Abstract
Aims: Despite successful prevention of lesion recurrence by drug-eluting stents (DES), and the advancement in procedural techniques in the treatment of chronic total coronary occlusions (CTO), the number of CTOs treated by percutaneous coronary intervention (PCI) is still low as compared to their prevalence. This study aims to assess the outcome of PCI for CTOs in a contemporary survey of PCI in interventional centres in Germany.
Methods and results: The basis of this analysis is the 2006 quality assessment database of PCI conducted by the ALKK (working group of cardiology centres). Thirty-five centres contributed to this database, representing about 10% of all interventional centres of Germany. From a total of 20,502 patients, 8,882 patients with stable angina were selected. Of these 674 patients (7.6%) underwent PCI for a CTO. Their procedural characteristics and the hospital outcome were compared with patients treated for non-occlusive lesions. As compared to non-occlusive lesions, less patients underwent ad hoc PCI for a CTO. The fluoroscopy time was almost double of that in non-occlusive lesions, and contrast usage was significantly higher. The success rate was 60.1% as compared to 97.3% (p<0.001). Severe intraprocedural and in-hospital complications were similar for CTO and non-CTO lesions. Almost all patients with a CTO received a stent; DES were used in 53.4%, which was higher than the rate in non-CTO lesions (38.9%; p<0.001).
Conclusions: Although the success rate for PCI in CTOs is still well below that in non-occlusive lesions, this procedure is safe, encouraging its wider application. The low rate of DES use did not reflect the evidence for DES in CTOs.
Introduction
Chronic total coronary occlusions represent a lesion subset that is not widely accepted as an indication for PCI, which is reflected by the low level of evidence attributed to the interventional therapy of CTOs in present guidelines1,2. The uncertainty on the therapeutic strategy is due to a lack of randomised trials regarding the benefit of PCI in CTOs of more than one month duration, and further corroborated by the negative outcome of the Open Artery Trial addressing occlusions of less than four weeks duration after a previous MI3. However, the latter trial is not representative for CTOs4, and there are consistent data from cohort studies on the improvement of LV function after CTO revascularisation5-11, and long-term observations suggest a lower mortality12,13.
The major setbacks for the revascularisation of a CTO by PCI are the low primary success rate to cross the CTO, and the low long-term patency rate14. The latter problem had been solved by the use of drug-eluting stents for CTOs, but the primary problem still remains15. One possible issue that holds back a more liberal and aggressive approach towards CTOs is the assumed higher risk of complications with these often complex and long procedures in otherwise stable patients. There are historical data on the complication rate, but many originate from specialised centres, and do not represent the broad experience in every day practice16-20. Therefore, we analysed the database of the quality control programme implemented in 35 representative PCI centres in Germany who collected periprocedural and in-hospital outcomes data of all PCIs performed in the year 2006, in order to assess the general approach towards CTOs in centres not specifically dedicated to CTO treatment.
Methods
Data source
The ALKK PCI registry was designed as a quality control data acquisition registry to survey procedural details and outcome of all PCI procedures performed in participating hospitals. The year 2006 was chosen as the basis of the present analysis. Thirty-five centres participated in this registry providing a complete overview of all their consecutive annual PCI procedures. Details of 21,560 procedures performed during 20,502 hospitalisations were documented.
Demographic data, patient’s history, procedures, complications, current treatment, and intra-hospital complications were documented. Data entry was done using the local catheterisation laboratory software documentation, and the data set was then sent at the end of the year to the central analysis centre at the Institut für Herzinfarktforschung an der Universität Heidelberg, Ludwigshafen, Germany. By applying a benchmark reporting system, this study should help implementing existing clinical guidelines.
Study objective
The present analysis focused on patients with stable angina pectoris, comparing patients with and without a CTO as the primary target of the PCI. The procedural characteristics regarding use of contrast media, fluoroscopy time, procedural success and stent use, as well as, the periprocedural complications and in-hospital outcome should be compared between these two groups. For each patient, the first PCI during hospitalisation was evaluated.
Definitions
Stable angina was diagnosed according to the Canadian Cardiovascular Society Functional Classification (Class I-III). In these patients, the CTO was defined by the detection of TIMI 0 flow and a stenosis degree of 100% at the lesion site. The duration of the CTO was determined by the local physician from the patient’s history. No strict minimum duration time line was set, as the more recent definition was not in place at the time of this study21. Recent post myocardial infarction (MI) CTOs were excluded by excluding patients presenting with acute coronary syndrome or cardiogenic shock. Periprocedural MI was defined as a three fold increase of creatinine kinase measured 24 hours after the procedure. MI during follow-up was defined as an ischaemic episode leading to rehospitalisation with evidence of increased cardiac marker enzymes, or evidence of new Q-waves related to the treated coronary artery. Major adverse cardiac or cerebrovascular events (MACCE) were defined as death, MI, or stroke after the PCI during hospitalisation.
Statistics
Data are presented as absolute numbers and percentages, or median and quartiles (25%-75%). Categorical variables were generally compared by Pearson chi-square test, but for infrequent events Fisher’s exact test was used. Continuous variables were compared by Mann-Whitney-Wilcoxon rank-sum test. All statistical comparisons were two-tailed, and P values ≤0.05 were considered statistically significant. All analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA).
Results
Clinical and angiographic characteristics of patients with stable angina and a CTO
In total, 8,882 patients with stable angina pectoris as presenting cardiac symptom underwent PCI in the participating 35 interventional centres. These centres represented the typical range of PCI experience in German invasive centres from around 100 PCIs per year to almost 2,000 PCIs per year (Figure 1). The number of CTO procedures was not evenly distributed and not correlated with the total number of PCI procedures. There were centres with equal total PCI load but distinctly different numbers of CTO procedures per year. The highest rate was about 10% of all PCI procedures, on average it was below 5% (Figure 1).
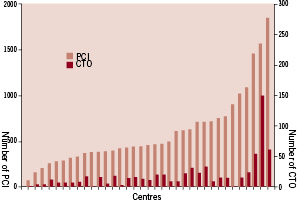
Figure 1. The graph represents the 35 individual centres participating in this registry, with their respective number of PCI (left scale) and CTO procedures (right scale). Note the different scale for both procedures.
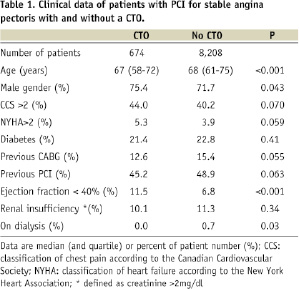
In 8,882 patients 10,961 segments were treated, out of which 714 (6.5%) were categorised as CTOs. The 674 patients undergoing PCI for a CTO were younger and tended to be more often male than those with PCI for non-CTO lesions (Table 1). LV function was more severely impaired in the CTO group with a trend towards more pronounced symptoms of angina and heart failure. On the other hand, they had less frequently a previous revascularisation procedure. There was no difference in the prevalence of diabetes or renal insufficiency (Table 1).
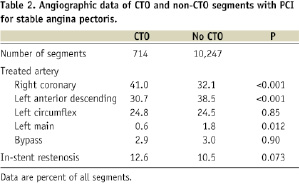
With CTOs the target lesion was more often in the right coronary artery than in the left anterior descending artery. There was a small number of lesions treated in the left main artery, however, this location appeared to be less often represented in the CTO group. In-stent lesions were similarly often represented in the CTO and non-CTO group (Table 2).
Procedural outcomes of PCI with and without a CTO
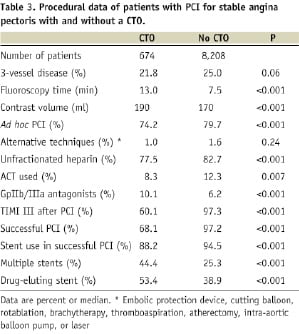
PCI for CTOs took longer and required more contrast volume than for non-CTO lesions, but the absolute values were moderately high with 13.0 minutes of fluoroscopy time and 190 ml of contrast for CTO procedures. A considerable number of 74% of all procedures were done ad hoc after a diagnostic angiography. More patients received GpIIb/IIIb antagonists when a CTO was treated as compared to non-occlusive lesions, even though the patients were by definition in a stable condition, and patients with unstable angina or acute coronary syndromes had been excluded from this analysis.
TIMI 3 flow was achieved in only 62.3% of segments in the CTO group as compared to 97.7% in the non-CTO lesion group. The investigator assessed success rate for CTOs was 68.1%, including outcomes with TIMI 2 flow. Stents were used in successfully opened CTOs in a slightly lower rate as with non-CTO lesions of around 90%, but more multiple stenting was required for CTOs. The rate of DES used in stented lesions was higher in CTOs than with non-CTO interventions, but given the fact that CTOs represented the more complex lesions with more stents per lesion, a DES use of 53.4% was still low given the expected high recurrence risk (Table 3).
Outcome in patients with a CTO undergoing PCI
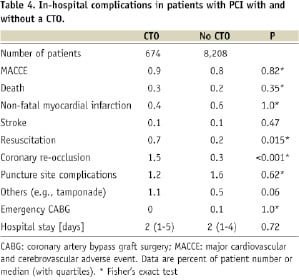
In patients who underwent a PCI for a CTO, minor periprocedural events were observed slightly more often, most notably vessel re-occlusion in 1.5%, which may be interpreted as a typical risk for these lesions. Life-threatening intraprocedural events were infrequent. The rate of pericardial tamponade not specifically listed in the database was summarised among other non-specified complications, which was slightly higher with 1.1% as compared to 0.5% (Table 4). Most notably the in-hospital outcome was not significantly different between PCI for CTOs or non-occlusive lesions with a MACCE rate of 0.9% and 0.8%, respectively. Despite a more complex procedure, the puncture site complications and length of hospital stay were not increased in PCIs for CTOs (Table 4).
Discussion
In this survey of patients with stable angina pectoris undergoing PCI in 35 German interventional centres in 2006, the fraction of interventions for chronically occluded lesions was only 7.6%, whereas the expected prevalence of CTOs among patients with stable angina is in the range of 20%-30% depending on the selection criteria for the diagnostic angiography22,23. Furthermore, the fraction of CTO procedures of all PCI procedures per centre was low and varied considerably among centres. For example, in the highest volume PCI centre participating, only 4% of procedures were dedicated to CTOs (Figure 1). This underscores the limited utilisation of PCI for this lesion subset in today’s clinical routine, similar to observations more than a decade ago22,24,25. This situation has not changed much despite the considerable advancement of PCI technique21.
The low fraction of CTOs among PCIs observed in the present study is in a similar range of 6% found in recent reports of contemporary PCI practice in the USA18,19. A possible explanation for the underuse of PCI in CTOs would be the still controversial and ambiguous indication for revascularisation of these lesions in the absence of a randomised trial, despite good clinical evidence and pathophysiological reasoning in this regard26. There are some facts also evident in the current survey which further explain the low proportion of CTOs in contemporary daily practice.
Procedural complexity and success rate
The procedural time and the contrast volume are significantly higher for the treatment of CTOs. Despite this increased use of resources, the absolute values of the median fluoroscopy time of 14 minutes and contrast volume of 190 ml are rather low as compared to those reported from specialised CTO treatment centres where these lesions are treated in a much higher proportion with advanced techniques27,28. There is no exact information of CTO duration available, except that patients with acute coronary syndromes were excluded, so that also recent CTOs below the defined threshold of three months were present. These facts indicate, that the target lesions selected by the operators were less complex than those lesions targeted in these specialised centres21. Another aspect seems to be a selection bias when choosing PCI for CTOs towards slightly younger patients.
Despite this bias for less complex CTOs in our survey, the success rate was still lower for CTOs as compared to non-CTO lesions. If we consider the successful recanalisation of a CTO to be achieved with the constitution of TIMI 3 flow, then only 62% of lesions were successfully revascularised. The success rate per patient was 60%. It is noteworthy that the success rates reported from comparable recent surveys from the USA are in the same range, indicating that the contemporary practice in catheterisation labs in Germany and in the USA are similar with respect to CTOs. The expected lower primary success rate and higher procedural cost and effort29-31 are probably the major reasons for the low frequency of PCI in CTOs, and specifically the exclusion of more complex CTOs. On the other hand, we must be aware of the potential of modern PCI techniques in complex CTOs with success rates of up to and above 90%32-34, and the question arises whether patients in the general population are denied this full potential of current interventional therapy?
The higher prevalence of RCA lesions among the CTOs may not be due to a selection bias, but rather reflects the observation that CTOs appear to be more frequent in the RCA22,23,25. One may speculate that patients with occlusions of a prognostically important LAD are more likely to die before being diagnosed with a CTO. However, another explanation may be derived from the differences in the anatomic course of the RCA and the left coronary branches: The RCA has a long segment that serves mainly as a conduit with few important branches, and most notably the coronary flow velocity profile is distinctively different35.
Stent use in CTOs
One argument against extensively complex interventional attempts in patients with a CTO would be the rather discouraging high rate of lesion recurrence, and typically re-occlusion even with the routine use of stents36. However, with the advent of drug-eluting stents this problem was convincingly resolved with a long-term outcome similar to that in non-CTO lesions37-39. Many of these studies had been presented before 2006, the year of the present survey, but had not yet led to specific consideration in daily practice. Despite the more than double rate of need for multiple stents in CTOs as compared with non-occlusive lesions, and the evidence of an adverse influence of this factor on lesion recurrence36, the rate of DES was not higher for CTOs. Given the fact that the benefit of a reduced lesion recurrence is highest among complex lesions like CTOs37,39, this evidence had not been applied in practice during the time period of this survey in 2006. This may have changed presently, as CTOs are mentioned explicitly as one of the few lesion specific indications for DES in recent guidelines1,40.
Procedural complications and hospital outcome
The data on in-hospital complications showed no differences in major complications. During the procedure, more often a lesion re-occlusion was reported, but this is an inherent and specific procedural problem of a CTO and does not constitute a major problem, whereas major periprocedural complications like pericardial effusion, considered to be typical for recanalisation procedures, were not reported more frequently. This may be due to a moderate aggressive strategy towards the CTO with regard to the wire selection, as dedicated stiff wires are not frequently used outside of expert centres20.
Even with recent and advanced approaches towards CTOs including a high rate of retrograde approaches, the expected complication rate has not necessarily increased, as recently shown in a report from a leading Japanese institution where the major complications were also in a low range similar to the one observed in our registry41.
One interesting observation needs to be commented on, which was the surprisingly higher use of GpIIb/IIIa antagonists during PCI for CTOs. A possible explanation could be the assessment of some of the occlusions as subacute, early after a previous acute MI, even though the selection criteria of this data analysis included only patients with stable angina. The GpIIb/IIIa antagonists did not lead to more severe complications, but it is strongly discouraged to use these agents as they are difficult to antagonise in case of a pericardial effusion as a typical complication during PCI for CTOs. Furthermore, there is no evidence supporting the use of these agents in CTOs. The idea for its use, even though unsupported, might be the misconception of a high thrombus load of totally occluded arteries, which is only true for acute and subacute occlusions, but not for CTOs, where we find only organised thrombus42.
Strength and shortcomings of the ALKK registry
This registry reflected the daily practice in the catheterisation lab routine of German interventional centres with a typical wide range of individual PCI experience, but it does not allow the specific analysis of angiographic features of the treated CTOs such as lesion length and duration of the occlusion, which would be indicators of the expected success rate. From the overall low percentage of CTO lesions among the target lesions, we may conclude that the lesions were already well selected according to these aforementioned lesion characteristics. The registry does not allow the further scrutiny of the basis for the indication of a CTO as compared to non-occlusive lesions.
Clinical implications
The present registry analysis reflects current clinical practice towards PCI for CTOs. The question arises whether the indication should be broadened, and more patients than treated presently might profit from a successful CTO treatment.

