Abstract
Aims: To assess the incidence and impact on clinical outcomes of subintimal tracking in patients undergoing percutaneous coronary intervention for chronic total occlusion (CTO).
Methods and results: Patients at 27 centres were consecutively enrolled when guidewire crossing of the CTO by either the antegrade or the retrograde approach was confirmed by intravascular ultrasound (IVUS). IVUS images were examined to identify the course of the wire. Clinical follow-up at one year and angiographic follow-up at nine months were performed after everolimus-eluting stent implantation. Among a total of 163 patients (59 antegrade and 104 retrograde), subintimal tracking was more frequent with the retrograde approach (24.2% vs. 12.3%, p=0.10). Although there was no difference in the one-year target vessel revascularisation rate between intimal and subintimal tracking with either the antegrade or the retrograde approach, angiographic follow-up revealed greater late loss in the subintimal group compared with the intimal group. Multivariate analysis identified the pre-procedural reference diameter as a predictor of subintimal tracking.
Conclusions: Subintimal tracking was more frequent with the retrograde approach. After medium-term follow-up, no negative clinical impact of subintimal tracking was observed in this small study. However, further evaluation of the angiographic impact is needed.
Introduction
Since the introduction of the retrograde approach via native collateral channels and the controlled antegrade retrograde tracking (CART) technique1,2, this technique has been widely adopted and has contributed to an increase in the success rate of percutaneous coronary intervention (PCI)3-5. Recently, the procedures for the retrograde approach have been refined and have almost been standardised with the development of new dedicated devices6. The reverse CART technique is commonly used for the retrograde approach, but this technique is associated with the possibility of subintimal tracking7,8. However, the incidence and impact on outcomes of subintimal tracking have not been adequately evaluated in the drug-eluting stent (DES) era. Therefore, we conducted the present multicentre registry to investigate these issues by using intravascular ultrasound (IVUS) to identify intimal and subintimal tracking in patients receiving second-generation DES after successful crossing of a CTO by either the antegrade or the retrograde approach.
Methods
STUDY DESIGN
J-PROCTOR (PROmus stent treatment of Chronic Total Occlusions using two different Recanalisation techniques in Japan) is a prospective multicentre registry study involving 27 Japanese hospitals. The definition of CTO and the inclusion criteria have been reported previously7. Exclusion criteria were renal failure (serum creatinine of 3.0 mg/dL or higher), haemodialysis, saphenous vein graft lesions, and in-stent restenosis. All patients were consecutively enrolled at each institution at the time when either antegrade or retrograde guidewire crossing of the CTO was confirmed by IVUS with or without a 1.5 mm balloon. The treatment strategy for CTO was selected by each operator at his/her discretion. Because this was a pilot observational study, the enrolment targets were set at 50 patients for the antegrade approach and 100 patients for the retrograde approach. In each patient, IVUS examination and predilatation were performed, after which an everolimus-eluting stent (EES) (PROMUS™ stent; Boston Scientific, Natick, MA, USA) was deployed so that it completely covered the lesion afterwards. The technique used for the retrograde approach has been described previously6,8. Antiplatelet therapy was commenced at least three days prior to PCI, with aspirin (100 mg/day) and ticlopidine (200 mg/day) or clopidogrel (75 mg/day), and was continued for at least one year after the procedure. Patients underwent follow-up coronary angiography at nine months and returned to hospital for review at 12 months after PCI. The primary endpoint was the target vessel revascularisation (TVR) rate at 12 months after PCI, while the secondary endpoints were major adverse cardiac events (MACE) at 12 months and quantitative coronary angiography (QCA) parameters obtained by follow-up coronary angiography. Procedural success was defined as recanalisation of the target lesion with restoration of grade 3 Thrombolysis In Myocardial Infarction (TIMI) flow and <50% residual stenosis. MACE were classified as cardiac death, Q-wave myocardial infarction, and coronary artery bypass grafting. Non-Q-wave MI was diagnosed when the creatine kinase-MB level exceeded three times the upper limit of the normal range.
The study protocol was approved by the institutional review board of each participating hospital and informed consent was obtained from all of the patients. The Safety Committee for this study was independently established by a third-party organisation (Itabashi Chuo Hospital, Tokyo, Japan).
ANALYSIS OF ANGIOGRAPHIC AND IVUS IMAGES
QCA and analysis of IVUS findings were performed at an independent core laboratory (Japan Cardiovascular Imaging Core Laboratory, Tokyo, Japan). QCA was performed by two trained angiographic technicians who used an automated edge detection system (QCA-CMS version 6.0; Medis medical imaging systems bv, Leiden, The Netherlands) to measure the reference diameter, the minimum lumen diameter, and the lengths of the occlusion and the stented segment. Aneurysm formation was defined as expansion of the lumen by at least 20% compared with the normal diameter in the treated region, which extended beyond the apparent normal vessel contour. Recorded IVUS images were analysed by an independent expert who categorised the patients into an intimal plaque tracking group or a subintimal tracking group (intimal or subintimal groups). The definitions and IVUS images of intimal plaque tracking and subintimal tracking are shown in Figure 1.
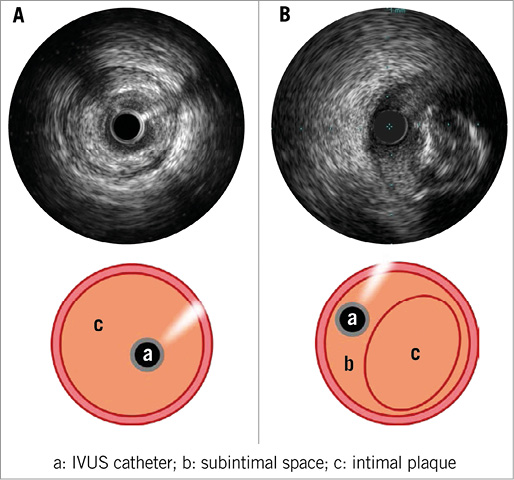
Figure 1. Intimal plaque tracking versus subintimal tracking on IVUS. Intimal plaque tracking was defined as detection of the IVUS catheter in the true lumen surrounded by dissection with/without haematoma (A). Subintimal tracking was defined as detection of the IVUS catheter in a dissection plane outside the intimal plaque, but inside the EEM, even when this finding was localised (B).
In patients with TVR, the location and pattern of angiographic restenosis were analysed by the core laboratory. In-stent restenosis was classified according to a previous report9. The site of restenosis was evaluated in relation to the original occluded segment by careful retrospective analysis of the pre-procedural and follow-up angiograms. In patients from the subintimal group with TVR, the site of restenosis was evaluated in relation to the subintimal tracking segment by comparing post-procedural IVUS and angiographic images with findings at follow-up angiography.
STATISTICAL ANALYSIS
Categorical variables are reported as percentages and continuous variables are shown as the mean±standard deviation. Either the chi-square test or Fisher’s exact test was used for analysis of categorical variables, while the unpaired Student’s t-test and the Wilcoxon test were employed for continuous variables. Logistic regression analysis was performed to identify independent predictors of subintimal tracking by entering baseline patient and lesion characteristics, including the QCA data. All statistical analyses were performed with SAS version 9.2 (SAS Institute, Cary, NC, USA), and p<0.05 was considered to indicate statistical significance.
Results
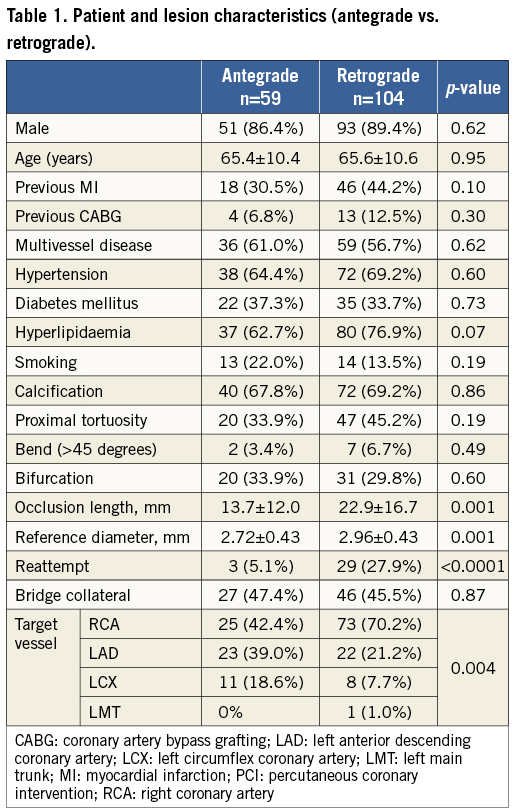
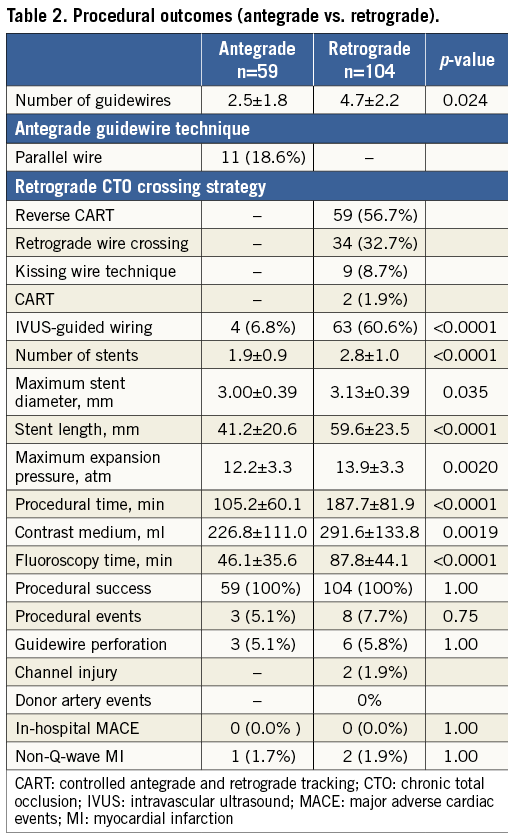
BASELINE CHARACTERISTICS AND PROCEDURAL OUTCOME
A total of 163 patients (59 treated by the antegrade approach and 104 treated by the retrograde approach) were enrolled from October 2010 to October 2011. The baseline patient and lesion characteristics are listed in Table 1. The right coronary was more frequently treated by the retrograde approach. The retrograde patients also had a longer occlusion length, a larger reference diameter, and more frequent reattempt PCI. Table 2 summarises the procedural data for both approaches. The CART technique was used in 58.6% of the retrograde patients. IVUS was more frequently employed for successful wiring in the retrograde patients, suggesting that the IVUS-guided reverse CART technique was also popular10. Furthermore, the stents were significantly longer in the retrograde patients. Procedural success was achieved in all patients treated by either approach and there were no differences in procedural events or in-hospital MACE.
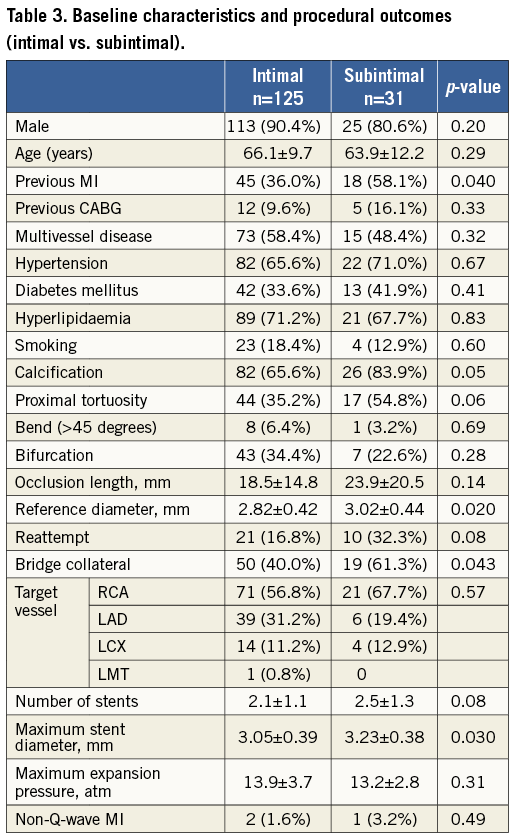
IVUS FINDINGS AND COMPARISON OF GROUPS CATEGORISED BY IVUS
Seven patients were excluded due to poor IVUS image quality, so 156 patients were analysed (57 in the antegrade group and 99 in the retrograde group). IVUS revealed subintimal tracking in 12.3% (7/57) of the antegrade patients versus 24.2% (24/99) of the retrograde patients (Figure 2). Although subintimal tracking was more frequent with the retrograde approach, the difference did not reach statistical significance (p=0.10). Baseline characteristics and procedural outcomes are compared between the intimal and subintimal groups in Table 3. Patients in the subintimal group had more complicated lesions with calcification or bridging collaterals, and were also more likely to be undergoing reattempt PCI. The pre-procedural reference diameter was significantly larger in the subintimal group.
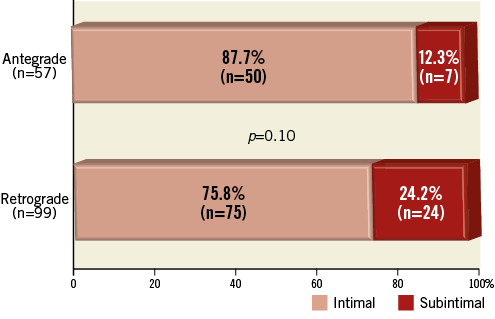
Figure 2. Incidence of subintimal tracking with the antegrade and retrograde approaches. Subintimal tracking was more frequent with the retrograde approach.
CLINICAL OUTCOME AT 12 MONTHS
Twelve-month follow-up data were obtained in all patients. One patient treated by the retrograde approach with intimal plaque tracking died from injuries sustained in an accident, but there were no MACE and no episodes of subacute or late thrombosis in either the intimal or the subintimal group. The TVR rate (primary endpoint) was 10.4% (13/125) in the intimal group and 12.9% (4/31) in the subintimal group (Figure 3). There was also little difference between the intimal and subintimal groups irrespective of whether the antegrade or retrograde approach had been employed for PCI.
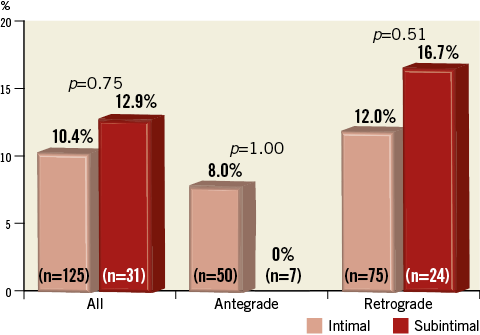
Figure 3. TVR rate in the intimal and subintimal groups. The TVR rate did not differ between the intimal and subintimal groups or between the antegrade and retrograde approaches.
QCA FINDINGS
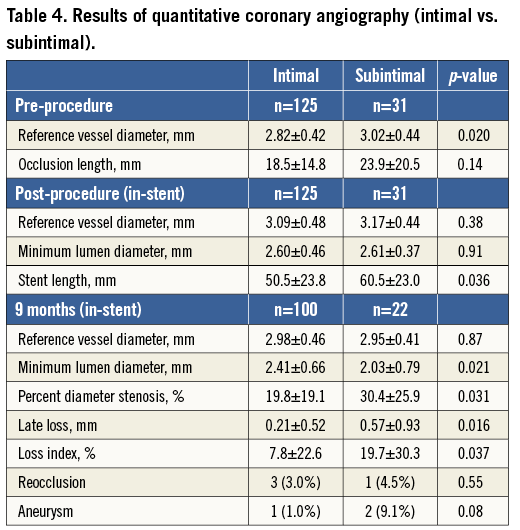
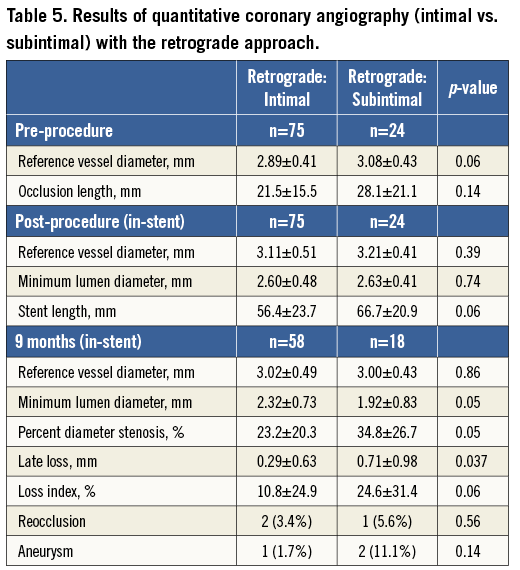
Table 4 compares acute and follow-up QCA results between the intimal and subintimal groups. Follow-up angiography was performed in 78.2% (122/156) of the patients. Post-procedural QCA revealed that the stented segment was significantly longer in the subintimal group. At follow-up, the percent diameter stenosis, late loss, and loss index were significantly smaller in the intimal group compared with the subintimal group, although the loss index was only 7.8% and 19.7%, respectively. Reocclusion and aneurysm formation were more frequent in the subintimal group, but the differences were not significant. Among patients treated by the retrograde approach (Table 5), QCA revealed that the stent length tended to be longer in the subintimal group. Follow-up showed that QCA parameters were significantly better in the intimal group. Aneurysm formation was only observed in the retrograde approach. Despite no significant difference, its incidence in the subintimal group was approximately five times higher than in the intimal group.
SITE AND PATTERN OF RESTENOSIS
The site and pattern of restenosis in patients who required TVR are summarised in Table 6. There were no differences between the intimal and subintimal groups regarding the site of restenosis and the pattern of ISR. Among the four patients with TVR from the subintimal group, one patient developed stent occlusion.
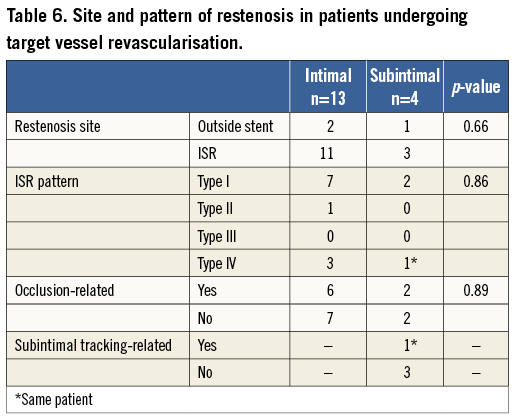
The sites of focal restenosis requiring TVR were not related to subintimal tracking in the other three patients.
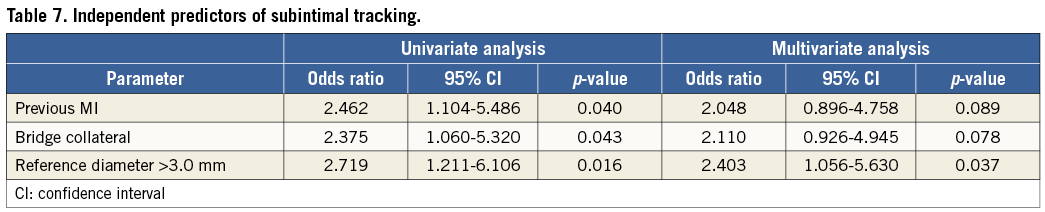
MULTIVARIATE ANALYSIS
Table 7 displays the results of multivariate analysis. Among the three parameters that were found to be significant by univariate analysis, only a larger pre-procedural reference vessel diameter was an independent predictor of subintimal tracking according to multivariate analysis (odds ratio: 2.403, 95% confidence interval: 1.056 to 5.630, p=0.037).
Discussion
The main findings of the present study can be summarised as follows. 1) In patients undergoing successful treatment of CTO, subintimal tracking was more frequent when the retrograde approach was employed than with the antegrade approach. 2) Clinical outcomes at one year were not influenced by subintimal tracking with either approach, although greater angiographic lumen loss was observed in the subintimal group.
There is limited information about the frequency of subintimal tracking when PCI is performed for CTO, including the retrograde approach11,12. Muhammad et al detected a high frequency of subintimal tracking by IVUS (45%) in patients with successful PCI for CTO, but they only studied 26 patients and the retrograde approach was only applied in four cases11. In addition, the occlusion length was longer in their study (>40 mm) than in the current study (14 mm in the antegrade group). Tsujita et al analysed subintimal tracking in 48 patients, 25 of whom were treated by the retrograde approach12, and reported that the incidence of subintimal tracking was significantly higher in the retrograde group (40% vs. 9%; p=0.02). This difference from the present study may possibly be explained by the smaller number of subjects (25 vs. 99), longer occlusion length (45 vs. 23 mm), and different treatment strategy compared with the current retrograde approach that has evolved since the introduction of channel dilators6,7. On the other hand, the incidence of subintimal tracking associated with the antegrade approach was similar to our result (9% vs. 12.3%), and the occlusion length was also similar (18 mm vs. 14 mm). Taking these findings together11, it seems that the CTO length may influence the incidence of subintimal tracking for both the antegrade and the retrograde approaches. The present findings also suggest that the incidence of subintimal tracking is not low with the antegrade approach, even though intentional subintimal tracking and re-entry techniques13,14 were not employed in our study population. Conversely, subintimal tracking is not so common with the contemporary retrograde approach, even though the reverse CART technique (with a higher theoretical risk of subintimal tracking) is used in more than half of all patients7. This suggests that reverse CART may often create an intraplaque connection in the occlusion when properly applied. The only significant predictor of subintimal tracking in the present study was a larger pre-procedural reference diameter, which may be explained by the higher frequency of right coronary artery lesions in the subintimal group.
There were two previous reports on IVUS findings, but follow-up data were not provided11,12. In the present study, there was no difference in the 12-month TVR rate between the intimal and subintimal groups whether treated by the antegrade or the retrograde approach. The overall TVR rates in this study were comparable to those in previous reports on EES implantation after successful recanalisation of CTO15,16. Use of a second-generation DES may explain the favourable clinical outcome in this study17. Although no negative clinical impact of subintimal tracking was observed at medium-term follow-up, our findings do not support the intentional subintimal tracking and re-entry technique for which high reocclusion rates have been reported (35-41%)13,14. It was recently reported that this technique only achieves a post-procedural TIMI grade 3 flow in 60% of patients and that its use is the strongest predictor of reocclusion17. In our study, post-procedural TIMI grade 3 flow was achieved in all patients, suggesting that the subintimal tracking distance was limited in our subjects and the distal main branches were well preserved. Furthermore, the PCI strategy employed in the present study is not comparable to the recently reported hybrid algorithm18. Results of ongoing hybrid registries are anticipated in the near future.
In the present study, the longer occlusion and stent lengths in the subintimal group compared with the intimal group influenced follow-up angiographic outcomes such as late loss. Furthermore, although there were no significant differences, reocclusion and aneurysm rates were higher in the subintimal group in this small pilot study. Analysis stratified by the site and pattern of restenosis showed that restenosis did not always occur in the segment affected by subintimal tracking, but the angiographic impact of subintimal tracking needs to be carefully evaluated in the future by investigating an adequate number of subjects.
Limitations
The limitations of this study were as follows. 1) All procedures were performed by skilled and experienced interventional cardiologists, so the results may have differed if less experienced physicians had been involved. 2) The number of patients enrolled was too small for adequate statistical analysis. 3) The subintimal tracking distance could not be measured in all patients because the IVUS catheter was selected at the discretion of each institution. 4) The angiographic follow-up rate was relatively low. 5) The clinical follow-up period was too short to assess completely the safety of subintimal DES stenting, including the risk of late stent thrombosis, particularly in patients with aneurysm formation19,20.
Conclusions
Subintimal tracking was more frequent with the retrograde approach than with the antegrade approach. Although there was no apparent negative clinical impact of subintimal tracking at one year after EES implantation by either the antegrade or the retrograde approach, some angiographic influence was observed. Because this was a small pilot study, further evaluation is required to confirm these findings.
| Impact on daily practice In the present study, clinical outcomes at one year showed no significant difference between the subintimal group and the intimal group despite greater angiographic lumen loss in the former group. The results of the study indicate that intentional subintimal tracking using a technique like the knuckle wire is not recommended. The favourable outcomes achieved in our study were due to a shortened subintimal space and a secure distal branch, resulting in better TIMI grade. Therefore, proper wiring techniques with available technologies must be utilised to minimise subintimal tracking. |
Acknowledgements
The authors are indebted to T. Matsubara, Y. Nozaki, Y. Igarashi, Y. Hamazaki, K. Wagatsuma, E. Kyo, Y. Takeda, M. Nakayama, M. Yamane, M. Okada, M. Okutsu, R. Kametani, E. Nozaki, H. Ohira, M. Iwabuchi, M. Kijima, and Y. Yamamoto for patient recruitment. They are also indebted to S. Ito, A. Endo and K. Kinoshita for performing QCA and IVUS image analysis.
Funding
This study was sponsored by the Retrograde Summit study organisation with grant support from Asahi Intecc Corporation and Boston Scientific Corporation.
Conflict of interest statement
E. Tsuchikane is a consultant for Asahi Intecc, Abbott Vascular, and Boston Scientific. T. Fujita is a consultant for Terumo. The other authors have no conflicts of interest to declare.

