal channel irrespective of its CC grade and a larger size epicardial channel irrespective of its tortuosity. This may, at least partially, explain why different predictors were identified between septal and epicardial collaterals. An intriguing finding in the present study was the irrelevance of collateral tortuosity to initial microcatheter CC tracking failure (Table 2). A reasonable explanation may be that successful wire CC tracking arguably provided support to straighten the CC and decrease tortuosity. The channel entry and exit angles of epicardial collaterals were not related to microcatheter CC tracking failure in the present study. Due to the limited sample size in the epicardial group (n=76), a future study with a large sample size is needed. It should be pointed out that an evaluation of channel entry and exit angle18 should also be undertaken before microcatheter CC tracking. Advancing a microcatheter through an adverse channel entry or exit angle would be a challenge and should be avoided during collateral selection.
In the present study, the Finecross MG microcatheter was shown to be associated with initial microcatheter septal tracking failure. This finding was potentially related to different designs among microcatheters. Figure 2 shows the detailed distribution of initial microcatheter selection in different collaterals. The major reasons for choosing the Finecross MG as the initial microcatheter in our centre included: 1) the 150 cm Corsair microcatheter was sometimes not available; and 2) the lower cost of the Finecross MG compared to the Corsair. At the same time, it is important to point out that microcatheter selection was influenced by operator consideration of the anatomical complexity of collaterals.
MANAGEMENT OF MICROCATHETER CC TRACKING FAILURE
To solve microcatheter CC tracking failure, the measure most frequently applied in the present study was microcatheter switching. It is very important to point out that microcatheter switching from Corsair to Finecross MG, and vice versa, should be considered. Interestingly, microcatheter switching back to the original failed microcatheter may achieve final CC tracking success in select cases. One probable explanation could be the additive dilating effects of all microcatheter switching attempts prior to the final CC tracking success.
Regarding the back-up support of guide catheters, several items including retrograde access, retrograde guide catheter type and catheter size were analysed. The results did not show significant differences among these characteristics. However, we should exercise great caution in coming to this conclusion. In our daily practice, we found microcatheter CC tracking failure paired with weaker back-up guide catheters in some cases. Since guide catheter switching was always the second choice just after wire CC tracking success, selecting a retrograde guide catheter with extra back-up support played a pivotal role in the whole procedure. Simple and effective measures to increase guide catheter support present in the current study included the deployment of guide catheter extensions, such as GUIDEZILLA, and anchoring balloon technique. Another alternative was septal channel dilation using a small balloon at a low atm pressure. In the present study, septal channel dilation was performed in two procedures. One case used a small balloon and the other the THREADER™ micro-dilatation catheter (Boston Scientific). As a result, after management, the final success rate of microcatheter CC tracking achieved was 95.7%. The suggested management for microcatheter CC tracking failure is illustrated in Figure 3. It is very important to point out that, when the combination of the above measures fails, the kissing wire technique may be a reasonable option in some cases. Modified microcatheter rendezvous was also an option if the retrograde wire could cross the occluded segment.
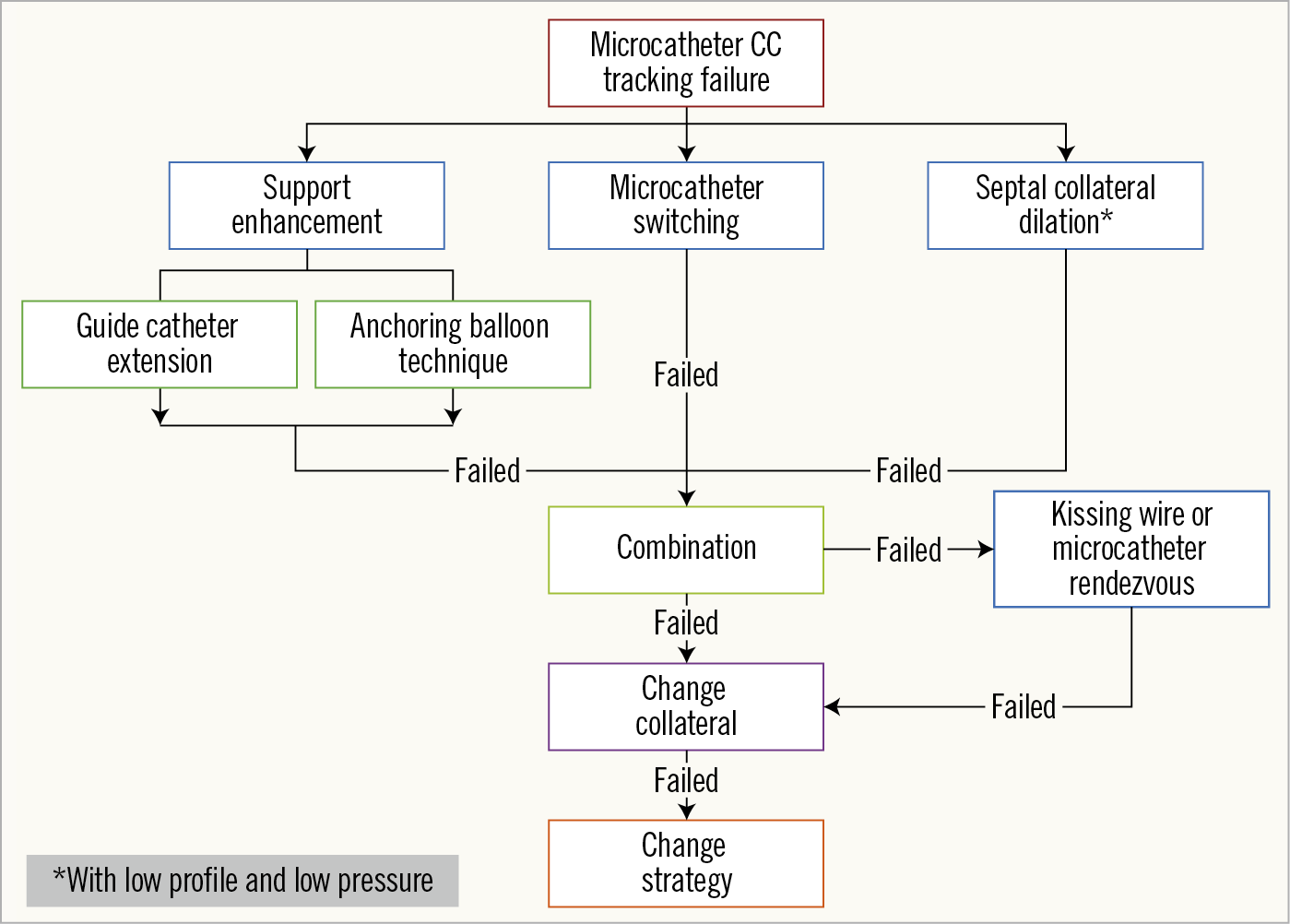
Figure 3. Flow chart of management strategies for microcatheter CC tracking failure.
Limitations
Several limitations of the present study should be mentioned. First, the retrospective, single-centre study design may have resulted in potential for bias in patient selection and interventional strategy. Second, both high-volume and non-high-volume operators were involved in this study. While there were no significant differences in procedural characteristics between the two groups, a higher J-CTO score (3.0±1.0 vs. 2.8±0.9, p=0.042) was noted in the high-volume operator group. The high-volume operator group also demonstrated a higher wire CC tracking success rate (79.3% vs. 64.6%, p=0.004) and overall procedural success rate (82.2% vs. 60.4%, p<0.001) (n=371). However, after wire CC tracking success (n=280), there were no significant differences in initial microcatheter CC tracking failure between high- and non-high-volume operators (Table 2). Third, the J-CTO score (3.0±1.0) in the present study was relatively higher than in some registries. This may be partly related to the specificity of the retrograde subgroup and heterogeneous evaluation among operators. Fourth, this study included a relatively small sample size and it may need a future large prospective study to validate its findings. Fifth, the average contrast consumption was 382.9±142.7 ml, which may be related to the high proportion of rescue retrograde approach use after a failed antegrade attempt (73.3%). Additionally, even with widely used perioperative hydration, more attention needs to be paid to control contrast consumption.
Conclusions
Initial microcatheter CC tracking failure was observed in 22.5% of successful wire CC tracking procedures. For septal collaterals, CC 0-1 collaterals, channel entry angle <90°, and channel exit angle <90° were independent angiographic predictors of initial microcatheter CC tracking failure after wire CC tracking success. CC 1 collaterals were identified as the only independent predictor in epicardial collaterals.
|
Impact on daily practice Currently, data on microcatheter collateral tracking in retrograde percutaneous coronary intervention for chronic total occlusion lesions are very limited. Clarification of the angiographic predictors and management experience of microcatheter collateral tracking failure will be of significant benefit in procedure planning and will allow appropriate treatment. |
Acknowledgements
The authors would like to thank Steve Huang (Shanghai Institute of Cardiovascular Diseases, Zhongshan Hospital, Fudan University) for language editing support. The authors also wish to acknowledge the cardiac interventional specialists who contributed to the database of the CTOCC.
Funding
This study was funded by Shanghai Sailing Program (No. 16YF1401600) and National Key R&D Program of China (No. 2016YFC1301200).
Conflict of interest statement
The authors have no conflicts of interest to declare.