Abstract
Aims: Limited data exist on the treatment and outcomes of patients with chronic total occlusions due to in-stent restenosis (CTO-ISR). We sought to evaluate results and clinical outcomes in percutaneous interventions over CTO-ISR.
Methods and results: We conducted a registry in 16 centres involving consecutive patients undergoing attempted percutaneous intervention over CTO-ISR. A total of 233 patients were included, 192 (82.4%) with a successful acute result. The success rate was significantly lower in patients with: lesion in the circumflex artery, ostial lesions, J score >3 and no femoral access. The presence of tandem lesions (OR 0.19, 95% CI: 0.06-0.68; p=0.01) was identified as an independent predictor for outcome. After a median follow-up of 20 months, cardiac death in the successful vs. failed groups was 3% and 8.3%, respectively (p=0.09). Independent predictors for mortality were previous CABG (HR 8, 95% CI: 1.3-50; p=0.02) and multivessel disease (HR 2.3, 95% CI: 1.2-4.3; p=0.01). In the successful group, TLR was 15%, re-occlusion 6% and definite/probable stent thrombosis 1.8%.
Conclusions: Percutaneous treatment of CTO due to ISR in contemporary practice shows a high success rate, resulting in good long-term results. The angiographic and procedural predictors identified may contribute to improving procedural outcome through better patient selection.
Abbreviations
CTO: chronic total occlusion
DES: drug-eluting stent
ISR: in-stent restenosis
MACE: major adverse cardiac events
PCI: percutaneous coronary intervention
TLR: target lesion revascularisation
Introduction
Coronary chronic total occlusions (CTO) due to in-stent restenosis (ISR) are not uncommon, representing from five to 25% of all CTO undergoing percutaneous coronary intervention1-3.
Limited data exist on the treatment of CTO-ISR. Registries published so far have been really limited in size (two to 78 cases), most performed in highly skilled centres or focused on the use of specific devices and all of them without long-term clinical follow-up1-8. The percutaneous revascularisation success rates reported for these restenotic occlusions have generally been lower than those observed on native vessels1,3. In a registry performed in five centres with highly skilled operators for CTO using a high rate of retrograde approach, dissection/re-entry techniques and specific devices, the success rate resulted in being quite similar to that observed in de novo CTO lesions8.
In addition to the inherent challenges posed by an occluded coronary segment to wire passage in conventional CTO PCI procedures, CTO-ISR pose specific procedural challenges, including the presence of calcific or heterogeneous in-stent neoatherosclerosis, stent underexpansion or fracture, presence of more than one layer of stent struts, extreme tortuosity of the stented segment, and aorto-ostial stent location. Correction of underlying triggers of stent restenosis as part of the CTO PCI procedure is key to improving long-term outcomes1,3,9.
A multicentre registry was designed to examine the procedural characteristics, technical success rates and clinical outcome in patients with CTO-ISR.
Methods
We conducted a retrospective registry in 16 centres with a variable degree of experience in CTO procedures. All consecutive patients in the period 2003-2013 undergoing attempted PCI over a CTO-ISR were included.
Medical records and coronary angiograms were reviewed to determine the clinical and angiographic characteristics, techniques utilised and success rates of the interventions. The choice of procedural strategy, equipment utilisation and antithrombotic therapy was made by the interventional cardiologist performing the procedure. Follow-up data were collected from hospital charts, by contacting patients or by referring physicians. No routine angiographic follow-up assessment was available but angiographic evaluation was carried out in all cases showing symptomatic recurrence or presenting abnormal findings in non-invasive tests for ischaemia or ventricular function. The study was approved by each institutional review board.
EVENT DEFINITIONS
Chronic total occlusions were defined as coronary obstructions with Thrombolysis In Myocardial Infarction (TIMI) flow grade 0 of at least three months duration. The estimation of the occlusion duration was made on the basis of the onset of symptoms, history of myocardial infarction in the target vessel territory or comparison with a previous angiogram. The CTO was attributed to ISR if located within a previously implanted stent or within the 5 mm margins proximal and distal to the stent edges. All patients with a recent acute coronary syndrome had a non-CTO culprit lesion that was initially treated and subsequently returned for PCI of the CTO-ISR because of persistent symptoms and/or related ischaemia.
Procedural success was defined as achievement of residual post-PCI stenosis less than 30% in the target lesion, associated with TIMI flow 3, without the occurrence of death, myocardial infarction or repeat lesion revascularisation during the index hospitalisation.
Death was regarded as cardiac in origin unless an obvious non-cardiac cause could be identified. Myocardial infarction was defined according to the third universal definition by the European Society of Cardiology and the American College of Cardiology Foundation. Target lesion revascularisation (TLR) was defined as any repeat percutaneous intervention of the target lesion or bypass surgery of the target vessel performed for ischaemia-driven restenosis or other complication of the target lesion. Target vessel revascularisation (TVR) was defined as any repeat percutaneous intervention or surgical bypass of any segment of the target vessel, which included upstream and downstream branches and the target lesion itself. Stent thrombosis was defined according to the Academic Research Consortium criteria.
Angiographic characteristics expected to be predictive of procedural success were classified according to recommendations proposed by the consensus document of the EuroCTO club10. The J-CTO score was calculated for each lesion based on occlusion length, stump morphology, presence of calcification, presence of tortuosity, and prior attempt to open the CTO11.
STATISTICAL ANALYSIS
Continuous variables are reported as mean±SD or median (interquartile range [IQR]), as appropriate. Categorical variables are reported as percentages. Chi-square test or Fisher’s exact test analysis was used for comparison of categorical variables. The Kolmogorov-Smirnov test was used to test for normal distribution of continuous data. Continuous variables were compared using the Student’s t-test or Wilcoxon rank-sum test according to their distributions. Survival free from cardiac death and MACE is shown by Kaplan-Meier curves, and the differences between groups were assessed by the log-rank test. A logistic regression analysis for predictors of procedural success was performed including all variables listed in Table 1 and Table 2 which showed a p-value <0.2 in the univariate analysis. A Cox proportional hazards model for predictors of mortality was conducted entering variables listed in Table 1 and Table 2 and showing a p-value <0.2 in the univariate analysis. All the statistical analyses were two-tailed with p-values <0.05 considered statistically significant. Analyses were performed using the SPSS software package, Version 15.0 (SPSS Inc., Chicago, IL, USA).
Results
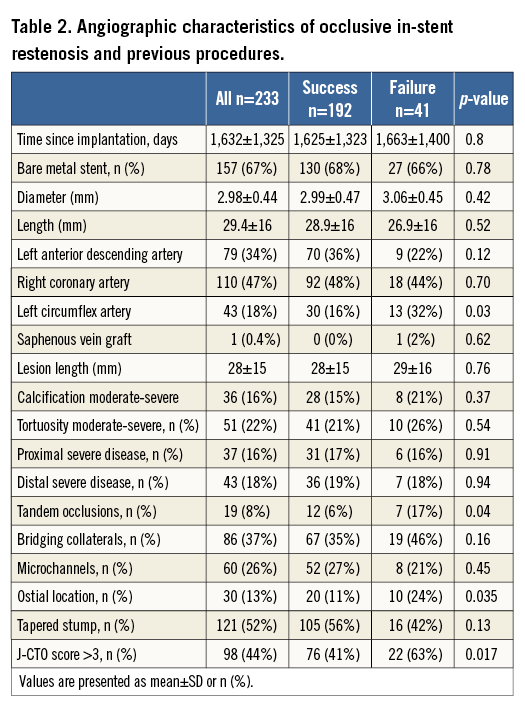
A total of 233 patients were included in the registry. The type of stent leading to CTO-ISR was known in 221 (95%) patients; of these, 67.4% were bare metal and 32.6% drug-eluting stents. Procedural success was achieved in 192 (82.4%) cases; the vast majority of failures were due to inability to cross the occlusion with the wire up to the distal true lumen. The number of cases treated, both failed and successful, and the corresponding success rates along the time period of recruitment are shown in Figure 1. A trend for increasing success rate was observed along the time period of recruitment, from 76% in the early period to 85% in the most recent.
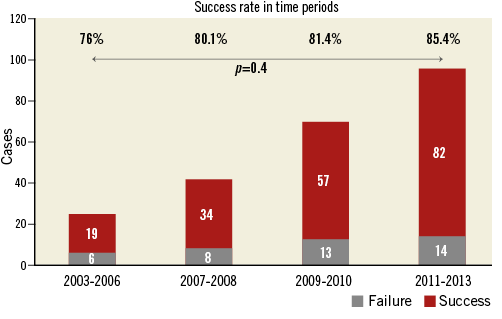
Figure 1. Success rates along the time period of recruitment. The number of cases treated, both failed and successful, and the corresponding success rates, are shown for different time periods.
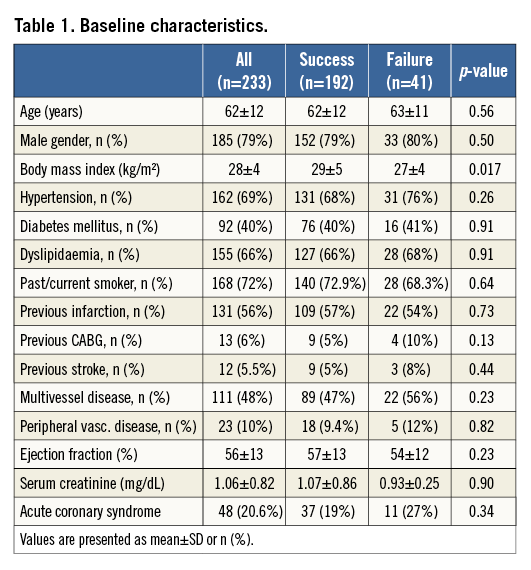
Baseline characteristics of patients with procedural success or failure are shown in Table 1. All baseline characteristics, with the exception of body mass index, were similar in both groups.
The angiographic characteristics for both groups are shown in Table 2. Patients with failed procedures showed a higher frequency of circumflex artery involvement (32% vs. 16%, p=0.03) and of ostial location (24% vs. 11%, p=0.035). Procedural success was lower in the left circumflex artery when compared with other target vessels (69% vs. 86%; p=0.008), whilst procedural success in the left anterior descending artery was 89.6%. Ostial lesions showed a significantly higher rate of severe calcification when compared with non-ostial location (20% vs. 3.5%; p=0.003). The complexity of the occlusive lesions was high, as was shown by the J-score, which was higher in failed cases (J-score >3 in 63% vs. 41%; p=0.017). In Figure 2 the success rates for the different values of J-score are shown, presenting significant differences for success between score values. This was related to the presence of more severe calcification, more tortuosity and a lesser presence of tapered stump in failed cases. The presence of tandem occlusions was more common in failed cases.
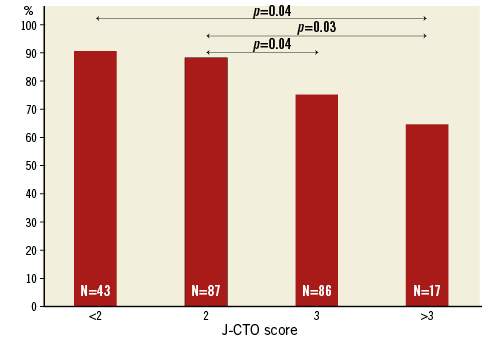
Figure 2. Success rates according to J-CTO score. The number of cases treated for different score values and the success rates for each value are shown and compared.
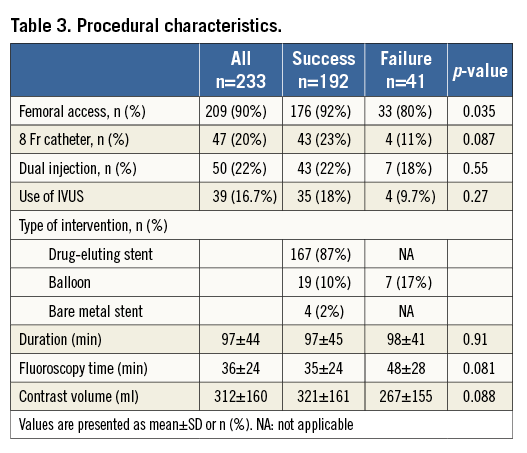
The procedural details are presented in Table 3. Only one CTO-ISR lesion was treated in each patient. The femoral access was more common in the successful group (92% vs. 80%, p=0.035), with a trend for higher usage of 8 Fr catheters. An antegrade crossing approach was used in 94% of cases and a retrograde approach (after failed antegrade) was attempted in 14 patients, being successful in 10 (71%). Polymer-coated wires (Whisper® ES or MS, Pilot 50, 150 or 200; Abbott Vascular, Santa Clara, CA, USA) and stiff non-tapered wires (Miracle 3 or 6 and ULTIMATEbros 3; Asahi Intecc, Aishi, Japan) were the more frequently used wires in the successful cases. No cases were carried out with the CrossBoss™ (Boston Scientific, Marlborough, MA, USA), mainly due to unavailabilty during the time period. In three cases, a Venture™ catheter (St. Jude Medical, St. Paul, MN, USA) was employed. In most cases, drug-eluting stents were used to treat the lesion. Seven cases treated with balloon angioplasty were considered failed cases. The use of IVUS was relatively low, but tended to be more frequent in successful cases. The success rate in those with IVUS performed during the procedure was 89.7%, and 80.1% in those without (p=0.2).
Among all variables, only the presence of tandem lesions (OR 0.19, 95% CI: 0.06-0.68; p=0.01) was identified as an independent predictor for the procedural outcome.
Complications occurred in 9.7% of procedures, coronary dissection in 5.2% and coronary perforation without pericardial tamponade in 4.5% of cases.
The median length of follow-up was 20 months (IQR 10-40). Clinical follow-up was completed in 203 patients (87%). No routine angiographic follow-up examination was carried out but the threshold for indicating angiography was not high, since 78 patients out of 192 successful cases (40.6%) had angiographic evaluation at follow-up and, among these, only 25 required TLR.
Survival curves for MACE and cardiac mortality are shown in Figure 3 and Figure 4. The incidence of MACE was comparable in both groups but a strong trend towards lower cardiac mortality was observed in the successful group (3% vs. 8.3%; p=0.09).
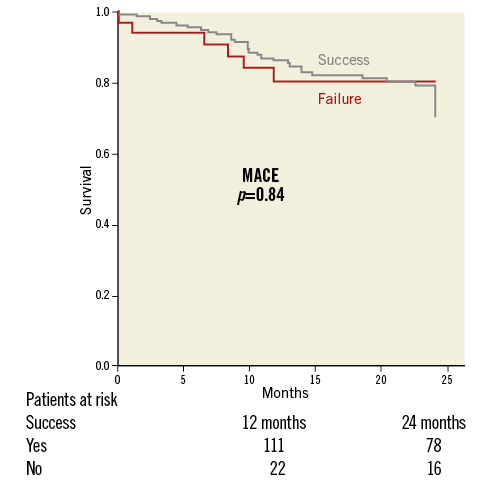
Figure 3. Cumulative incidence of MACE. Incidences of MACE (cardiac mortality, infarction and TVR) in successful and failed groups were quite comparable.
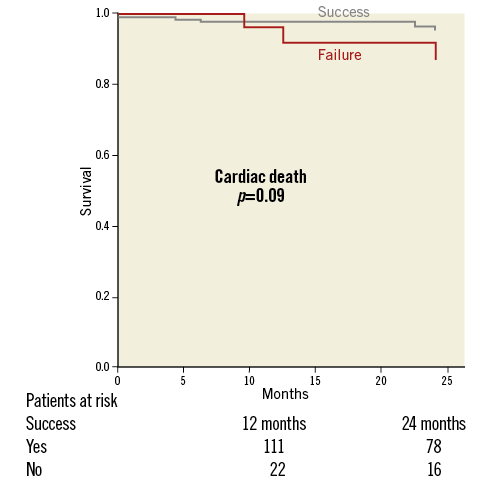
Figure 4. Cumulative incidence of cardiac mortality. A strong trend for lower cardiac mortality was observed in the successful group.
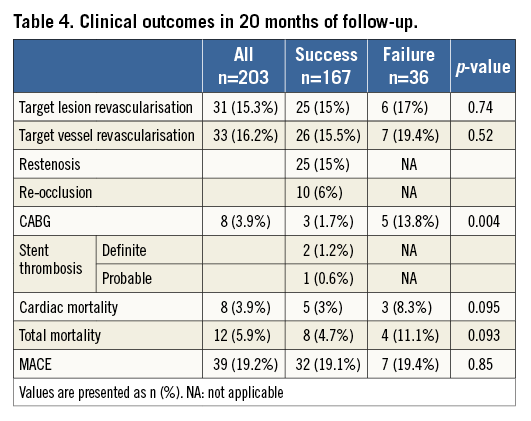
Major adverse cardiac events at 20 months are listed in Table 4. The need for subsequent CABG was significantly higher in the failed group. In the successful group TLR was 15% due to restenosis, which was occlusive in 40% of cases. The incidence of TLR in cases with IVUS performed during the index procedure was 11.2% and 13.9% in those without (p=0.6). No significant differences were observed according to the type (DES vs. BMS) of restenosed stent. Definite and probable thrombosis in this group was 1.8%. In all these thrombosis cases only one drug-eluting stent had been previously deployed at the site of the CTO-ISR, this being the left anterior descending artery, the one always involved.
The multivariant analysis for cardiac mortality showed a history of previous CABG (HR 8, 95% CI: 1.3-50; p=0.02) and multivessel disease (HR 2.3, 95% CI: 1.2-4.3; p=0.01) to be independent predictors.
Discussion
The main results of this registry are the following: a) compared with reported series, the success rate of CTO-ISR recanalisation was high (82.4%), despite a low usage of the retrograde approach and dedicated devices; b) circumflex artery loction, ostial CTO-ISR location and high J-score were related to failure, though only tandem occlusion was found to be an independent predictor; c) TLR was acceptable (15%), albeit frequently driven by re-occlusion; d) successful procedures were related to a strong trend towards lower cardiac mortality in long-term follow-up, but only previous CABG and multivessel disease were identified as independent predictors.
CTO lesions portend a challenge for the interventionalists. Successful rates have improved due to technological progress but are still highly dependent upon operator experience.
A limited amount of knowledge exists regarding treatment and outcomes of patients with CTO-ISR treated percutaneously, despite the fact that they constitute around 10-15% of all CTO PCI procedures1-3. This proportion is variable and depends on the time period and the centre. In our registry, the total number of CTO procedures was not available for the whole time period and for all centres. Reviewing the databases from some of the centres, over 500 CTO PCI cases, 5% corresponded to ISR.
Regarding the outcomes, the conclusions of previously published registries were hampered by their limited size, the largest including only 78 cases1-8. Furthermore, most of these registries were conducted in centres with highly skilled operators for CTO, and consequently employing a high rate of retrograde approach and specifically CTO-dedicated devices. Of note, all these registries were only focused on procedural results and no clinical outcomes were provided.
The success rates reported in the previously mentioned registries have usually been lower than those in CTO of native arteries1,3,5, except for a registry of highly experienced operators using complex techniques8 or very small series based on the use of dedicated devices2,4,6,7. Although inability to wire the occlusion was the primary mechanism of failure in these registries, inability to advance or fully dilate the balloon catheter used to be more common in CTO-ISR compared to CTO in the native artery1.
There are several potential explanations for the previously reported lower success rate for CTO-ISR lesions compared to non-ISR lesions. The pre-existing substrate of stented lesions with further development of ISR could be longer8, or more calcified12.
The presence of a prior stent could interfere with wire and balloon advancement through the CTO, particularly in the presence of underlying stent fracture or stent underexpansion (both acknowledged triggers of ISR) and marked tortuosity of the stented segment. Re-stenting may be hindered by trapping of the new stent in the struts of the prior stent13 or, in cases of subintimal crossing of the CTO, true lumen re-entry may be difficult. Finally, even after balloon crossing, optimal balloon expansion could be more difficult to achieve1. The reason for this would be the frequently underlying underexpanded stent and, in some cases, the densely fibrotic or calcified nature of in-stent plaques resulting from neoatherosclerosis.
The success rate in our registry (82.4%) appears to be higher than that reported in previous registries (63-71%)1,3,5, but slightly lower compared to studies based on specific devices such as the CrossBoss (87%)2, or registries of highly experienced operators using complex techniques (89.4%)8. A few very small series of cases (two to six) have been published describing results with the use of dedicated devices such as CrossBoss, FRONTRUNNER® XP (Cordis, Cardinal Health, Milpitas, CA, USA) or the combination of the Stingray™ catheter (Boston Scientific, Marlborough, MA, USA) and the Venture™ guidewire (St. Jude Medical) showing a 100% success rate4,6,7.
In the present registry only CTO-ISR were included, and direct comparison with de novo CTO is not possible. Nevertheless, using databases from some of the centres, the success rate for de novo CTO was 79% in that time period compared with the 82.4% observed for CTO-ISR. Restricting the analysis to the more recent period of time (since 2010), the success was almost the same, 85.7% and 85.4%, respectively.
Of note, the success rates experienced a sustained improvement along the time period of recruitment, from 76% to 85%. The success rates also varied according to centre, from 90% in the top performers to 75% in those with lower volume. Nevertheless, results of our registry may be generalisable to PCI settings where experience with percutaneous treatment of CTO is more variable, from high to more limited levels. The low rate of retrograde procedures (6%) could be explained by the good success of the antegrade approach in our series. Yet, we feel that the potential incremental value of the retrograde approach in CTO-ISR cannot be ascertained from a registry, since case selection bias is likely to occur in the current clinical scenario in which the penetration of the retrograde approach in overall PCI practice is still low.
With respect to variables related to procedural outcome, among all baseline factors, a lower body mass index, circumflex artery or ostial location, higher J-score and tandem lesions were linked to more failures. The proportion of patients with previous CABG was higher among failed cases but this difference did not reach statistical significance. With respect to the vessel involved, it is interesting to note that location of the CTO-ISR in the left circumflex artery was associated with less success, similarly to that observed with de novo CTO.
Despite the fact that the J-score was derived from an overall population of CTO lesions, and not specifically from CTO-ISR lesions, we included its use as indicative of CTO PCI complexity. Our results, showing a statistically significant association with procedural outcomes, support its value as a procedural score also in the setting of CTO-ISR.
In this regard, there are two variables included in the calculation of the J-score that deserve discussion when applied in this particular setting, calcification and angulation within the restenotic segment.
The process of neoatherosclerosis within the stent has been described extensively by means of in vivo studies (using OCT and IVUS) and by pathologic evaluations. This process accounts for the vast majority of late restenotic findings with BMS and DES. CTO-ISR used to be found later in time compared to non-CTO-ISR. In our registry, the mean time after index PCI was 1,632 days. Then again, neoatherosclerosis is the substrate of many cases of CTO-ISR rather than intimal proliferation alone. The component of calcification in neoatherosclerosis within a stent is not at all uncommon, as for atherosclerosis in de novo lesions14. In fact, cases with extensive and severe in-stent calcification have been reported15. In a registry of patients with CTO including 57 due to ISR, severe calcification was found in 5.3% of cases8. Furthermore, calcifications within 5 mm of stent edges are part of the restenotic lesion. In this registry, 16% of CTO-ISR presented a moderate or severe degree of calcification.
With respect to angulation, markedly angulated coronary diseased segments containing highly fibrocalcified plaques remain to some extent angulated even after stent implantation, not only because of the stiffness of the plaque components but because of the conformability of the stent platforms we have been using for the last 10 years. Moreover, angulations at the stent edges are part of the restenotic segment. A moderate or severe degree of angulation was found in 22% of lesions.
In the case of the circumflex artery, the angulated take-off of this vessel from the left main may decrease the pushability of wires through the lesion. In addition, more severe calcification was found in this vessel. However, only the presence of tandem occlusion was an independent predictor of procedural result. In other studies with a smaller sample size, a higher body mass index, longer time from implantation and larger stent diameter were identified as predictors of failure1,5. Regarding procedural features, only the use of the femoral access was significantly related with success. A trend was detected towards a higher success rate with 8 Fr catheters.
The use of IVUS was 16.7%, relatively low for lesions with these characteristics, but this rate is much higher than that reported in overall PCI practice in the USA and Europe. Detailed information about its use is not available for all cases but the indication for using IVUS was in most cases to guide crossing and secondarily to optimise stent implantation.
The incidence of complications was as low as in other registries and comparable to native CTO1,8. The long-term clinical outcomes, not available in previously published studies, showed a strong non-significant trend for lower cardiac mortality in the successful group. Lack of significance was probably related to the small size of the failed group. The difference in cardiac mortality between groups could be partially related to more CABG procedures required in the failed group.
In the successful group, with the vast majority of patients treated with a new drug-eluting stent, TLR was 15%. This figure is somewhat higher than that reported in series of CTO lesions on native arteries treated with drug-eluting stents, but it seems to be quite acceptable for occlusive ISR16. However, it is remarkable that 40% of recurrent restenosis presented as re-occlusions. The use of IVUS reduced numerically the incidence of TLR but numbers were low to draw meaningful conclusions in this regard.
A definite and probable thrombosis rate of 1.8% after a mean follow-up of 20 months also appears acceptable, taking into consideration the adverse lesion profile and the use of first-generation drug-eluting stents in the first years of the cohort.
Limitations
The CTO-ISR lesions included in this analysis were not all the lesions diagnosed but those in which an attempted percutaneous revascularisation was carried out in the 10-year period under consideration. The threshold for trying might have been variable according to operator experience but overall results are representative of the average practice.
On the other hand, a variation in success was observed along the 10-year time period of inclusion. In this regard, although we aimed to show the results of current practice on CTO-ISR in the drug-eluting stent era, we needed to collect a large number of cases. Thus, we extended the inclusion period from 2003 (introduction of drug-eluting stents in our practice) to 2013 (at least one year of follow-up), though most were included in the second half. Therefore, the study shows the success rate currently achieved and its evolution over the last 10 years.
The retrospective nature of the registry makes the performance of systematic or routine angiographic follow-up really difficult, or even unfeasible. On the other hand, in real practice it is unusual to perform routine angiographic follow-up after succesful PCI of CTO-ISR in otherwise asymptomatic patients experiencing an uneventful good clinical evolution after patency is restored. These patients had procedures carried out over the CTO-ISR because angina and/or ischaemia was found to be related to that specific lesion. Then, only those patients presenting recurrence of angina and/or ischaemia underwent recatheterisation and eventual TLR when indicated during follow-up. Anyway, the clinically driven angiographic evaluation rate during follow-up was relatively high (40.6%).
Angiographic characteristics were not analysed in a core lab but provided by local investigators from participating centres. Some patients were lost during follow-up. The time period of inclusion from 2003, the treatment of non-residents in the area of the centres or even from other countries (not uncommon in Spain) could explain this.
Conclusions
Percutaneous recanalisation of CTO due to ISR in contemporary practice shows a high success rate despite a low use of the retrograde approach and dedicated devices. Circumflex artery location, ostial lesions and high J-CTO score were related to failure, though only tandem occlusion was an independent predictor. TLR was not so high, albeit frequently driven by re-occlusion. Successful procedures were related to a strong trend towards lower cardiac mortality in long-term follow-up, but only previous CABG and multivessel disease were identified as independent predictors.
| Impact on daily practice This registry is the largest experience on CTO-ISR presented and the only one providing long-term follow-up. The study identifies the predictors of success and failure, the value of the J-CTO score in this context and the impact of results on long-term clinical outcomes. This information may be helpful in the management of these patients. |
Conflict of interest statement
The authors have no conflicts of interest to declare.