CASE SUMMARY
BACKGROUND: Percutaneous attempts to open chronic total occlusion (CTO) of native coronaries are associated with a significantly lower procedural success rate than the patent subset of lesions. The retrograde approach represents one of the most sophisticated and technically challenging alternatives to open a CTO after an unsuccessful anterograde attempt or as a primary approach according to the operator’s experience.
INVESTIGATION: Physical examination, ECG, echocardiography, coronary angiography.
DIAGNOSIS: CTO.
MANAGEMENT: Repeat CTO PCI.
KEYWORDS: chronic total occlusion, retrograde, saphenous vein graft
PRESENTATION OF THE CASE
A 73-year-old man with a history of myocardial infarction of the anterior and lateral wall in 1994, coronary artery bypass grafting in 1999 (left internal mammary artery [LIMA] to the left anterior descending coronary artery [LAD] and saphenous vein graft [SVG] to the right coronary artery [RCA]), balloon angioplasty of the RCA via the SVG in 2004, was referred for further treatment. He remained in CCS functional class III, despite optimal medical treatment.
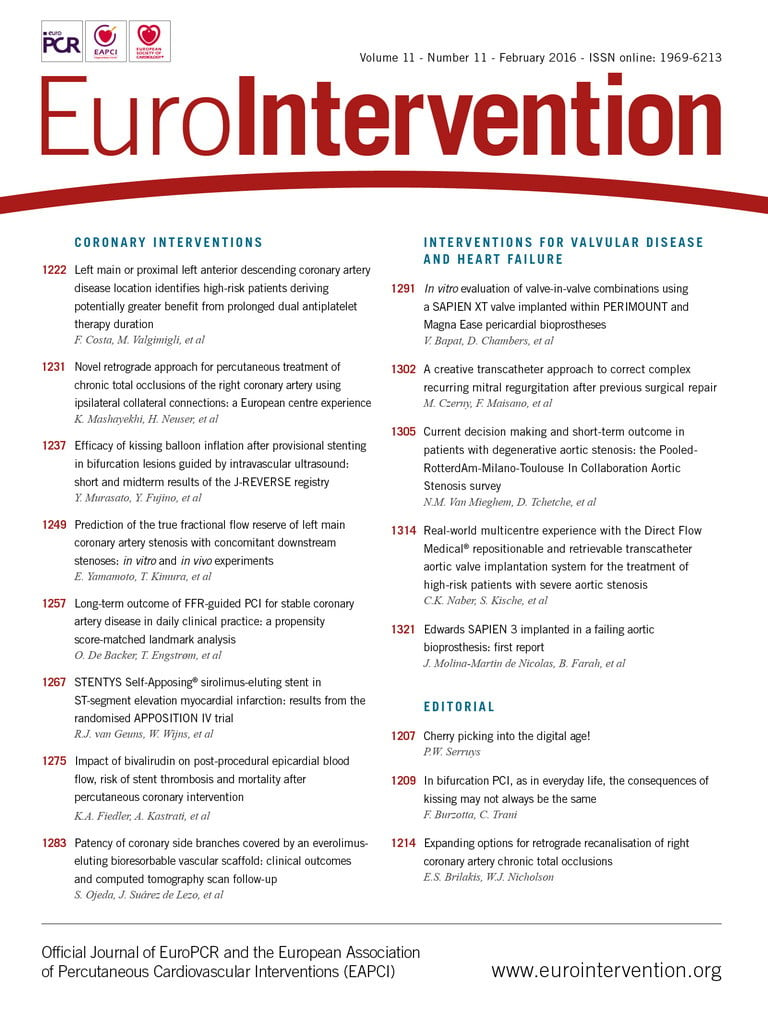
Control angiography revealed an RCA CTO and an ostial CTO of the SVG to the RCA without any visible stump, retrograde contrast filling of the distal RCA segment, as well as a CTO of the distal LAD with a patent LIMA to the LAD (Figure 1). Thus, an attempt to open the RCA CTO was carried out. However, neither the anterograde approach with guidewires (ULTIMATEbros 3, Fielder FC and CONFIANZA PRO 12; ASAHI Intecc., Aichi, Japan), nor the retrograde attempt using soft wires (Fielder FC and SION; ASAHI Intecc) with the support of a Corsair microcatheter (ASAHI Intecc) could cross the RCA CTO (Figure 2).
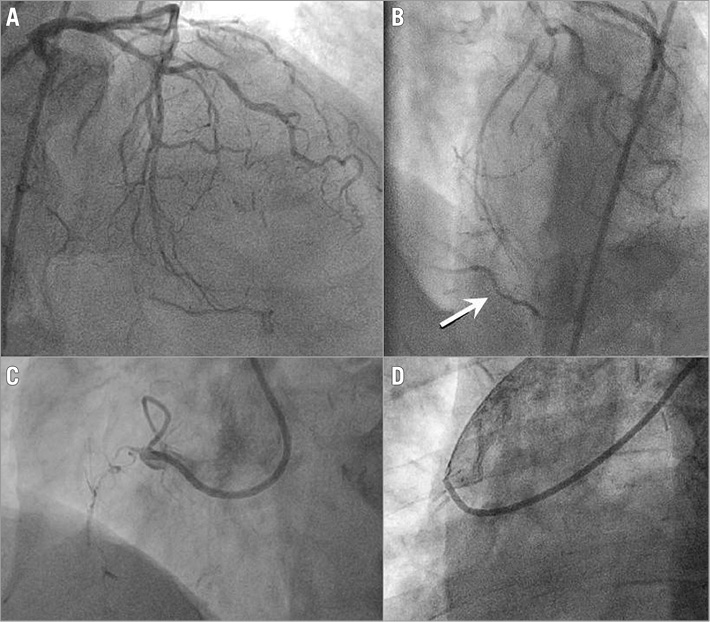
Figure 1. Coronary angiography. A) Occluded left anterior descending coronary artery and retrograde filling of the distal segment of the right coronary artery. B) Magnification of panel A - distal segment of the right coronary artery (arrow). C) Stumpless occlusion of the right coronary artery. D) Stumpless occlusion of the saphenous vein graft.
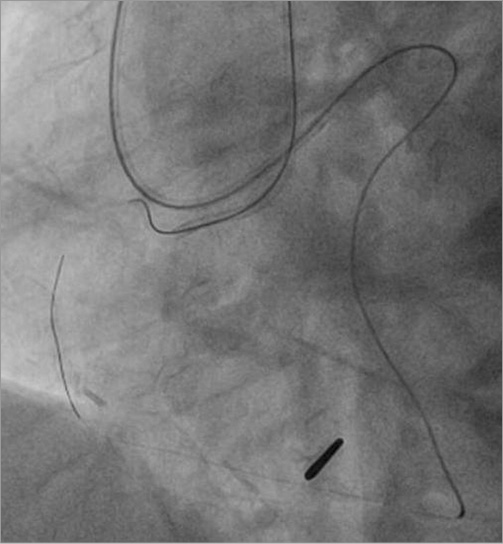
Figure 2. Unsuccessful attempt to open the right coronary artery occlusion anterogradely and retrogradely.
Four months later the patient was admitted for a second attempt to treat the CTO.
How would I treat?
THE INVITED EXPERT’S OPINION

It is a frequent observation that venous grafts supplying native chronic coronary total occlusions (CTO) do not remain patent1, and more than 20% of CTO cases are native CTOs after graft failure. In my practice I will never attempt to open a saphenous venous graft (SVG) as the patency after PCI is extremely poor. It may be argued that one might access the native artery from this reopened graft to recanalise the native artery in a second step. There are also reports of using the occluded SVG as an access to open the native RCA, but in this specific case the retrograde access from the proximal LAD via the septum had already proven to be accessible in the first attempt.
In the brief description of the previous attempt we see that a retrograde wire was advanced via a septal access very far into the occlusion. It is mentioned that the retrograde wires were soft wires. We also see that the Corsair microcatheter (ASAHI Intecc) was not advanced far into the occluded artery and was very far distal from the position of the retrograde wire. The mode of failure here was most likely the inability to advance the microcatheter. As far as we can see from the diagnostic image, there is a septal connection of size CC2 to the RCA. With a properly sized guide (7 Fr) and an aggressive shape (EBU 4.0) the passage of the Corsair should be possible. It looks like these catheters were used, but then there are still a few collaterals that are difficult to pass. If patient rotating anticlockwise with the Corsair does not work, balloon dilatation of the septal collateral with a 1.25 mm balloon at 4 atm can open the path, or change of the Corsair to a new one (there may be loss of coating or damage to the tip) or finally also switching to a FineCross® microcatheter (Terumo Corp., Tokyo, Japan) will do the trick. At any rate, the anatomic situation of this case can be solved by the appropriate approach. The microcatheter can then be advanced distal to the occlusion and dedicated wires can be used. My first choice would be the ULTIMATEbros 3, then Gaia Second, then CONFIANZA PRO 12 (all ASAHI Intecc).
At the same time, the antegrade access towards this distal wire target is required. The guide catheter can be a short Amplatz 1.0 or 0.75 7 Fr. Here we can see an ideal conus branch to anchor the antegrade guide to help support the antegrade wire manipulation. Anchoring should be done right away as the first step. I would choose a short Corsair (ASAHI Intecc) in this particular situation as a support catheter and a Gaia Second wire as first choice, then escalate up to CONFIANZA PRO 12. With the distal wire as target and an anchored guide it will be possible to reach an overlap position of the antegrade wire and the retrograde wire, and then proceed to a standard reverse CART procedure with antegrade balloon passage and then retrograde wire passage along the balloon. Then reach the guide with the wire, trap this retrograde wire and follow with the microcatheter, then exchange for the RG3 externalisation wire (ASAHI Intecc) and finish the case over this externalised wire.
Conflict of interest statement
The author has no conflicts of interest to declare.
How would I treat?
THE INVITED EXPERT’S OPINION

The case presented by Debski and colleagues is that of a complex chronic total occlusion (CTO) of a right coronary artery (RCA) in a patient post-coronary artery bypass graft (CABG) surgery with graft failure. The authors have already attempted to recanalise the RCA once (with a combination of an antegrade and retrograde approach, only with wire escalation techniques). However, the attempt failed despite multiple wires.
As we do not have moving images but rather only Figures, it is difficult to judge this CTO properly; however, we believe the J-CTO score of this lesion should be 4 (length more than 20 mm, calcifications, bends >45 degrees in the CTO segment, previous failure). The only point missing is the lack of a blunt stump of the proximal cap.
If we analyse the lesion keeping in mind the hybrid approach, this lesion has a non-ambiguous proximal cap, is longer than 20 mm, seems to have a good distal landing zone and does not have a distal cap located at a bifurcation.
If we consider reattempting the CTO with the hybrid approach, probably a dissection re-entry technique would be indicated, mainly because of the length of the lesion. However, it seems that there is a small antegrade microchannel, quite straight, connecting the proximal to the distal cap.
Given all these considerations, I would reattempt the same lesion using the hybrid algorithm. I would start with an antegrade 8 Fr guiding catheter (Amplatz left curve in order to have good support) from the femoral artery and I would also be prepared to go retrograde with a 6 Fr guiding catheter (extra back-up curve) from the radial artery. Practically all techniques of the hybrid algorithm are possible with this set-up. I would consider attempting an antegrade wire escalation technique with an extremely hydrophilic and tapered wire with low tip load, such as a Fielder XT-A (ASAHI Intecc), and support of a microcatheter (FineCross; Terumo Corp., or SuperCross™; Vascular Solutions, Minneapolis, MN, USA). If this attempt fails, I would switch to an antegrade dissection re-entry technique, using the CrossBoss™ (Boston Scientific, Marlborough, MA, USA) catheter to pass into the subintimal space, and the Stingray™ (Boston Scientific) balloon and wire to attempt controlled re-entry in the distal RCA before the crux (as there seems to be a good landing zone for re-entry at this level). If this attempt also fails (if the landing zone is not so favourable or if too much subintimal haematoma does not allow a proper attempt at re-entry), the last resort would be to attempt a reverse controlled antegrade retrograde subintimal tracking, with a retrograde microcatheter (Corsair; ASAHI, or Turnpike; Vascular Solutions) sent purposely into the subintimal space, eventually with a knuckle wire technique (the authors have shown that it is possible to pass to the distal RCA via the septal collaterals of the LAD, thus a retrograde approach would definitely be feasible again) and aggressive balloon dilatation of the subintimal space antegrade (once again eventually using a knuckle wire to pass into the subintimal space) to try to allow the retrograde subintimal wire to re-enter the true lumen in the proximal RCA and allow the performance of a loop with a long wire from the retrograde to the antegrade guiding catheter. We believe that this stepwise approach would lead to a CTO procedure with a very high probability of success.
In recent years, the hybrid algorithm has been shown to be the most effective way to recanalise a CTO, with a success rate >90%2. This algorithm should be the first choice for complex CTO interventions in case of lesions with a high J-CTO score such as the one presented by Debski and colleagues.
Conflict of interest statement
The author has no conflicts of interest to declare.
How did I treat?
ACTUAL TREATMENT AND MANAGEMENT OF THE CASE
Using bilateral femoral access, both the left coronary artery and the ostial SVG CTO were cannulated with an EBU 4.5 and an AR 2.0 guide catheter, respectively. The SVG CTO was penetrated retrogradely via the septal artery (Figure 3), using a Fielder FC with the support of a FineCross microcatheter (Terumo Corp.). Having placed the crossing wire retrogradely within the SVG guide catheter and stabilised with an inflated balloon, it was possible to penetrate the CTO lesion with the FineCross microcatheter. Afterwards, the wire was exchanged for a 300 cm RG3 wire (ASAHI Intecc) in order to execute the externalisation of the retrograde guidewire. Next, SVG predilatation with a 1.5 mm OTW balloon and subsequently with upgraded balloons was performed. Finally, four 3.0 mm and 3.5 mm biolimus-eluting stents were deployed at 20 atm into the SVG. A good angiographic result was achieved with TIMI 3 flow (Figure 4). As no sufficient landing zone was available for the FilterWire (Boston Scientific) in the distal RCA, it was not used. The total contrast amount used was 300 ml and the fluoroscopy time was 72 min. No periprocedural complications were observed. The post-procedural troponin T rise was 168 ng/L (UNL 14). Computed tomography angiography performed after two months revealed a patent SVG. During one year of follow-up, the patient remains in class I according to CCS.
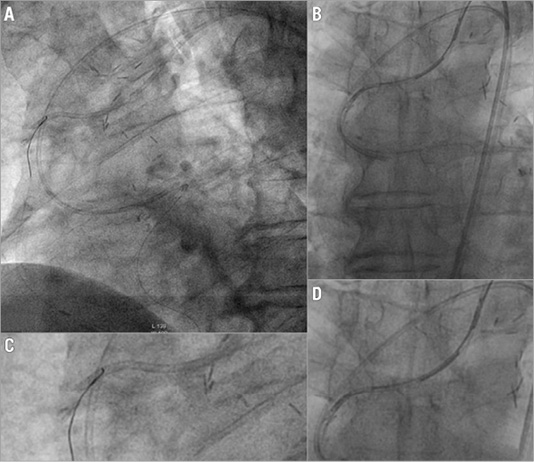
Figure 3. Retrograde opening of the chronically occluded saphenous vein graft. A) Retrograde passage of the crossing wire into the guide catheter to the saphenous vein graft. B) Magnification of panel A. C) Stabilisation of the retrograde wire within the catheter with an inflated balloon. D) Magnification of panel C.
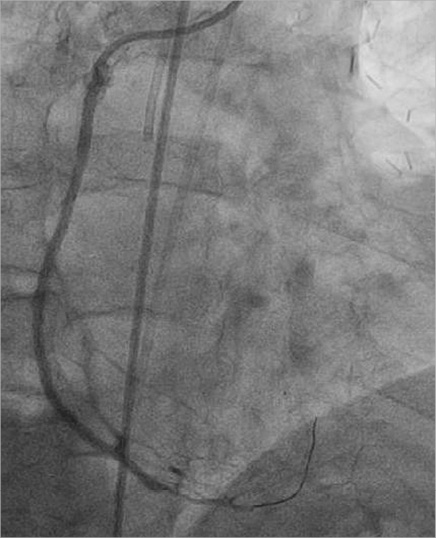
Figure 4. Final angiographic result.
Discussion
As stated in recently published 2014 ESC guidelines on myocardial revascularisation, percutaneous coronary intervention (PCI) of CTO of native coronaries should be considered for ischaemia reduction and/or angina relief. However, the retrograde approach has only class IIb indications3. Secondly, SVG PCI is considered a high-risk procedure due to acute distal embolisation and poorer long-term results. Additionally, when SVG CTO is the case, it makes the PCI much more challenging. The 2011 ACCF/AHA/SCAI PCI guidelines discourage such an approach (class IIIB indications). In a retrospective study, the success rate of SVG CTO opening was reported at 79%4. However, one must bear in mind the selection bias. Further, in a small group comparing the outcome after successful PCI of SVG CTO versus PCI of native coronary CTO, the cumulative three-year event-free survival was similar in both groups5.
Several techniques have been developed for retrograde attempts to open CTO of native coronaries6. However, such an approach for SVG CTO has extremely little evidence. To the best of our knowledge, only two cases of successful retrograde SVG CTO recanalisation from one centre have been reported so far7,8. One of these cases was carried out via the epicardial artery. However, as the septal collateral channels are safer, they should be preferred over the epicardial collaterals whenever possible, although they frequently occlude after the procedure.
Finally, by their nature such procedures are associated with long fluoroscopy time and not a small contrast amount. Very careful patient preparation is obligatory to avoid contrast-induced nephropathy.
Conclusion
In very selected patients such an approach may be an option when other revascularisation options have failed or were not feasible.
Conflict of interest statement
The authors have no conflicts of interest to declare.