Abstract
Aims: In comparison with non-occlusive lesions, percutaneous coronary intervention (PCI) of chronic total occlusions (CTO) represents a greater challenge for the interventionalist, due to lower procedural success rates, relatively higher incidence of procedural complications and the increased rate of restenosis. The European Registry of Chronic Total Occlusion (ERCTO) was created with the goal of evaluating the real impact of CTO PCI in the European context, trying to analyse the rates of procedural success, technical information from the CTO procedures and patient outcome.
Methods and results: Data collection was carried out in 16 centres across Europe, starting from the beginning of January 2008. In two years of activity, a total of 1,914 patients with 1,983 CTO lesions were consecutively enrolled in the registry. Overall procedural success was achieved in 1,607 lesions (82.9%); anterograde procedures obtained higher procedural success of retrograde ones (83.2% versus 64.5%, p<0.001). Coronary perforation occurred more frequently in patients who underwent retrograde approach (4.7% versus 2.1%, p=0.04). Although no differences were observed in terms of 30-day major adverse cardiac events between anterograde and retrograde treated patients, a trend toward higher periprocedural non-Q-wave myocardial infarction was found in patients in which the retrograde approach was attempted (2.1% versus 1% p=0.08). Moreover, retrograde approach was related with longer procedural and fluoroscopy times (156.9±62.5min vs. 98.2±52.8min and 73.3±59.9min vs. 38.2±43.9min respectively, p<0.001) and higher contrast load administration (402±161cc vs. 302±184cc, p<0.001).
Conclusions: The first report of the ERCTO registry by the EuroCTO club shows a high procedural success rate obtained by expert European operators in a “real-world” consecutive series of patients, comparable with those reported by Japanese registries. The rate of observed procedural adverse events was low and similar to the non-CTO PCI series. In this registry, retrograde procedures were associated with extended fluoroscopy exposure and procedural time, increased contrast load administration as well as a higher incidence of coronary perforations. Such outcomes should become the standard of care that all centres undertaking CTO PCI should aspire to.
Introduction
Coronary chronic total occlusions (CTOs) are found in more than 20% of patients affected by coronary artery disease and represent a common reason for surgical referral1. Despite the fact that several retrospective studies have shown the prognostic benefits of successful CTO revascularisation, there is no consensus on clinical indication for their treatment2-5. Moreover, in comparison with non-occlusive lesions, percutaneous coronary intervention (PCI) of CTOs represents a greater technical challenge, with lower procedural success rates, relatively higher incidence of procedural complications and increased rates of restenosis5,6 compared to non-CTO PCI. Over the last few years the increased use of the retrograde approach or other techniques specifically created by Japanese operators have resulted in improvement of procedural success from a previous average of 50-60% to 75-90% in the hands of experienced and skilled operators7. The European Registry of Chronic Total Occlusion (ERCTO) was created, with the goal of evaluating the real impact of CTO PCI in the European context, trying to analyse the rate of procedural success, the technical information from CTO procedures and to determine patients’ outcome. In the following article we present procedural and in-hospital outcomes of patients percutaneously treated for one or more CTOs who have been enrolled in this registry.
Methods
Study design and population
The ERCTO registry is a prospective, real-world registry in which all patients treated percutaneously for one or more CTO lesions involving a main coronary artery (≥2.5mm) or a saphenous bypass conduit were enrolled. Data collection was carried out in 16 centres across Europe. The enrolment started on the 1st of January 2008 and continues to date. The scheduled duration of clinical follow-up is three years after CTO procedure. The study was carried out in accordance with the Helsinki declaration, the ethics committee approved the protocol and all patients provided written informed consent before undergoing PCI procedure.
Definitions
Coronary CTO was defined as a TIMI (Thrombolysis In Myocardial Infarction) grade 0 flow within the occluded segment, with an occlusion duration greater than three months. The occlusion duration was divided into three levels of certainty as suggested by the EuroCTO club consensus document8. In short, the time of occlusion duration was described as:
a) “certain” (angiographically confirmed), in cases where a previous angiogram confirmed the presence of a TIMI 0 flow greater than three months prior to the planned procedure;
b) “likely” (clinically confirmed), objective evidence of an acute myocardial infarction in the territory of the occluded artery without other possible culprit arteries of more than three months before the current angiogram;
c) “undetermined”, a CTO with TIMI 0 flow and angiographic anatomy suggestive of a long-standing occlusion with stable anginal symptoms unchanged in the last three months or evidence of silent ischaemia.
Angiographic success was defined as final residual stenosis less than 30%, with a TIMI grade flow ≥ than 2. Major adverse cardiac events (MACE) were defined as cardiac death, acute myocardial infarction (AMI) or target vessel revascularisation (TVR). All deaths were considered of cardiac origin unless otherwise documented. Non Q-wave AMI was defined as a creatine kinase–MB (CK-MB) enzyme elevation > 3 times the upper limit of the normal value. When new pathological Q waves, in addition to enzyme elevation, were observed in the electrocardiogram the event was defined as a Q-wave AMI. TVR was defined as repeated revascularisation within the treated vessel. Stent thrombosis was defined, according with the definition of the Academic Research Consortium9. A procedure-related contrast-induced nephropathy (CIN) was defined as an increase of 25% or 0.5 mg/dl in serum creatinine at 48 hours after PCI comparing baseline values10.
Study endpoints
The primary endpoint of the study was the rate of procedural success in accordance with the primary strategy adopted, comparing results achieved using anterograde and retrograde approach. Secondary endpoints considered were procedural time, fluoroscopy time, contrast volume load, periprocedural complications (such as coronary perforation, CIN and MI) and in-hospital MACE.
Angiographic procedure
The angiographic characteristics of the CTOs were evaluated by the operator performing the procedure. At the beginning of the procedure patients received intravenous unfractioned (UNF) heparin (80-100 IU/Kg) to maintain an activated clotting time (ACT) ≥ than 300 seconds which was measured every 30-60 minutes so that, if required, an additional bolus of unfractionated heparin could be administered. Glycoprotein IIb/IIIa inhibitors were never administered. The antiplatelet therapy after stent implantation was administered according to recognised standard of care11. In the majority of cases, a 300 or 600 mg loading dose of clopidogrel was administered prior to the procedure. The dual antiplatelet therapy with aspirin (≥75 mg daily) and clopidogrel (75 mg daily) was in general prescribed for twelve months after the patient’s discharge.
The operators performed procedures according to their understanding of the needs of each particular case. Moreover, they chose the most appropriate CTO technique, taking into account the angiographic lesions characteristics and their personal skill. The strategies used included the single guidewire technique, the parallel wire technique, intravascular ultrasound (IVUS)-guided wiring technique, subintimal tracking and re-entry techniques, as well as retrograde techniques described elsewhere7,8,12-14. Dedicated guidewires were mostly used in order to perform these techniques, and ranged from soft polymeric wires, including Fielder XT (Asahi Intecc, Aichi, Japan), Fielder and Fielder FC (Asahi Intecc), to stiff flat or tapered spring ones such as Miracle 3-12 (Asahi Intecc, Aichi, Japan), Confianza Family (Asahi Intecc, Aichi, Japan). The sequence of use of these wiring techniques, and the selection of the guidewire, was completely dependent on the operator’s judgement.
In brief, the parallel wire technique involves two antegrade wires in which the first wire has tracked into a false lumen and its tip is used as a landmark to redirect the second wire through the true lumen. IVUS-guidance was used to identify the CTO entry point in cases where it was not visible. Retrograde wiring was used with all its modifications, such as pure retrograde wire crossing, touching wire techniques, Knuckle techniques and controlled anterograde retrograde tracking (CART) techniques as previously described7.
All patients were controlled for any post-procedural event such as evidence of pericardial tamponade, chest pain, heart failure, bleeding, or any ischaemic event. CK-MB, and troponin I were measured at 6-8 and 12-24 hours after the procedure (total rate of sample for CK-MB at each time points 87%, for Troponin I 24%), while serum creatinine was measured at 24 and 48 hours after procedure (total rate of sample 83%).
Statistical analysis
Continuous variables were presented as mean±standard deviations (inter-quartile range and median if not normally distributed) and were compared using Student unpaired t test. Categorical variables were presented as counts and percentages and compared with the chi-square test when appropriate (expected frequency > 5). Otherwise, the Fisher exact test was used. A p-value of <0.05 was considered significant. For the primary endpoint analysis we considered the outcome of procedure obtained with the intention to treat approach or, in the case of intra-procedural crossover from antegrade to retrograde and vice versa, the prevalent approach used. The predictors of procedural failure in patients treated by anterograde approach were identified using logistic regression. All clinical and angiographic characteristics were tested. All univariate variables with a p<0.1 were included in a statistical model in order to detect the independent predictors of procedural failure using multivariate regression analysis with the Wald method. Moreover, variables likely relevant for procedural failure were included in the final model despite a p>0.1 was found. An exploratory analysis comparing patients treated with anterograde and retrograde approaches was also performed. All data were processed using the Statistical Package for Social Sciences, version 15 (SPSS, Chicago, IL, USA).
Results
Population characteristics
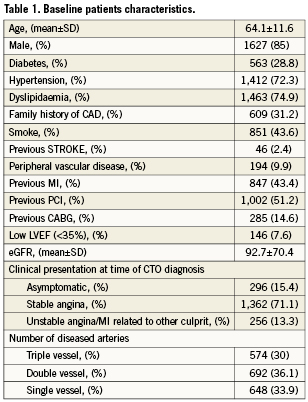
From January 2008 to the end of December 2009 a total of 1,914 patients with 1,983 CTO lesions were registered into a website database. Baseline patients’ characteristics are shown in Table1. In accordance with previous other large registries, the majority of patients were males. The 43.4% of patients had a history of previous MI, represented in most of the cases by non-ST elevation MI (57.1%). Moreover, in about half of these patients (47.5%) the previous MI was related to the territory subtending the CTO. Interestingly, 63.3% of these patients showed a normal ECG related to the CTO lesion. More than 2/3 of the population had a coronary multivessel disease (70%). CTO lesions characteristics are listed in Table2. Similar to previous reports, the most common CTO was the right coronary artery. It was possible to date the time of occlusion in accordance with EuroCTO club criteria in the majority of lesions (81.1%); in 45.7% of cases the time of occlusion was angiographically confirmed (certain) while in 35.4% it was only clinically confirmed (likely).
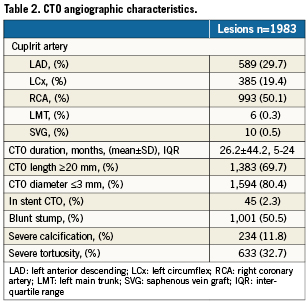
Angiographic outcome
Overall procedural success was achieved in 1,607 lesions (82.9%). The rate of success among re-attempts, following a previous failure, was slightly lower but significant (76.1%, p=0.001). An antegrade approach was undertaken in 1,749 lesions (88.2%), while a retrograde approach was used in 234 lesions (11.8%); the switch of the initial approach strategy in the same procedure was observed in 84 cases (4.2%): in 28 cases (1.4%), retrograde was switched with antegrade, while in the remaining 56 procedures (2.8%) antegrade was changed into the retrograde approach. Procedural success according to the approaches employed were 1,456/1,749 (83.2%) and 151/234 (64.5%), respectively for anterograde and retrograde (p<0.001). In the successful anterograde procedures, the single wiring technique was able to obtain CTO recanalisation in the majority of cases (68.2%), the parallel wire technique in 25.3% of cases, while IVUS guided and STAR techniques were used in a minority of patients (respectively 2.9% and 3.6%). For retrograde cases, retrograde wiring was the most performed technique (37.2%), the CART was used in the 31.8%, the touching wire in 22.3% and knuckle techniques in 8.7%. Procedural characteristics are showed in Table 3. In the majority of cases, the wires which finally reached the distal true lumen were stiff tapered guidewires such as the Conquest guidewires series, Cross-it guidewires series and Persuader 9 (38.8%). The details of the wires that crossed the lesions are reported in Figure1. Notably, the Fielder XT guidewire was able to reach the distal true lumen in 10.5% of lesions. The retrograde approach when compared to the anterograde one was seen to be more time-consuming (procedural and fluoroscopy times 156.9±62.5min versus 98.2±52.8min p<0.001 and 73.3±59.9min versus 38.2±43.9min p<0.001, respectively). Additionally, in patients treated by the retrograde approach, higher amounts of contrast was administered (402±161cc versus 302±184cc, p<0.001).
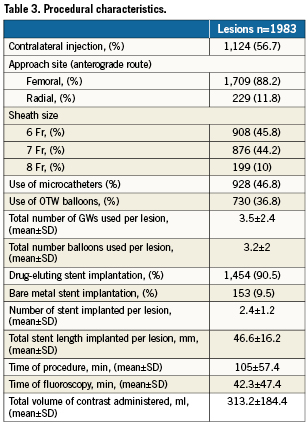
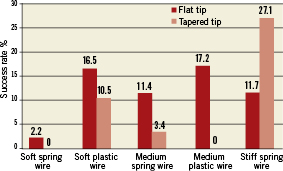
Figure 1. This graph shows the prevalence of wires able to successfully cross the CTO lesions in the study. Soft spring wires include: BMW, BMW Universal, Prowaterflex, Runthrough. Soft plastic wires include: Fielder, Whisper, PT Graphic as flat tip type and Fielder XT as tapered tip type. Medium spring wires include: Medium and Miracle 3 as flat tip type and Crossit-100 as tapered tip type. Medium plastic wires include all Pilot wire series. Stiff spring wires include: Miracle 4.5, 6, 9, 12, Persuader 6 as flat tip type and Conquest wire series, Crossit-200, 300, 400 and Persuader 9 as tapered tip type.
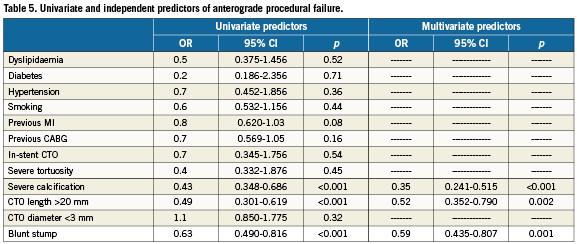
Predictors of procedural failure
Among lesions treated by anterograde approach, blunt stump, CTO length > 20 mm and the presence of severe calcifications were recognised as univariate predictors of procedural failure (OR 0.63, 95% CI 0.490-0.816 , p<0.001, OR 0.49, 95% CI 0.301-0.619 p<0.001 and OR 0.43, 95% CI 0.348-0.686, p<0.001, respectively). After multivariate analysis the same variables resulted independent predictors of procedural antegrade failure (OR 0.59, 95% CI 0.435-0.807, p=0.001, OR 0.52, 95% CI 0.352-0.790, p=0.002 and OR 0.35, 95% CI 0,241-0.515, p<0.001, respectively).
In-hospital outcome
Table 4 summarises complications and in-hospital outcomes, stratified according to the type of approach carried out. Post-procedure assessment of CK-MB was performed in 97% of patients. Among these, a mere 26 patients satisfied the definition of MI. There was an unfavourable trend towards non-Q wave MI in patients treated with the retrograde approach, while no differences were found concerning the Q-wave MI. There was one case of definite stent thrombosis and one case of stroke, both in patients treated with the anterograde approach. Coronary perforation occurred in 2.6% of cases, but more frequently in patients who underwent the retrograde approach. Coronary perforation caused cardiac tamponade in 0.5% of cases (11/1,983); in all of these cases pericardiocentesis was performed. Access site vascular complications were observed rarely (0.7%), and they required vascular surgery in 2/14 (14.3%) of these cases.
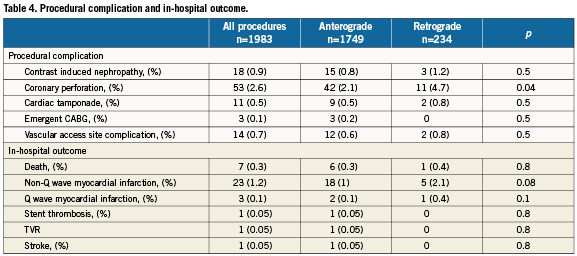
In-hospital death occurred in seven patients (0.3%); in two cases, death was not related to cardiac cause (reacutisation of chronic obstructive pulmonary disease); in the other two cases death was caused by damage to the donor artery (one was a flow-limiting dissection of the left main during a retrograde approach; the second, athrombosis of the donor artery related to the simultaneous coronary cannulation during an antegrade procedure); two patients died after emergency cardiac surgery, undertaken because of coronary perforation; and one patient died from subacute stent thrombosis. No differences were observed in the distribution of access site complications between patients treated by femoral vs. radial approaches (0.7% versus 0.4%, p<0.6). Patients with procedural failure showed a higher rate of 30-day death and non-fatal MI in comparison with patients successfully revascularised (1.9% versus 0, p<0.001 and 3.6% versus 0.8%, p<0.001, respectively).
Discussion
The major findings of the present study can be summarised as follow:
– the procedural success rate of CTO PCI among the operators of EuroCTO club is similar to that reported in the Japanese registry15-17;
– the in-hospital MACE and other procedural complications are low and comparable to non-CTO PCI series18,19;
– the retrograde approach is associated with extended fluoroscopy and procedural time, increased contrast load administration and a higher incidence of coronary perforations.
Procedural success rates and in-hospital outcomes
The largest registries carried-out dating from the pre-stent era up until the beginning of the drug eluting stent era –often including recent and “functional CTO” (>TIMI 0 flow) occlusions– have reported a rate of procedural success around 65-70% as well as a rate of in-hospital MACE of about 3.5-5%2-5. Taking into consideration the definition reported in EuroCTO club consensus document, the current success rates of experienced operators, not specialised in CTO-PCI is <55%. In the CONQUEST (CTO New techniQUE for Standard procedure) registry, which was conducted by CTO “specialised” operators at six Japanese centres, the rate of procedural success at first attempt obtained in a series of 116 denovo CTOs was 86.2% with a low rate of periprocedural MACE15.
Recently, Rathore et al have shown a 87.5% procedural success rate in 665 consecutive lesions, treated at the Toyohashi Heart Center from 2002 to 200816. Of interest in this review, the rate of success increased from an initial 80% up to 90% within two years and then remained almost unchanged during many years, underscoring the importance of recent techniques and experience for these types of lesions. Despite the high rate of type 1 coronary perforations (9.8%), the rate of in-hospital MACE was acceptably low (1.9%), with an in-hospital mortality of 0.5%. Noteworthy, coronary perforations and in-hospital MACE occurred more frequently in patients with procedural failure (20.2% vs. 7.4, p<0.01 and 1.5% vs. 4.4%, p=0.03, respectively) related to the aggressive guidewire strategies adopted in this study16.
The J-CTO represents a multicentre registry carried out in 12 Japanese centres enrolling 498 consecutive patients with 528 CTO lesions17. In this study, the overall procedural success was comparable with previous “Japanese experience” (86.6%), showing afavourable procedural outcome in terms of in-hospital adverse events (death 0.4%, MI 2.3%, coronary perforation 10%). Despite the use of the retrograde approach in more than 25% of cases the rate of procedural success in the retry case was lower in comparison with the “first touch” cases (68.5% vs. 86.6%) in accordance with the findings of our study.
In a retrospective cohort of patients treated percutaneously for CTO lesions in two United States centres, Thompson et al showed the influence of operator expertise20. The reported overall success rate among 636 consecutive CTOs treated was about 69%, but there was a significantly lower success rate in operators not able to perform the retrograde approach in comparison with retrograde operators (58.9% vs. 75.2% respectively, p<0.0001). Moreover, in procedures performed by non-retrograde operators, the total procedural time was longer and more contrast agents were administered20.
The present study was carried-out in centres with a specific program for CTO treatment accomplished by skilled operators able to perform the retrograde approach if required but, in essence, all of them had a dedicated program with a skilled staff. Such a CTO-focused environment, with an understanding of the available technology and outcome data as well as appropriate high numbers of cases performed, is likely to explain the high procedural success similar to the Japanese experience. This study highlights some differences of European strategy in comparison with the Japanese series such as the lower use of dual coronary injections and the relative higher use of the radial approach. Despite these different approaches, the recent development of new guidewires and device technologies could explain the increase of procedural success achieved using this “simple strategy”. The very low rate of procedural complications and in-hospital MACE achieved in this study suggests that CTO should no longer be a reason for referral to CABG. Recent evidence reports low rates of procedural success in combination with a low incidence of periprocedural events in patients who underwent CTO PCI in non-dedicated centres21. However, we doubt that such high success rates and low event rates exist in non-dedicated centres, but clearly these results should be the standard for all hospitals undertaking these procedures when they audit their cases.
The influence of different approaches
To the best of our knowledge this study represents the largest series of patients treated with PCI for CTOs lesions with the current armamentarium of devices and techniques. In comparison with the Japanese series, the retrograde approach was used less frequently by European operators, who nevertheless achieved similar rates of procedural success. Indeed, in a Japanese retrograde registry of 157 consecutive procedures, the success rate obtained was 65.6%, comparable with ours of 64.5%22. This might explain why the retrograde approach was used in most of cases after a prior failed anterograde approach, and as a first choice in case of a very difficult anterograde attempt. We thus see that patients undergoing the retrograde approach are more likely to have the most challenging lesions. On the other hand, we must acknowledge the fact that the retrograde approach is a demanding procedure which should be left to experienced operators after a long period of training23. A preliminary report of expert operators from the EuroCTO club has shown a high procedural success with the retrograde approach in a series of 175 patients treated in seven centres throughout Europe24. The operators were keen to learn and apply this novel technique in all cases that were ideal for a retrograde approach, but which were also favourable for an antegrade approach. In this study, the most important factor responsible for procedural failure was the inability to cross the collateral channels with a retrograde wire24. The lower success rate of the current registry may be due to the fact that the retrograde technique was restricted to the worst cases, and to those with antegrade failure. The present study confirms that the choice of the retrograde approach is associated with an increase of fluoroscopy exposure, procedural times and contrast load administration. One of the reasons for this finding could be the use of the retrograde approach immediately after the antegrade failure, which was seen in about 25% of the retrograde cases. Moreover, the rate of coronary perforations was higher among patients treated with the retrograde approach, without differences in clinical sequelae but with an unfavourable trend of non-Q wave MI, suggesting that the retrograde approach might be considered an aggressive approach.
Predictors of procedural failure
The multivariate logistic regression analysis has shown that severe calcifications, a CTO length of more than 20mm and the presence of a blunt stump are associated with anterograde failure. These angiographic characteristics were previously recognised as independent predictors of procedural failure by previous studies3,5,16,17. Moreover, in contrast with previous data, we did not show any significant association of procedural failure in the presence of multivessel disease, previous MI or CABG. However, comparison of predictors in different studies can be difficult because of the small sample size of most studies, the lack, in some series, of angiographic and morphological CTO characteristics, and the differences regarding the definitions used for the detection of angiographic features. Finally, it is interesting to note that the improvement of materials and the development of techniques has dramatically changed CTO PCI in the last five years; therefore, it may be not very reliable to take into consideration older studies for comparison when dealing with this topic.
Study limitation
This study has some limitations. First, its non-randomised nature may cause a selection bias which may influence the results. Second, the study was carried out by CTO-dedicated expert operators, therefore the results obtained could not reflect the actual success rate of CTO PCI in Europe. Third, the choice of guidewires and techniques employed was at the operator’s discretion, and this may be a somewhat confounding factor in the interpretation of procedural results. Fourth, an independent corelab did not analyse the angiographic characteristics of the lesions treated. Finally, there were no pre-specified criteria to stop the procedure; due to this, time of fluoroscopy, time of procedure and contrast load administration are strongly correlated to the decision of each individual operator to continue the attempt.
Conclusion
The first report of the ERCTO registry by the EuroCTO club shows a high procedural success rate obtained by expert operators in a consecutive series of patients. In the most experienced hands and at dedicated centres –despite the complexity of procedures as shown by high procedural and fluoroscopy times– the incidence of in-hospital MACE was comparable with non-CTO PCI registries.
Conflict of interest statement
The authors have no conflicts of interest to declare.