Abstract
BACKGROUND: Percutaneous coronary interventions (PCI) of chronic total occlusions (CTO) have reached high procedural success rates thanks to dedicated equipment, evolving techniques, and worldwide adoption of state-of-the-art crossing algorithms.
AIMS: We report the contemporary results of CTO PCIs performed by a large European community of experienced interventionalists. Furthermore, we investigated the impact of different risk factors for procedural major adverse cardiac and cerebrovascular events (MACCE) and trends of employment of specific devices like dual lumen microcatheters, guiding catheter extensions, intravascular ultrasound and calcium-modifying tools.
METHODS: We evaluated data from 8,673 CTO PCIs included in the European Registry of Chronic Total Occlusion (ERCTO) between January 2021 and October 2022.
RESULTS: The overall technical success rate was 89.1% and was higher in antegrade as compared with retrograde cases (92.8% vs 79.3%; p<0.001). Compared with antegrade procedures, retrograde procedures had a higher complexity of attempted lesions (Japanese CTO [J-CTO] score: 3.0±1.0 vs 1.9±1.2; p<0.001), a higher procedural and in-hospital MACCE rate (3.1% vs 1.2%; p<0.018) and a higher perforation rate with and without tamponade (1.5% vs 0.4% and 8.3% vs 2.1%, respectively; p<0.001). As compared with mid-volume operators, high-volume operators had a higher technical success rate in antegrade and retrograde procedures (93.4% vs 91.2% and 81.5% vs 69.0%, respectively; p<0.001), and had a lower MACCE rate (1.47% vs 2.41%; p<0.001) despite a higher mean complexity of the attempted lesions (J-CTO score: 2.42±1.28 vs 2.15±1.27; p<0.001).
CONCLUSIONS: The adoption of different recanalisation techniques, operator experience and the use of specific devices have contributed to a high procedural success rate despite the high complexity of the lesions documented in the ERCTO.
Coronary chronic total occlusions (CTOs) are found in about 20% of patients undergoing coronary angiography, and this prevalence increases up to 40% in diabetic or heart failure patients123. Over the past two decades, the improvement of operator skill, the optimisation of recanalisation techniques and the development of new dedicated devices for CTO percutaneous coronary intervention (PCI) have contributed to greatly increasing the procedural success that is nowadays in a range close to 90%456. However, such procedures still have a non-negligible incidence of specific procedural complications (e.g., collateral perforations and access site vascular complications, especially when a dual arterial access with a large-bore sheath is adopted) as compared with non-CTO PCI; this aspect must be taken into account at the time of evaluating procedural benefits and risks7. Moreover, a proper assessment of the procedural risks and benefits is essential for patient counselling and procedural planning.
The aim of our study is to report the contemporary procedural technical success and complication rates of the European Registry of Chronic Total Occlusion (ERCTO) in light of the latest state-of-the-art reviews and expert consensus documents about dedicated devices such as guiding catheter extensions (GCEs), dual lumen microcatheters (DLMs), intravascular ultrasound (IVUS) catheters or other dedicated calcified plaque modification devices (CPMDs)89101112.
Methods
We examined 8,673 CTO PCIs included in the ERCTO between January 2021 and October 2022. The ERCTO is an electronically based registry developed by the non-profit organisation Euro CTO to collect data from patients undergoing CTO PCI, treated by 89 expert operators at referral centres across Europe (www.ercto.org). According to their credentials, 53 operators were classified as high-volume operators (HVOs) with more than 300 documented and certified entries in the ERCTO and a minimum number of 50 CTO PCIs per year as first operator. The remaining 36 operators, despite being named “CTO expert operators”, were designated mid-volume operators (MVOs) since they had not received “HVO” status yet. The mean MVO’s annual procedural volume was 27.3 (standard deviation [SD]=17.0). All patients were selected based on the presence of symptoms, viability, and significant inducible ischaemia in the CTO artery territory, as demonstrated by functional imaging tests. Among asymptomatic patients, CTO PCI indication was based on the presence of a large area of inducible ischaemia and significant viability in those patients with reduced left ventricular ejection fraction. The sequence of use of wiring techniques and guidewire selection were left entirely to the operator’s discretion. All patients signed the informed consent form for a CTO PCI procedure. The documentation of patient data was anonymised and managed according to the data safety protocols of the participating centres. The study was approved by the institutional review board of each centre and performed in accordance with the Declaration of Helsinki.
Definitions
CTO Academic Research Consortium definitions were adopted13. Accordingly, CTOs were defined as the absence of antegrade flow through the lesion with a presumed or documented duration of >3 months and Thrombolysis In Myocardial Infarction (TIMI) flow grade 0. Lesion crossing strategies were the following: the antegrade approach was defined as advancing from the proximal CTO cap to cross the distal CTO cap in order to access the distal true lumen. The retrograde approach was defined as a wire-based technique with the intention of crossing the distal CTO cap to the proximal CTO to access the proximal true lumen. Each approach is then different in wiring: either the CTO is intentionally crossed from proximal vessel true lumen, through the CTO body, to the distal vessel true lumen; or there is dissection re-entry if the CTO is intentionally crossed from the proximal vessel lumen through a dissection plane, followed by re-entry into the distal vessel lumen at or beyond the distal cap of the occlusion, named, respectively, antegrade dissection re-entry (ADR) and retrograde dissection re-entry (RDR). Furthermore, those antegrade cases with retrograde contribution have been defined as “retrograde”. Technical success was defined as the successful recanalisation of the CTO vessel with <30% residual stenosis and final TIMI flow grade 3. Bifurcations were defined by the presence of a side branch diameter of >2 mm within 5 mm of the proximal or distal cap of the CTO lesion.
Procedural success was defined as technical success in the absence of in-hospital major adverse cardiac and cerebrovascular events (MACCE). MACCE were defined as the composite of death, myocardial infarction (MI), stroke, urgent repeat revascularisation (re-PCI or surgery), or pericardiocentesis. MI was defined using the Fourth Universal Definition of Myocardial Infarction14. CTO calcifications, assessed semiquantitatively by angiography, were classified as mild (spots), moderate (radiopaque densities noted during the cardiac cycle involving only one side of the vascular wall) and severe (radiopaque densities noted without cardiac motion before contrast injection, generally involving both sides of the arterial wall).
Statistical analysis
Continuous variables were presented as mean±SD or median and interquartile range [IQR], while categorical variables were presented as counts and percentages. To assess the statistical significance, the Chi-squared test was used for categorical variables (or Fisher’s exact test when necessary) and the t-test for continuous variables. Furthermore, a logistic regression model, adjusted for clinical, procedural and lesion characteristics, was used to verify the odds ratio for procedural complication occurrence of different clinical and procedural variables. The statistically significant variables in univariable analysis were added in multivariable analysis, and the results were expressed as adjusted odds ratios (adjORs) and 95% confidence intervals (CIs). A two-sided p-value of less than 0.05 was considered to indicate statistical significance. All data were processed using R software, version 4.1.2 (R Foundation for Statistical Computing).
Results
POPULATION CHARACTERISTICS
Baseline patient characteristics are shown in Table 1. Most of the patients were male (82.8%); the mean age was 65.5±10.4 years. One-third of patients had a previous MI and 10.1% a previous MI in the CTO territory; 11.8% had a previous coronary artery bypass graft (CABG). Furthermore, 17.8% complained of stable angina with a Canadian Cardiovascular Society (CCS) grading >2, and 52.4% complained of dyspnoea, assessed by New York Heart Association (NYHA) Class >1. Seventy-eight percent of patients were taking 1 antianginal drug, 19% ≥2, while 3% did not take any antianginal drugs (Central illustration). Moreover, 7.6% had a severely reduced left ventricular ejection fraction (<35%), while 52% had segmental wall motion abnormalities in the CTO territory. Most of the patients (81%) underwent a functional test before CTO PCI, either for the assessment of inducible ischaemia or viability. Ninety percent of patients with akinesia or dyskinesia in the CTO territory underwent a non-invasive imaging test to assess viability by either single positron emission computed tomography (SPECT), positron emission tomography (PET) or magnetic resonance imaging (MRI).
Table 1. Clinical characteristics.
| OverallN=8,673 | AntegradeN=6,282 | RetrogradeN=2,391 | p-value | |
|---|---|---|---|---|
| Age, years | 65.5±10.4 | 65.6±10.6 | 65.1±10.1 | 0.018 |
| Male | 7,183 (82.8) | 5,088 (81) | 2,095 (87.6) | <0.001 |
| Hypertension | 6,548 (75.5) | 4,670 (74.3) | 1,878 (78.5) | <0.001 |
| Dyslipidaemia | 6,285 (72.5) | 4,463 (71) | 1,822 (76.2) | <0.001 |
| Diabetes mellitus overall | 2,682 (30.9) | 1,902 (30.3) | 780 (32.7) | 0.037 |
| Diabetes mellitus ID | 463 (5.3) | 337 (5.4) | 126 (5.3) | 0.902 |
| Smoker | 1,951 (22.5) | 1,367 (21.8) | 584 (24.4) | 0.008 |
| Previous MI | 2,876 (33.2) | 2,015 (32.1) | 861 (36) | <0.001 |
| MI in CTO territory | 881 (10.1) | 623 (9.9) | 258 (10.8) | 0.342 |
| Prior stroke | 307 (3.5) | 212 (3.4) | 95 (4) | 0.199 |
| Previous CABG | 1,027 (11.8) | 612 (9.7) | 415 (17.4) | <0.001 |
| Previous PCI | 4,482 (51.7) | 3,139 (50) | 1,343 (56.2) | <0.001 |
| Atrial fibrillation | 401 (4.6) | 293 (4.7) | 108 (4.5) | 0.151 |
| eGFR, ml/min | 73.4±300.0 | 75.3±352.2 | 68.5±28.6 | 0.128 |
| Impaired LVEF | ||||
| 35%<LVEF<50% | 1,966 (22.7) | 1,366 (21.7) | 600 (25.1) | 0.016 |
| LVEF <35% | 656 (7.6) | 502 (8) | 154 (6.4) | 0.063 |
| Wall motion abnormality in CTO territory | 4,516 (52.1) | 3,272 (52.1) | 1,244 (52) | 0.981 |
| Clinical presentation | ||||
| Asymptomatic | 1,401 (16.2) | 999 (15.9) | 402 (16.8) | <0.001 |
| Stable angina | 6,443 (74.3) | 4,628 (73.7) | 1,815 (75.9) | <0.001 |
| Unstable angina | 408 (4.7) | 319 (5.1) | 89 (3.7) | <0.001 |
| MI | 244 (2.8) | 191 (3) | 53 (2.2) | 0.723 |
| CCS >2 | 1,545 (17.8) | 1,330 (21.1) | 215 (9) | <0.001 |
| NYHA >1 | 4,594 (52.4) | 3,814 (60.7) | 781 (32.6) | 0.030 |
| Functional tests for ischaemia and viability assessment | 7,025 (81) | 4,962 (79) | 2,063 (86) | 0.006 |
| Exercise ECG | 1,734 (20) | 1,256 (19.9) | 478 (20) | 0.521 |
| Stress echocardiography | 3,122 (36) | 2,259 (35.9) | 863 (36.1) | 0.321 |
| SPECT | 1,125 (13) | 737 (11.7) | 388 (16.2) | <0.001 |
| MRI | 948 (10.9) | 658 (10.5) | 290 (12.1) | 0.072 |
| PET | 51 (0.6) | 36 (0.6) | 15 (0.6) | 0.125 |
| No. of diseased vessels | ||||
| 1 vessel | 3,109 (35.8) | 2,288 (36.4) | 821 (34.3) | <0.001 |
| 2 vessels | 2,555 (29.5) | 1,882 (30) | 673 (28.1) | <0.001 |
| 3 vessels | 2,809 (32.4) | 1,932 (30.8) | 877 (36.7) | <0.001 |
| Data are expressed as mean±SD and n (%). CABG: coronary artery bypass grafting; CCS: Canadian Cardiovascular Society; CTO: chronic total occlusion; ECG: electrocardiogram; eGFR: estimated glomerular filtration rate; ID: insulin dependent; LVEF: left ventricular ejection fraction; MI: myocardial infarction; MRI: magnetic resonance imaging; NYHA: New York Heart Association; PCI: percutaneous coronary intervention; PET: positron emission tomography; SD: standard deviation; SPECT: single positron emission computed tomography | ||||
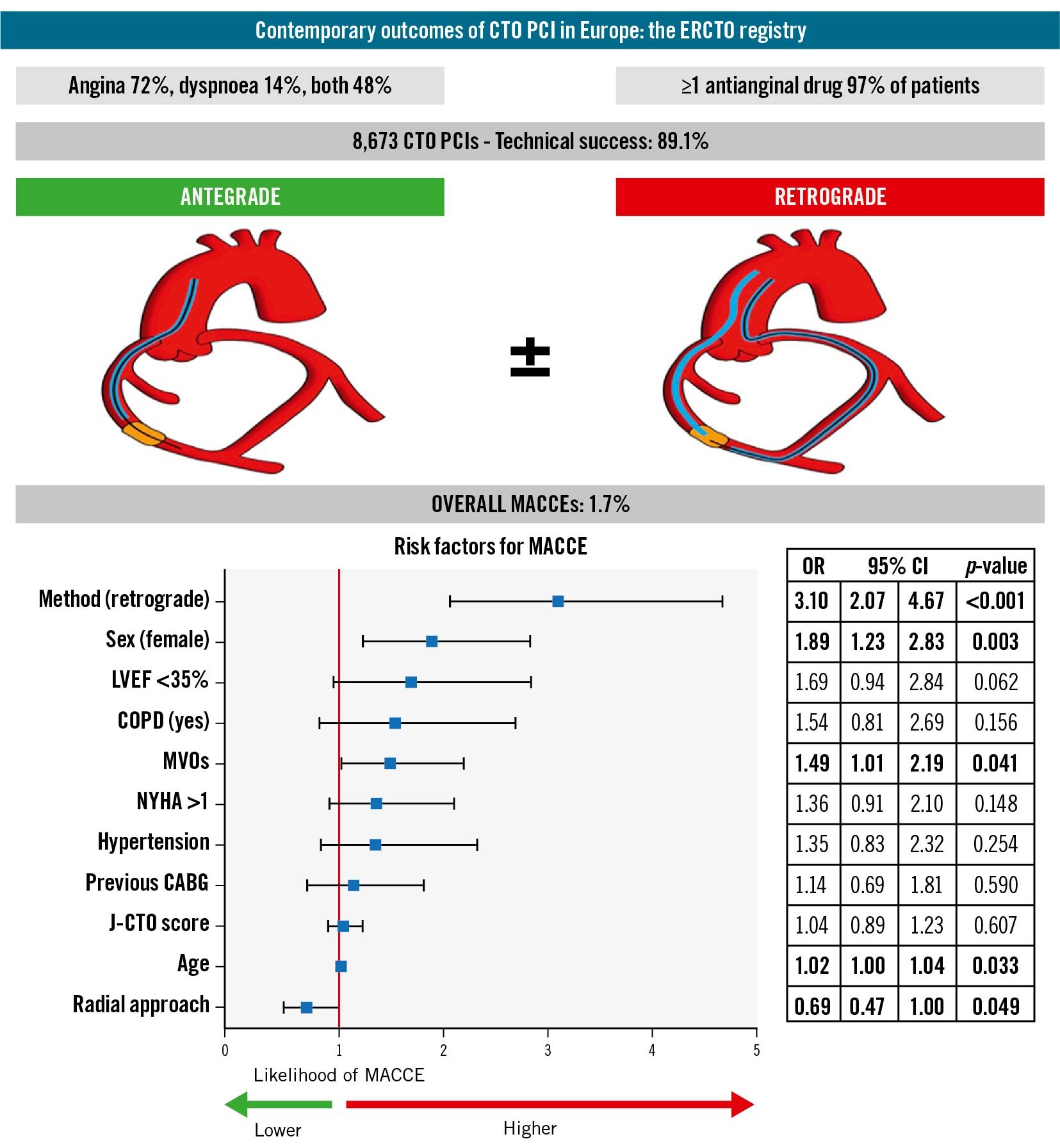
Central illustration. Main findings of contemporary CTO PCI in the ERCTO registry. The logistic regression model shows the impact of different risk factors for procedural and in-hospital MACCE. CABG: coronary artery bypass grafting; CI: confidence interval; COPD: chronic obstructive pulmonary disease; CTO: chronic total occlusion; ERCTO: European Registry of Chronic Total Occlusion; LVEF: left ventricular ejection fraction; MACCE: major adverse cardiac and cerebrovascular events; MVO: mid-volume operator; J-CTO score: Japanese CTO score; NYHA: New York Heart Association; PCI: percutaneous coronary intervention; OR: odds ratio
LESION CHARACTERISTICS
Lesion characteristics are listed in Table 2. The right coronary artery (RCA) was the most frequent target vessel (55.9%), followed by the left anterior descending artery (LAD; 26.4%) and the left circumflex artery (LCx; 14.9%). The mean lesion complexity as assessed by the Japanese CTO (J-CTO) score was 2.2±1.3; the mean lesion length was 27.1±16.9 mm. A bifurcation involvement was reported in one-third of lesions. Retrograde procedures had a significantly higher mean J-CTO score than antegrade procedures (3.0±1.0 vs 1.9±1.2; p<0.001).
Table 2. Lesion characteristics.
| OverallN=8,673 | AntegradeN=6,282 (73) | RetrogradeN=2,391 (27) | p-value | ||
|---|---|---|---|---|---|
| Target vessel | LAD | 2,412 (27.8) | 1,801 (28.7) | 611 (25.5) | 0.036 |
| LCx | 1,309 (15.1) | 1,142 (18.2) | 167 (7.0) | <0.001 | |
| RCA | 4,904 (56.6) | 3,307 (52.7) | 1,597 (66.8) | <0.001 | |
| IMA | 4 (0) | 4 (0.1) | 0 (0) | - | |
| SVG | 11 (0.1) | 9 (0.1) | 2 (0.1) | - | |
| LM | 32 (0.4) | 19 (0.3) | 13 (0.5) | 0.312 | |
| CTO location | ostial | 903 (10.4) | 479 (7.6) | 424 (17.7) | <0.001 |
| proximal | 3,249 (37.5) | 2,259 (36) | 990 (41.4) | <0.001 | |
| middle | 3,753 (43.3) | 2,901 (46.2) | 852 (35.6) | <0.001 | |
| distal | 767 (8.8) | 642 (10.2) | 125 (5.2) | <0.001 | |
| Bifurcation | 2,778 (32) | 1,903 (30.3) | 875 (36.6) | <0.001 | |
| SB within CTO | 784 (28.2) | 551(28.9) | 233 (26.6) | <0.001 | |
| SB proximal to CTO | 891 (32.1) | 658 (34.5) | 233 (26.6) | <0.001 | |
| SB distal to CTO | 978 (35.2) | 621 (32.6) | 357 (40.8) | <0.001 | |
| J-CTO score | 2.2±1.3 | 1.9±1.2 | 3.0±1.0 | <0.001 | |
| Mean lesion length, mm | 27.1±16.9 | 23.6±14.8 | 36.1±18.8 | <0.001 | |
| CTO diameter, mm | 3.0±1.2 | 2.9±1.4 | 3.2±0.7 | <0.001 | |
| Lesion length >20 mm | 4,772 (55.1) | 2,888 (46) | 1,884 (78.8) | <0.001 | |
| Stump | tapered | 3,633 (41.9) | 3,166 (50.4) | 467 (19.5) | <0.001 |
| blunt | 3,393 (39.1) | 2,162 (34.4) | 1,231 (51.5) | <0.001 | |
| Tortuosity (severe) | 227 (2.6) | 142 (2.3) | 85 (3.6) | <0.001 | |
| Previous attempt ≥1 | 1,885 (21.8) | 1,154 (18.4) | 731 (30.7) | <0.001 | |
| CC ≥2 | 7,776 (89.7) | 5,497 (87.5) | 2,279 (95.3) | <0.001 | |
| Heavy calcification | 1,606 (18.5) | 937 (14.9) | 669 (28) | <0.001 | |
| In-stent CTO | 805 (9.3) | 645 (10.3) | 160 (6.7) | <0.001 | |
| Data are expressed as mean±SD and n (%). CC: collateral channel grade; CTO: chronic total occlusion; IMA: inferior mesenteric artery; J-CTO: Japanese CTO score; LAD: left anterior descending artery; LCx: left circumflex artery; LM: left main; RCA: right coronary artery; SB: side branch; SD: standard deviation; SVG: saphenous vein graft | |||||
PROCEDURAL CHARACTERISTICS
Table 3 shows in detail the procedural characteristics. Out of 8,673 procedures, 73% were antegrade, while the remaining 27% were retrograde. Among antegrade procedures, ADR techniques were employed in 6% of cases, while among retrograde procedures, RDR techniques were adopted in 44% of cases. Overall technical success was 89.1% and was significantly higher for the antegrade approach, as compared with retrograde (92.8% vs 79.3%; p<0.001). Dual arterial access was utilised in 75.8% of procedures. Out of these, a combined transradial (TR) and transfemoral (TF) approach was adopted in 33.9% of cases, while a dual TR or dual TF approach was employed in 25.8% and 16.1% of cases, respectively. Bifurcation stenting was performed in 26.1% of procedures, by a single-stent technique in 82% of cases and by a double-stent technique in the remaining 18%. A mechanical support device was employed in 36 procedures (0.4%); in all but 4 cases, the devices were placed prophylactically before CTO PCI. As compared with antegrade, the retrograde approach showed a significantly higher total stented length (65.8±44.6 mm vs 54.5±34.1 mm; p<0.001), higher total procedural time (140 min [IQR 106.8-180.0] vs 70 min [IQR 49-103]; p<0.001), higher fluoroscopy time (61 min [IQR 44-85] vs 25 min [IQR 15.0-39.7]; p<0.001), and higher contrast volume (250 ml [IQR 180-350] vs 180 ml [IQR 120-250]; p<0.001).
Table 3. Procedural characteristics.
| OverallN=8,673 | AntegradeN=6,282 (73) | RetrogradeN=2,391 (27) | p-value | |
|---|---|---|---|---|
| Technical success | 7,727 (89.1) | 5,832 (92.8) | 1,895 (79.3) | <0.001 |
| Arterial access | ||||
| Dual | 6,573 (75.8) | 4,182 (66.6) | 2,391 (100) | <0.001 |
| TFA/TFA | 1,399 (16.1) | 887 (14.1) | 512 (21.4) | <0.001 |
| TRA/TRA | 2,235 (25.8) | 1,818 (28.9) | 417 (17.4) | <0.001 |
| TFA/TRA | 2,939 (33.9) | 1,477 (23.6) | 1,462 (61.2) | <0.001 |
| Single | 2,100 (24.2) | 2,100 (33.4) | - | - |
| TFA | 712 (8.1) | 849 (13.5) | - | - |
| TRA | 1,388 (13) | 1,251 (19.9) | - | - |
| Target vessel | ||||
| TFA as target vessel | 4,212 (48.6) | 2,967 (47.2) | 1,244 (52) | <0.001 |
| TRA as target vessel | 4,461 (51.4) | 3,314 (52.8) | 1,147 (48) | <0.001 |
| Target vessel sheath size | ||||
| 6 Fr | 2,081 (24) | 1,679 (26.7) | 402 (16.8) | <0.001 |
| 7 Fr | 5,907 (68.1) | 4,122 (65.6) | 1,785 (74.7) | <0.001 |
| 8 Fr | 387 (4.5) | 217 (3.5) | 170 (7.1) | <0.001 |
| TFA target vessel ≥7 Fr | 3,515 (41) | 2,398 (38) | 1,117 (47) | <0.001 |
| TRA target vessel ≥7 Fr | 2,768 (32) | 1,932 (31) | 836 (35) | <0.001 |
| Dedicated devices | ||||
| Dual lumen microcatheter | 1,021 (11.8) | 642 (10.2) | 379 (15.8) | <0.001 |
| Guiding catheter extension | 1,633 (18.8) | 795 (12.6) | 838 (35) | <0.001 |
| IVUS-assisted procedure | 1,844 (21.3) | 1,207 (19.2) | 637 (26.6) | <0.001 |
| Rotational atherectomy | 297 (3.4) | 233 (3.7) | 64 (2.7) | 0.056 |
| Orbital atherectomy | 8 (0.1) | 7 (0.1) | 1 (0) | 0.088 |
| Intravascular lithotripsy | 95 (1.1) | 66 (1.1) | 29 (1.2) | 0.100 |
| Stent metrics | ||||
| Number of implanted stents | 2.0±1.3 | 1.9±1.2 | 2.2±1.5 | <0.001 |
| Max stent diameter, mm | 2.8±1.6 | 2.9±1.5 | 2.7±1.9 | <0.001 |
| Total stented length, mm | 57.6±37.6 | 54.5±34.1 | 65.8±44.6 | <0.001 |
| Bifurcation stenting | 2,263 (26.1) | 1,626 (25.8) | 637 (26.6) | 0.324 |
| Single stenting technique | 1,850 (21.3) | 1,342 (21.3) | 508 (21.2) | 0.421 |
| Double stenting technique | 413 (4.8) | 309 (4.9) | 104 (4.3) | <0.001 |
| LV mechanical support | ||||
| IABP | 7 (0.1) | 4 (0.1) | 3 (0.1) | - |
| Impella (Abiomed) | 27 (0.3) | 22 (0.4) | 5 (0.2) | 0.041 |
| ECMO | 2 (0) | 2 (0) | 0 (0) | - |
| Procedural metrics | ||||
| Total procedural time, min | 96 [74-182] | 70 [49-103] | 140 [106.8-180.0] | <0.001 |
| Total fluoroscopic time, min | 41 [23-82] | 25 [15.0-39.7] | 61 [44-85] | <0.001 |
| Total contrast volume, ml | 212.2±128.1 | 180 [120-250] | 250 [180-350] | <0.001 |
| Data are expressed as mean±SD, interquartile ranges [IQR] and n (%). ECMO: extracorporeal membrane oxygenation; IABP: intra-aortic balloon pump; IQR: interquartile range; IVUS: intravascular ultrasound; LV: left ventricle; SD: standard deviation; TFA: transfemoral access; TRA: transradial access | ||||
TECHNOLOGY APPLIED TO PROCEDURE
The type of wires used to start and to terminate the procedure and the microcatheters used in antegrade and retrograde approaches are depicted in Supplementary Figure 1.
A soft polymeric wire was used as the initial wire in 57% of the procedures, while in the remaining cases, a hydrophilic wire with various tip loads was used. Conversely, the wire that finally crossed the CTO was a hydrophilic one in 58% of the procedures. Among the different types of polymeric and hydrophilic wires, the Fielder and Gaia family wires (Asahi Intecc) were most frequently used. Furthermore, the Gaia series wires were those that, in most of the cases, finally crossed the CTO lesion.
A microcatheter was used in 98% of overall procedures; more than one microcatheter was required in a significantly higher proportion of retrograde than antegrade procedures (50.2% vs 15.9%; p<0.001).
Figure 1 depicts the use of dedicated devices such as GCEs, DLMs, IVUS catheters and CPMDs. IVUS was performed within a guiding catheter ≤7 Fr in 93% of cases (12%: 6 Fr; 81%: 7 Fr; 7%: 8 Fr). Out of 1,606 lesions classified as heavily calcified, a CPMD was used in 383 procedures (24%). The Rotablator (Boston Scientific) was employed in 75% of such procedures, followed by the Intravascular Lithotripsy System (Shockwave Medical) and Diamondback 360 Orbital Atherectomy System (Abbott) used in 23% and 2% of cases, respectively. After successful CTO lesion wire crossing, despite the high lesion complexity of such complex procedures (mean J-CTO score 2.78±1.05), technical success was achieved in 97.4% of procedures.
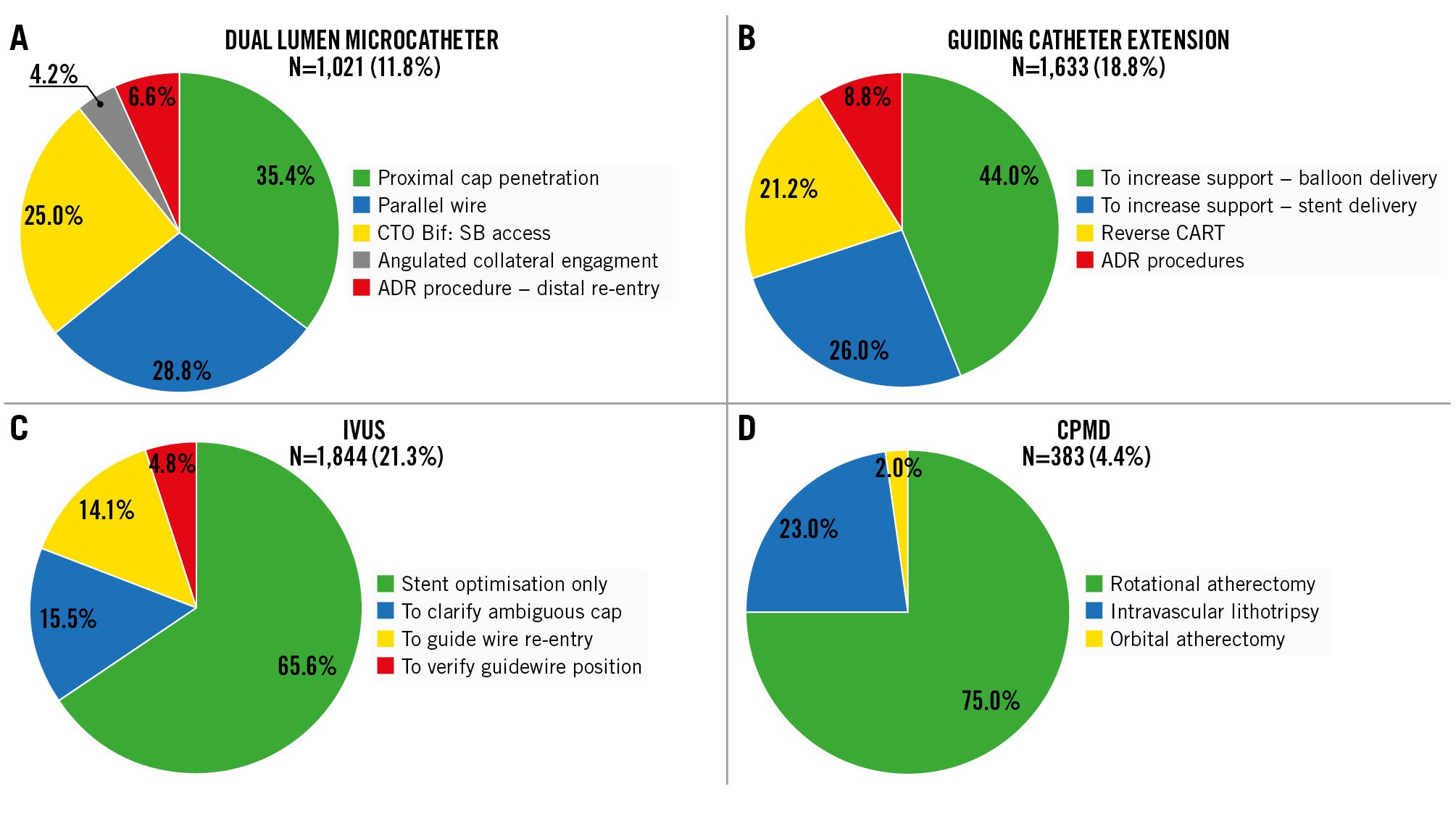
Figure 1. Different settings of the employment of dedicated devices for CTO PCI. A) Dual lumen microcatheter, B) catheter extension, C) intravascular ultrasound, and D) calcified plaque modification device. ADR: antegrade dissection and re-entry; Bif: bifurcation; CART: controlled antegrade and retrograde tracking; CPMD: calcified plaque modification device; CTO: chronic total occlusion; IVUS: intravascular ultrasound; SB: side branch
PROCEDURAL AND IN-HOSPITAL COMPLICATIONS
Figure 2 and Supplementary Table 1 describe procedural complications and in-hospital outcomes. MACCE occurred in 147 procedures (1.7%), driven mostly by perforations with tamponade (0.7%), periprocedural MIs (0.5%), and deaths (0.3%). Coronary perforations occurred in 3.8% of procedures; 0.7% of perforations involved coronary collaterals. Overall cardiac tamponade was observed in 0.4% of all procedures. As compared with antegrade, the retrograde approach showed significantly higher rates of MACCE (3.1% vs 1.2%; p=0.018), mortality (0.4% vs 0.3%; p=0.023), overall perforation rate (8.3% vs 2.1%; p<0.001), perforation with tamponade (1.5% vs 0.3%; p=0.009) and major vascular complications (1.5% vs 0.5%; p<0.001). Among retrograde procedures, a primary retrograde approach was employed in 41.5% of cases; in the remaining 58.5%, the retrograde approach was used in combination with one or more antegrade techniques. As compared with the primary antegrade procedures, in cases where the retrograde approach was used alone or in combination with antegrade techniques, MACCE rates and overall perforation rates were higher (1.2% vs 2.5% vs 3.5%; p<0.001; 2.1% vs 7.7% vs 8.7%; p<0.001). Vascular complications occurred more frequently in procedures with at least one TF access, as compared with those performed without any TF access (1.2% vs 0.3%; p<0.001), and more frequently in cases performed by a guiding catheter ≥7 Fr in size as compared to those with 6 Fr (1.0% vs 0.4%; p<0.001). Relevant side branch occlusion occurred in 1.3% of procedures. The logistic regression analysis (Central illustration) identified the retrograde approach (odds ratio [OR] 1.89, 95% confidence interval [CI]: 1.23-2.83; p=0.003), female sex (OR 1.89, 95% CI: 1.23-2.83; p=0.003), age (OR 1.02, 95% CI: 1.00-1.04; p=0.033), and the operator’s MVO status (OR 1.49, 95% CI: 1.01-2.19; p=0.041) as independent risk factors of procedural and in-hospital MACCE; conversely, the radial approach showed a reduced risk of events (OR 0.69, 95% CI: 0.47-1.00; p=0.049).
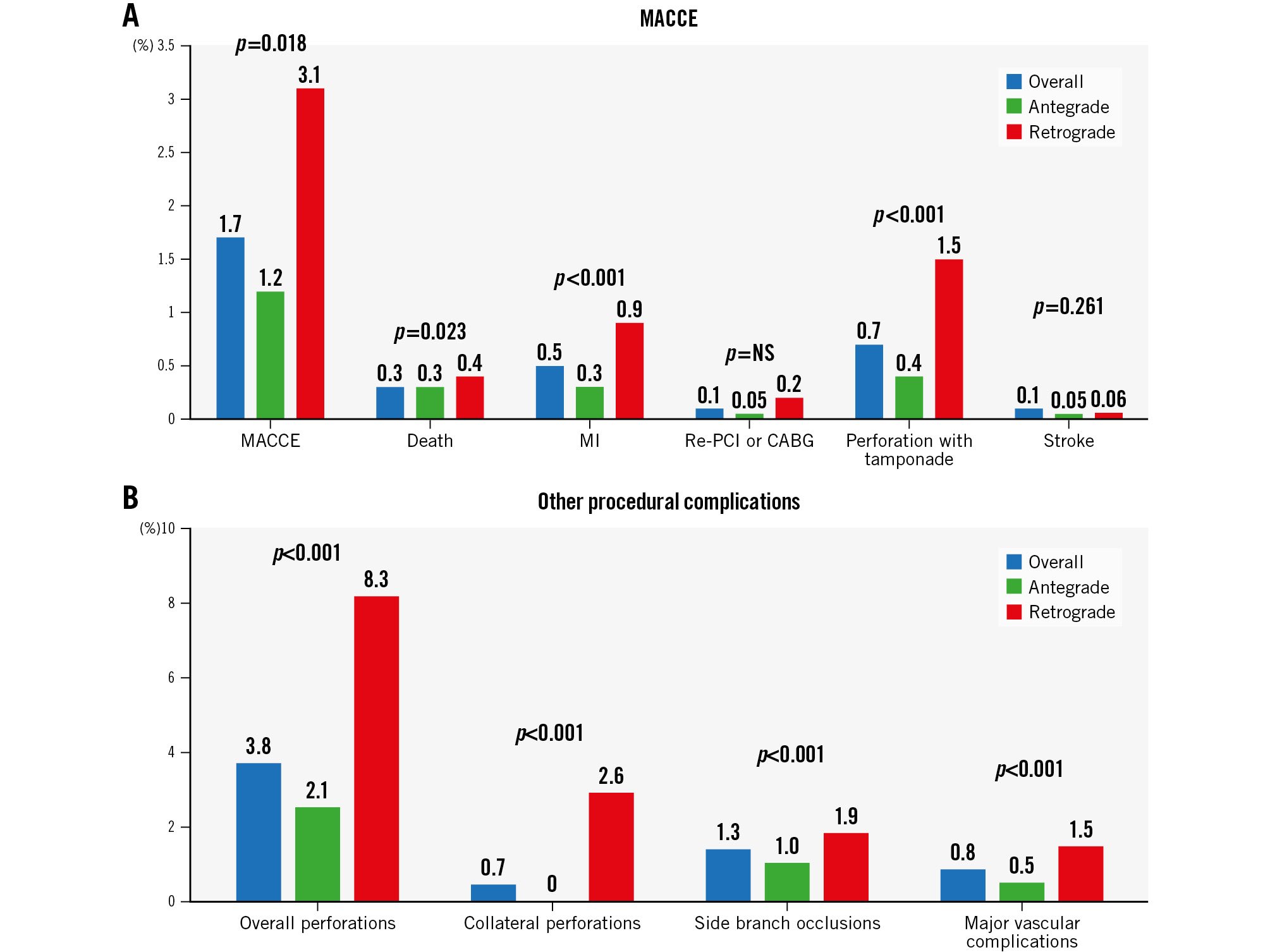
Figure 2. Procedural and in-hospital complications. A) MACCE and B) other procedural complications. CABG: coronary artery bypass grafting; MACCE: major adverse cardiac and cerebrovascular events; MI: myocardial infarction; NS: non-significant; PCI: percutaneous coronary intervention
PROCEDURAL PERFORMANCE ACCORDING TO OPERATOR EXPERTISE
Supplementary Table 2 shows the most important features of procedures performed by HVOs and MVOs. As compared with MVOs, HVOs performed a higher number of procedures with dual arterial access (78.5% vs 67.1%; p<0.001) and with dual TRA access (27.8% vs 19.1%; p<0.001); HVOs attempted more complex CTO lesions (J-CTO score: 2.42±1.28 vs 2.15±1.27; p<0.001), performed more retrograde procedures (29.7% vs 20.7%; p<0.001), and achieved higher technical success rates (89.9% vs 86.6%; p<0.01), in both antegrade (93.4% vs 91.2%; p<0.001) and retrograde approaches (81.5% vs 69.0%; p<0.001).
HVOs had a significantly lower MACCE rate (1.47% vs 2.41%; p<0.001), mortality (0.18% vs 0.72%; p<0.001) and overall perforation rate (3.5% vs 4.7%; p<0.001); however, the number of perforations with tamponade did not differ between the two groups (0.8% vs 0.5%; p=0.294) (Figure 3).
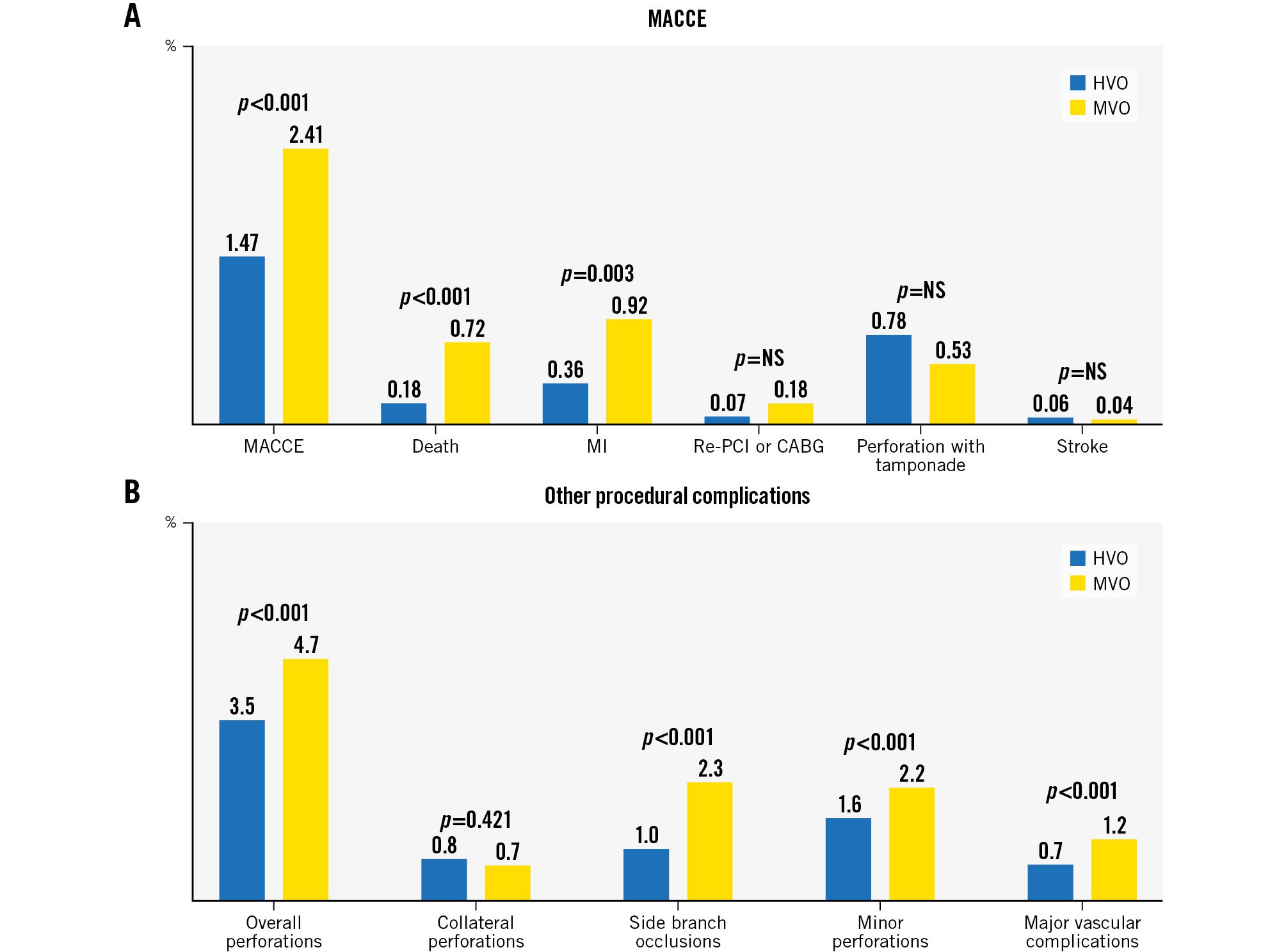
Figure 3. Procedural and in-hospital complications according to operator expertise. A) MACCE and B) other procedural complications. CABG: coronary artery bypass grafting; HVO: high-volume operator; MACCE: major adverse cardiac and cerebrovascular events; MI: myocardial infarction; MVO: mid-volume operator; NS: non-significant; PCI: percutaneous coronary intervention
Discussion
The main findings of the study are the following: 1) contemporary ERCTO CTO PCI success rates are comparable to the US and Japanese updated registries; 2) the retrograde approach was performed in more complex lesions but also had higher complication rates as compared with antegrade procedures; 3) operator expertise was shown to be a key factor for procedural success; and 4) dedicated devices for CTO PCI are essential to facilitate these complex procedures.
TECHNICAL SUCCESS AND COMPLICATIONS
In the last decade, the CTO PCI procedural success rate has increased, at least in part, thanks to the widespread adoption of state-of-the-art techniques for CTO PCI15. Furthermore, major adverse cardiac event rates have remained stable worldwide despite the overall lesion complexity of CTO PCI having increased12. However, the complication rate for this procedure is still higher than for non-CTO PCI716. In this regard, safety concerns around these procedures have been raised in the international guidelines on myocardial revascularisation1718.
The current ERCTO technical success rate is 89.2%, achieved at the cost of 1.7% MACCE, 3.8% overall perforations and 0.4% coronary perforations with tamponade. In the previous ERCTO report from Konstantinidis et al, referring to the period from 2008 to 2015, the procedural success rate increased significantly from 79.7% to 89.3%, while the MACCE rate remained steady at 1%. Moreover, the coronary perforation rate increased from 2.5% to 3.2%. The authors explained this trend by the concomitant increasing complexity of lesions attempted during the study period (J-CTO score: 1.76±1.03 in 2008 vs 2.17±0.91 in 2015; p for trend<0.001)6. Similarly, Werner et al, in the EuroCTO randomised controlled trial, showed a technical success rate of 86.6% and in-hospital complication rate of 2.9%19. Data from US studies showed a technical success rate ranging between 86.0% and 91.5%, while in-hospital major complications ranged between 1.8% and 7.0%5202122, whereas an Asian study reported a technical success rate in the range of 89.9-90.1% and an incidence of in-hospital major adverse cardiovascular events (MACE) in the range of 1.5-1.7%23. As compared to the PROGRESS-CTO Registry, where the previous CABG rate was as high as 32%, in the ERCTO registry, it was only 11.8%. This aspect might, at least in part, explain the lower MACE rate in the ERCTO than in the PROGRESS-CTO Registry24. However, the wide MACE rate variability is very likely to be biased by the underreporting of possible adverse events in registries where an independent events adjudication committee is often not available and by different existing definitions of procedural MI or MACE. Thus, these issues make “interstudy” MACE rate comparisons rather cumbersome.
THE RETROGRADE APPROACH
In our study, the retrograde approach was definitively adopted in more complex CTO lesions, as a bailout option in failed antegrade cases or to somehow facilitate the antegrade CTO body wire crossing, either intraplaque or in an extraplaque fashion. However, as compared with antegrade, the retrograde approach had a higher complication rate. Interestingly, among coronary perforations that occurred using the retrograde approach, one-third involved collateral circulation. This finding is consistent with most of the available literature202122232425. Similarly, in the Japanese Expert Registry and the Retrograde Summit General Registry, the channel perforation rates for the primarily retrograde approach were 10.2% and 6.2%, respectively23.
Furthermore, in our study, it has been outlined that a retrograde approach, among other identified independent risk factors of procedural MACCE, has the highest odds ratio so far. This finding is consistent with the results of the novel PROGRESS-CTO complication score, in which the retrograde approach has also been identified as a strong independent risk factor of MACE, besides age >65 years, moderate-severe calcification, blunt stump, antegrade dissection and re-entry, and female sex26.
OPERATOR EXPERIENCE
Many studies have found a correlation between operator procedural volume and the success rate of CTO PCIs162728. Indeed, Brilakis et al showed that an operator’s increased annual CTO PCI volume is associated with improved success without a significant increase in major complications16. On the contrary, in a contemporary multicentre registry, Karacsonyi et al showed that procedures performed by HVOs had higher technical success rates (87.9% vs 86.9% vs 82.6%; p<0.001), and higher rates of periprocedural major adverse cardiac events compared with MVOs and low-volume operators (LVOs) (3.08% vs 2.71% vs 1.50%; p<0.01). The authors justified this result by noting that the procedures performed by HVOs were significantly more complex, with higher J-CTO scores, compared with procedures performed by LVOs (2.72±1.27 vs 2.12±1.27, respectively; p<0.001)27. However, the adoption of different cutoffs to define operator expertise makes the “interstudy comparison” quite cumbersome.
For example, while in a report from the National Cardiovascular Data Registry, the annual procedural volume necessary to classify operators as experienced was at least 10 cases, more recently, in the Japanese Retrograde and Summit Registry, operators were classified as highly experienced if their annual procedural volume was >50 cases1628. In our study, as compared with MVOs, HVOs showed significantly higher technical success rates and lower overall complication rates, despite the higher mean lesion complexity and the higher number of retrograde procedures performed. However, as outlined by Brilakis et al, these data could be interpreted in view of the fact that there appears to be no upper limit in CTO PCI success rates with increased CTO PCI volume, suggesting that continuous improvement is possible for each level of operator expertise16.
CTO REVASCULARISATION NOVELTIES
In the last decade, novel approaches and dedicated devices for CTO PCI have contributed to the increasing procedural success. Among these, the radial approach has been shown to improve procedural performance through the reduction of vascular access site complications in CTO PCI as compared with the TF approach29. While in the past, the TR approach was considered taboo in CTO PCI, historically performed using a TF approach30, our experience demonstrates a trend switching towards TR. Indeed, the TR approach was used either exclusively (bi-TR) or in combination with TF (TR/TF) in a cumulative range of 60% of cases, leaving the dual femoral approach in only the remaining 16% of cases.
Beyond standard single lumen microcatheters that are essential in all CTO PCIs, DLMs have recently been shown to be a potential technology in specific CTO settings8. In our study, as expected, all these devices have been used significantly more often in retrograde than antegrade procedures, and, overall, in the more complex CTO lesions. Indeed, a DLM was used more frequently in cases of parallel wire technique, in ADR cases for distal re-entry, for side branch access in CTO bifurcation, for proximal cap penetration and for the engagement of angulated collaterals in retrograde cases.
Similarly, the recent adoption of GCEs has been shown to simplify and increase procedural success in a recent prospective study from Kandzari10. In our study, GCEs were used to facilitate equipment delivery − increasing antegrade support and speeding up the equipment exchange − both in antegrade dissection and re-entry or reverse controlled antegrade and retrograde tracking (CART) procedures.
Finally, despite the great, well-known utility of IVUS in CTO PCI, as shown in previous studies912, the adoption of this tool in our registry was only 21.3% (ranging between 10% and 70% among different operators and countries). This wide variability might be explained by the different ready availability in cath labs, by IVUS costs and finally by its reimbursement opportunity across different European countries. However, a more extensive use of IVUS, especially in complex settings such as the case of cap ambiguity, extraplaque navigation of the wire, unclear reverse CART, false-true wire position, and difficult guidewire access to the true lumen, may further improve in-hospital CTO PCI outcomes. In addition, increased use of IVUS to optimise stent expansion should improve longer-term CTO PCI outcomes.
Limitations
First, ERCTO is subject to the limitations of observational studies. Second, ERCTO does not have core laboratory assessments of the patients’ angiograms and composite assessments of the coronary anatomy, proximal cap ambiguity, lesion length, tortuosity and calcification, quality of the distal vessel, or the presence and quality of collateral circulation. Furthermore, there is not an independent angiographic and clinical event adjudication, which might therefore lead to an overestimation of technical success and, conversely, an underestimation of procedural complications. Thus, each centre was responsible for the accuracy and completeness of the entered data. Furthermore, there is a potential patient selection bias since the decision to enrol a patient into ERCTO is at the discretion of the operator and is not systematically followed by an oversight committee. Finally, the data presented in this manuscript reflect ERCTO practice and cannot be generalised for other European CTO PCI centres.
Conclusions
The ERCTO registry has reached high procedural success rates and low procedural complication rates even in highly complex lesions. Different patient-based and procedure-based factors were found to increase the risk of procedural complications. Operator experience is a leading factor in achieving a high procedural success rate.
Impact on daily practice
Contemporary outcomes of chronic total occlusion percutaneous coronary interventions (CTO PCI) in Europe showed a high procedural success rate and a low procedural complication rate, even in highly complex lesions. Recanalisation techniques (antegrade or retrograde), gender, operator experience and the arterial access site are the factors that play a major role in determining procedural success. All these factors should be taken into account when a physician is called to balance the potential risks and benefits of a CTO PCI. Lesions in the highest range of complexity, where a retrograde approach is indicated, should be attempted by high-volume operators only.
Acknowledgements
We thank Chiara Alaimo, MD, who provided the images for the Central illustration.
Conflict of interest statement
A. Bufe reports speaker honoraria from Biotronik and Shockwave Medical. A. Ladwiniec reports consulting/speaker/proctoring honoraria from Boston Scientific and Abbott. G. Werner reports speaker honoraria from Abbott, Asahi Intecc, OrbusNeich, Philips, Siemens, and Terumo. K. Mashayekhi reports consulting/speaker/proctoring honoraria from Abbott, Abiomed, Asahi Intecc, AstraZeneca, Biotronik, Boston Scientific, Cardinal Health, Daiichi Sankyo, Medtronic, OrbusNeich, Shockwave Medical, Teleflex, and Terumo. M. Ayoub reports consultant/proctor honoraria from Boston Scientific, Teleflex, Asahi Intecc, Cordis, Terumo, and SIS Medical. P. Agostoni reports consulting honoraria from Abbott, Boston Scientific, Cordis, iVascular, Medtronic, Neovasc, Seven Sons, Teleflex, and Terumo. R.D. Diletti reports consultant/proctoring honoraria from Asahi Intecc, Terumo, IMDS, Boston Scientific, Teleflex, and Philips. The other authors have no conflicts of interest to declare relevant to the contents of this paper.
Supplementary data
To read the full content of this article, please download the PDF.