The right coronary artery (RCA) is the most common target vessel for chronic total occlusion (CTO) percutaneous coronary intervention (PCI), accounting for 44% of target lesions in the multicentre CTO registry in Japan (J-CTO)1, 50% in the European Registry of Chronic Total Occlusion (ERCTO)2, and 59% in the Prospective Global Registry for the Study of Chronic Total Occlusion Intervention (Progress CTO)3. The exact reasons underlying this high prevalence are unclear. Possible contributing factors may include the long length that the RCA runs in the atrioventricular groove before it bifurcates into the posterior descending and posterolateral arteries. The poor long-term patency of saphenous vein grafts4 in contrast to the excellent patency of internal mammary grafts also results in the native occluded vessel becoming clinically relevant following bypass surgery5.
Given the high prevalence of RCA CTOs, strategies for successfully recanalising them are very important to the CTO operator and can be broadly categorised as antegrade and retrograde. Antegrade crossing can be achieved with wire escalation or antegrade dissection/re-entry6. A dissection/re-entry strategy can be liberally leveraged in the RCA because possible occlusion of acute marginal branches caused by dissection typically does not cause adverse consequences. Retrograde crossing can be achieved most commonly via collaterals from the left anterior descending artery (usually septal but also epicardial), but can also be performed via saphenous vein grafts (patent or occluded7), and through ipsilateral collaterals8,9 (Figure 1).
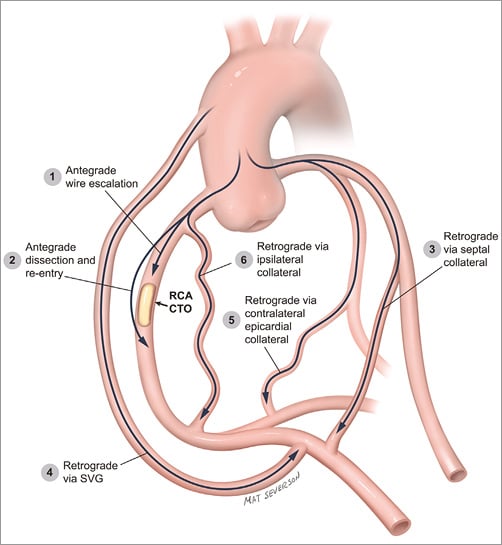
Figure 1. Crossing options for patients with right coronary artery chronic total occlusions.
Selection of the optimal crossing strategy for RCA CTOs starts with a careful review of the angiogram, ideally using dual injections through large-bore guide catheters6. Angiogram review is best done with all members of the cardiac catheterisation team in a highly interactive fashion. Four key questions are asked: 1) where does the occlusion start? 2) how long is it? 3) what is the quality of the distal vessel? and 4) are interventional collaterals present6,10? Starting from these questions a brainstorming session ensues with initial emphasis on quantity, identifying and writing down all possible crossing options. In the next step the options are ranked in terms of feasibility and safety arriving at the final “plan of attack”. The plan is not set in stone, but is flexible and can change at any time depending on new information obtained during the procedure. It is critical to have a pre-procedural plan, or important options may be missed “in the heat of the battle”!
In general, an initial antegrade crossing attempt is preferred for most patients, as use of the retrograde approach is often associated with higher risk11 for periprocedural myocardial infarction12,13, donor vessel injury, and collateral perforation, that can be very challenging to control, especially in epicardial collaterals14. However, in some cases a primary retrograde approach is preferred, especially in cases with proximal CTO cap ambiguity, or poor landing zones secondary to an important bifurcation or a diffusely diseased distal vessel.
Use of the retrograde approach is commonly required for RCA CTOs15. In the ERCTO retrograde registry the RCA represented 70.4% of all CTO lesions16. Retrograde crossing of RCA CTOs is most commonly performed via septal collaterals. Septal collaterals are relatively easy to cross and carry low risk for complications if traumatised, although septal haematomas causing compression have been reported17. Saphenous vein bypass grafts (SVGs) are also favourable conduits for retrograde RCA CTO crossing with a low risk of perforation. On occasions, retrograde wiring into the RCA after the touchdown of the distal SVG anastomosis can be challenging and may require the use of an angled tip microcatheter such as the SuperCross™ (Vascular Solutions, Inc., Minneapolis, MN, USA) or a deflectable tip microcatheter such as the Venture® catheter (Vascular Solutions)18. Retrograde crossing of occluded SVGs is more successful in recently occluded SVGs with a clear proximal funnelled stump and is usually achieved with a Corsair microcatheter (ASAHI Intecc, Aichi, Japan) and a PILOT 200 guidewire (Abbott Vascular, Santa Clara, CA, USA). The third option for retrograde crossing of RCA CTOs is the use of ipsilateral collaterals, which is an infrequently performed procedure. In this issue of the Journal, Mashayekhi et al elegantly provide a thorough, detailed, and practical description of how to use ipsilateral collaterals for RCA CTO PCI19.
First, careful attention should be paid to performing optimal coronary angiography. Ipsilateral collaterals often arise close to the RCA ostium or from a separate ostium. Hence, suboptimal visualisation may occur when injections are performed with the catheter deeply intubated. Contrary to standard RCA CTO PCI in which an Amplatz 1 or Amplatz 0.75 guide is used to engage the RCA, a JR4 guide with side holes to allow contrast to fill the proximal RCA directly and indirectly may be a better choice for ipsilateral collateral visualisation and crossing.
Second, the authors demonstrate that ipsilateral collaterals of the RCA are not uncommon; they were present in 30% of RCA CTOs. The majority of these (66%) follow an epimyocardial course as opposed to an intramyocardial path.
Third, in Figure1 of their article, the authors classified and illustrated five types of ipsilateral collaterals based upon their origin and the course of the collateral. Although epimyocardial collaterals as a whole are more frequently encountered than intramyocardial collaterals, when subdividing all ipsilateral collaterals into these five categories, a septal intramyocardial course from the proximal RCA to the posterior descending or posterolateral arteries is the most commonly encountered (type E, 34% of all collaterals). Type A epimyocardial collaterals, originating from a high acute marginal branch and inserting to the right posterolateral artery or originating from a lower acute marginal branch and inserting to the posterior descending artery, were the next most frequently observed connection (21% of all collaterals). Type B collaterals (connecting distal ends of higher and lower acute marginal branches) represented 19% of all collaterals. Type D collaterals (originating from the proximal RCA and inserting in the posterolateral branch) and the morphologically similar type C collaterals (originating in the proximal RCA and inserting close to the posterior descending/posterolateral branch bifurcation) represented 17% and 9% of all collaterals, respectively. The main conclusion and practical implication from this classification is that type B collaterals appear to be the least suitable for the retrograde approach because of small size and high tortuosity, increasing the risk of injury and rupture, and they should therefore be avoided.
Fourth, crossing of ipsilateral RCA collaterals may be best attempted with a Sion™ guidewire (ASAHI Intecc), as is standard for most retrograde procedures currently.
Fifth, the microcatheter may need to be changed during collateral crossing attempts when trying to achieve a balance between crossability (with the NHancer™; IMDS, Roden, The Netherlands) and support (with the Corsair).
Sixth, avoiding guidewire externalisation may minimise the risk of collateral vessel injury by minimising the shear tension applied to the collateral. Alternatives to externalisation are the use of the retrograde guidewire as a marker for antegrade crossing, or the use of the “tip-in” technique if retrograde guidewire crossing is achieved. In the “tip-in” technique20, the retrograde guidewire is advanced into an antegrade microcatheter that can then be tracked over the retrograde guidewire through the lesion, enabling antegrade wiring and stenting20. This is easier to achieve when the retrograde guidewire enters the antegrade guide catheter, but can also be performed within the proximal portion of the CTO vessel segment.
Seventh, if externalisation is pursued, it can be facilitated by use of a second guide catheter in a “ping-pong” fashion, alternating engagement of the RCA with the “retrograde” guide catheter (through which the retrograde guidewire is advanced) and the “antegrade” guide catheter (that receives the retrograde guidewire after CTO crossing).
Using the above techniques Mashayekhi et al successfully treated eight of nine attempted lesions, achieving an overall phenomenal success rate of 94% for RCA CTOs.
Who should perform ipsilateral collateral retrograde RCA CTO PCI? This is clearly not a procedure for the novice CTO operator, or even the novice retrograde operator. It should be performed by expert operators with extensive experience in retrograde CTO PCI and advanced technical skills. Moreover, it should be performed at centres that can treat potential complications, such as epicardial vessel perforation. Such centres should have equipment for sealing perforations, such as coils21, microparticles, or thrombin14, and access to cardiac surgery. Epicardial vessel perforation may require treatment from both sides of the perforation that could be challenging if the CTO has not been successfully recanalised22.
Recanalising RCA CTOs can be challenging, but can also provide important clinical benefits23. Having multiple crossing options (Figure 1) is critical for high success rates. Retrograde crossing via ipsilateral collaterals has a limited, yet important role in the quest to restore RCA patency. Our patients stand to derive the benefits from application of this elegant advance in retrograde CTO PCI.
Conflict of interest statement
E.S. Brilakis has received consulting/speaker honoraria from Abbott Vascular, ASAHI, Boston Scientific, Elsevier, Somahlution, St. Jude Medical and Terumo, and research support from Infraredx and Boston Scientific. His spouse is an employee of Medtronic. W.J. Nicholson has received consulting/speaker honoraria from Abbott Vascular, ASAHI, Boston Scientific and Edwards Lifesciences, and intellectual property royalties from Vascular Solutions.