Abstract
Aims: We sought to compare the efficiency of the novel EuroCTO (CASTLE) score with the commonly used Multicentre CTO Registry in Japan (J-CTO) score in predicting procedural success of percutaneous coronary intervention (PCI) for coronary chronic total occlusions (CTOs).
Methods and results: We evaluated 660 consecutive CTO PCIs (mean age 66±11 years, 84% male). The mean J-CTO and EuroCTO (CASTLE) scores were 1.86±1.2 and 1.74±1.2, respectively. Antegrade wire escalation, antegrade dissection re-entry and retrograde approach were used in 82%, 14% and 37% of cases, respectively. Receiver operating characteristic analysis demonstrated equal overall discriminatory capacity between the two scores (AUC 0.698, 95% CI: 0.653-0.742, p<0.001 for J-CTO vs AUC 0.676, 95% CI: 0.627-0.725, p<0.001 for EuroCTO; AUC difference: 0.022, p=0.5). However, for more complex procedures (J-CTO ≥3 or EuroCTO [CASTLE] ≥4]), the predictive capacity of the EuroCTO (CASTLE) score appeared superior (AUC 0.588, 95% CI: 0.509-0.668, p=0.03 for EuroCTO [CASTLE] score vs AUC 0.473, 95% CI: 0.393-0.553, p=NS for the J-CTO score, AUC difference: 0.115, p=0.04).
Conclusions: In this study, the novel EuroCTO (CASTLE) score was comparable to the J-CTO score in predicting CTO PCI outcome with a superior discriminatory capacity for the more complex cases.
Introduction
Coronary chronic total occlusions (CTOs), defined as coronary lesions with Thrombolysis In Myocardial Infarction (TIMI) grade 0 flow of at least three months duration, are a common finding in patients undergoing invasive diagnostic angiography1,2,3. Over the last decade, the advent of novel techniques and the utilisation of more advanced equipment has resulted in high procedural success rates and an upsurge in the number of CTO percutaneous coronary interventions (PCIs) performed4,5. However, the success of CTO interventions can still vary significantly, especially in unselected populations6 and, apart from lesion complexity and operator experience, it is also liable to several additional factors including patients’ clinical characteristics.
Preprocedural preparation, involving careful identification of various clinical risk factors and meticulous assessment of the diagnostic coronary angiogram to evaluate lesion complexity and plan the procedural strategy, is important to achieve successful outcomes in CTO PCI7. Success prediction scores are valuable in this regard, as they provide a quantitative evaluation of procedural difficulty and the likelihood of recanalisation success and thus facilitate case selection, procedural planning and clinical decision making7. The novel EuroCTO (CASTLE) scoring system has recently been derived and validated from the large multicentre EuroCTO registry including more than 20,000 patients. It comprises two clinical factors (age ≥70 years and previous coronary artery bypass graft [CABG] surgery) and four angiographic factors (blunt or invisible proximal cap, severe tortuosity, severe calcification and lesion length ≥20 mm) with one point for each factor, resulting in a minimum score of 0 to a maximum score of 68. We sought to compare the technical success predictive efficacy of the novel EuroCTO (CASTLE) score with the widely adopted Multicentre CTO Registry in Japan score9.
Methods
We analysed 660 consecutive CTO PCI cases performed in a tertiary cardiac centre with a dedicated CTO programme (Essex Cardiothoracic Centre, Basildon, United Kingdom). All cases performed since the onset of the programme in June 2012 up to November 2018 were included in the analysis. As part of the programme and for auditing purposes, clinical, angiographic and procedural characteristics of the CTO cases were prospectively recorded in a dedicated CTO database. The J-CTO and EuroCTO (CASTLE) scores were calculated according to the algorithms described by Morino et al9 and Szijgyarto et al8, respectively. The EuroCTO (CASTLE) score analysis took place retrospectively as the score was introduced only recently. The definitions of the EuroCTO and J-CTO score variables and the different recanalisation techniques can be found in Supplementary Appendix 1-Supplementary Appendix 3 and Supplementary Table 1.
Technical success of CTO PCI was defined as successful CTO revascularisation resulting in <30% residual vessel diameter stenosis within the treated segment and restoration of TIMI grade 3 antegrade flow.
STATISTICAL ANALYSIS
All quantitative variables were tested for normal distribution according to the Kolmogorov-Smirnov test. Continuous variables are reported as mean and SD values. Categorical variables are expressed as frequency and proportion. Normally distributed continuous variables were compared using the Student’s t-test, whilst the Mann-Whitney U test was used to compare non-normally distributed continuous variables. Categorical data were compared using the Pearson chi-squared test. To evaluate the trend of efficiency metrics amongst different prediction score strata, the Jonckheere-Terpstra statistical test was applied. The association between prediction scores and technical outcome was evaluated using the univariate logistic regression analysis and their efficiency as independent factors for predicting successful outcomes in CTO PCI was evaluated using a multivariate logistic regression model accounting for various potential confounding factors. Odds ratios for every one-point increase of the J-CTO and the EuroCTO (CASTLE) scores with their respective 95% confidence intervals were calculated. The Hosmer-Lemeshow goodness-of-fit (HL) test was used to assess calibration of both scores in our study population. The HL test analyses the observed versus the predicted outcomes; theoretically, there should not be any statistically significant difference between the expected and observed counts and thus, based on χ2 distribution, an HL statistic with a p-value >0.05 should be consistent with a good model fit10. The discriminatory performance of the predictive scores was evaluated by comparing the two scores using the receiver operating characteristic (ROC) curve and area under the curve (AUC) analysis. Differences in AUC between ROC curves were tested as described by Hanley & McNeil11. Statistical analysis was performed with SPSS, Version 24.0 (IBM Corp., Armonk, NY, USA). A two-tailed p-value of <0.05 was considered statistically significant.
Results
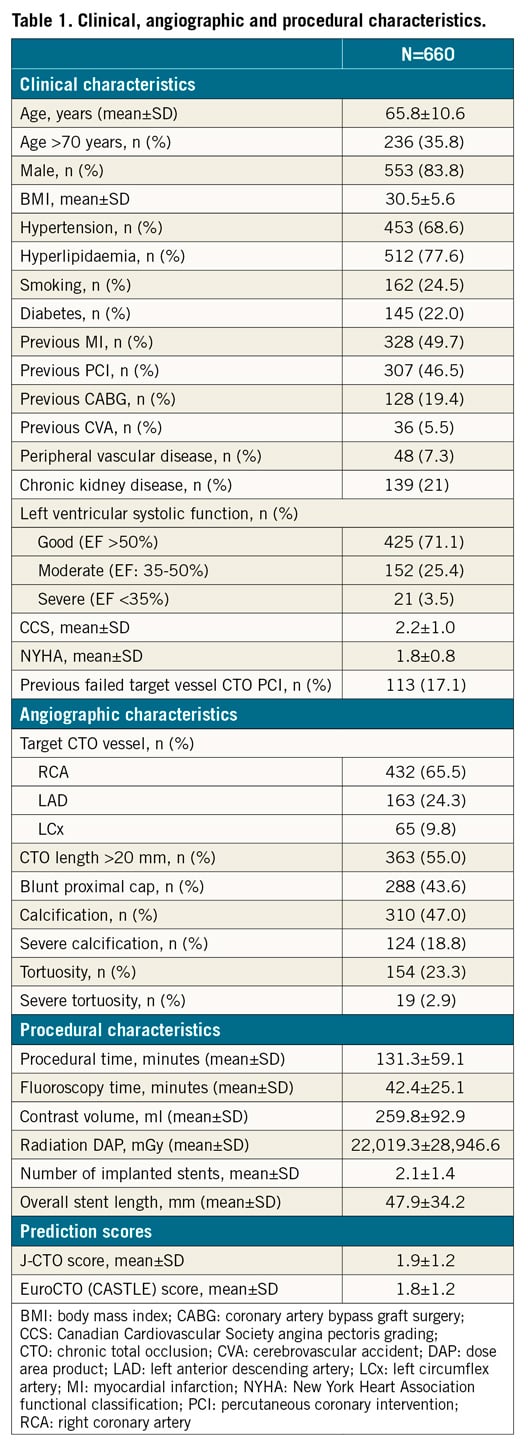
The study included 660 CTO PCIs (mean age 65.8±10.6 years, 83.8% male). Table 1 shows the clinical, angiographic and procedural characteristics of the study cases. The indication for CTO PCI was stable angina pectoris in all cases; the most common target PCI vessel was the right coronary artery (66%). More than 30% of the study participants were ≥70 years old and 19% had a history of previous CABG. An antegrade wire escalation (AWE) approach was the most frequent recanalisation approach: it was applied as an initial strategy in 73.9% of cases followed by the retrograde approach (RA) in 20.4% of cases and antegrade dissection and re-entry (ADR) in 5.8% of cases. The overall prevalence of AWE, RA and ADR was 82%, 37% and 14%, respectively. Successful CTO recanalisation was achieved in 516 cases (78%). Amongst cases with successful CTO PCI, AWE was the successful recanalisation strategy used in 67% of cases, RA was used in 22% of cases and ADR in 11% of cases. The mean EuroCTO and J-CTO scores were 1.8±1.2 and 1.9±1.2, respectively. Failed cases had significantly higher EuroCTO (CASTLE) and J-CTO scores compared to cases with successful CTO PCI (2.4±1.2 vs 1.6±1.2, p<0.001, and 2.5±1.0 vs 1.7±1.2, p<0.001, respectively).
The EuroCTO (CASTLE) score exhibited superior calibration compared to the J-CTO score in our sample analysis: EuroCTO (CASTLE) score HL χ2=0.765, p=0.858, and J-CTO score HL χ2=17.397, p=0.001. In the multivariate logistic regression analysis, both the EuroCTO (CASTLE) and J-CTO scores were the only independent predictors of successful CTO PCI. For each unit increase of the EuroCTO (CASTLE) and J-CTO scores, there was a 28% and 36% odds reduction for successful recanalisation, respectively (Table 2). Technical success was significantly lower for higher values of both scores (Figure 1A, Figure 1B); the probability of successful PCI was inversely correlated with both score strata (Figure 1C, Figure 1D). The most pronounced difference in success rates of approximately 54% between the lowest scoring grade (least complex cases) and the highest scoring grade (most complex cases) was observed in the EuroCTO (CASTLE) score (Figure 1B). The J-CTO score was associated with an overestimation of case complexity compared to the EuroCTO (CASTLE) score as a J-CTO score ≥3 was observed in 30% and a EuroCTO (CASTLE) score ≥4 in 9% of cases (Figure 1C, Figure 1D).
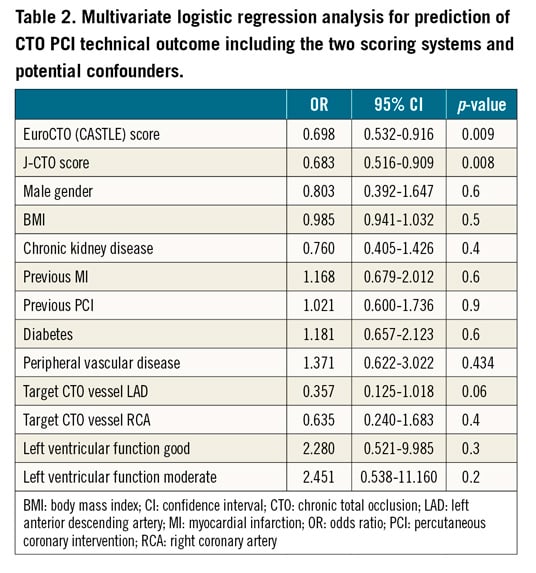
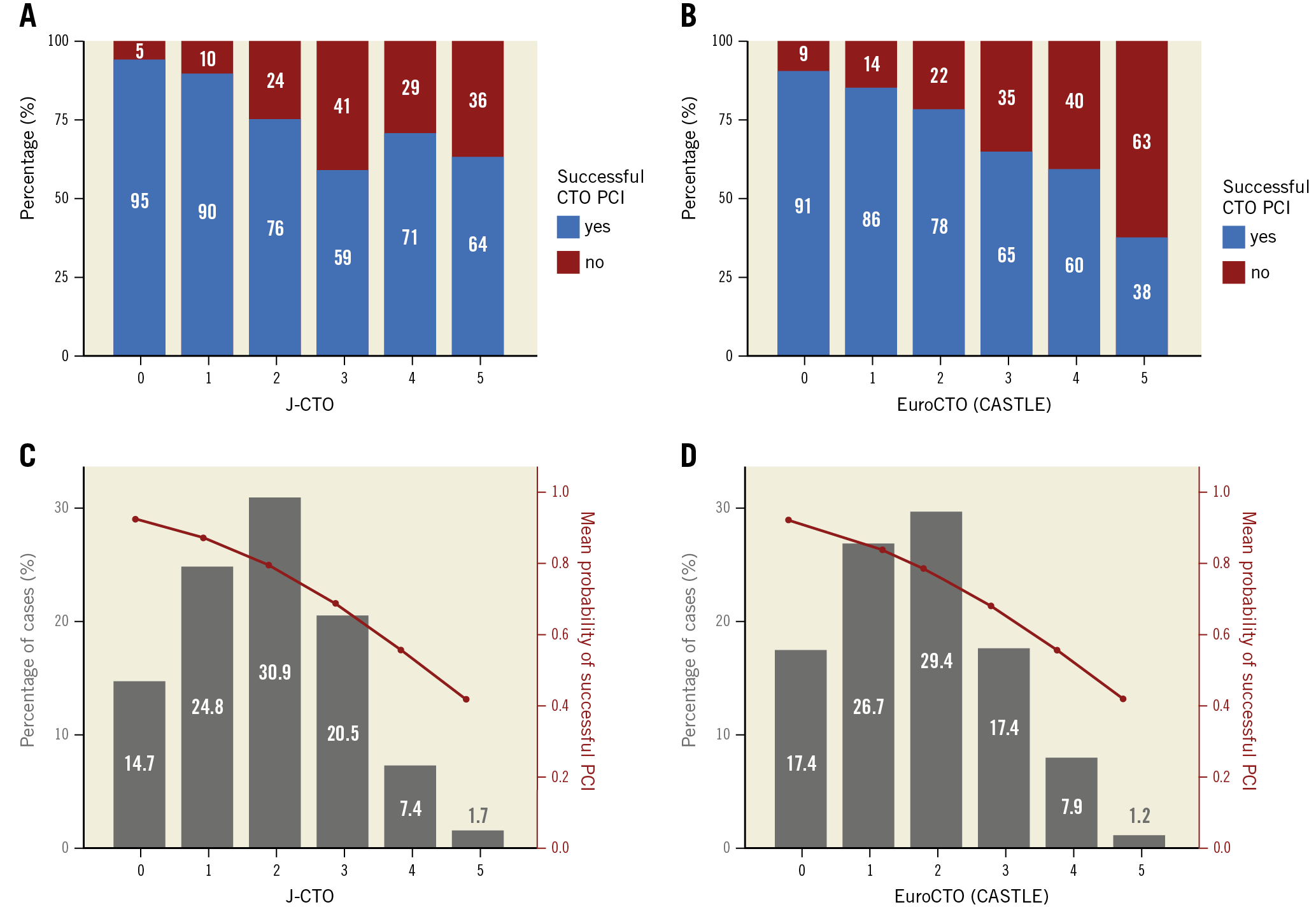
Figure 1. Rates of technical success and J-CTO and EuroCTO (CASTLE) scores strata. A) Observed rates of technical success of CTO PCI across J-CTO score strata. B) Observed rates of technical success of CTO PCI across EuroCTO (CASTLE) score strata. C) Distribution of J-CTO score strata across study cases. The red line demonstrates the predictive mean probability of successful CTO PCI according to the J-CTO score stratification. There is an evident discrepancy between the observed (panel A) and predicted success rates (red line) in the more complex cases with a J-CTO score of ≥3. D) Distribution of EuroCTO (CASTLE) score strata across study cases. The red line demonstrates the predictive mean probability of successful CTO PCI according to the EuroCTO (CASTLE) score stratification. The EuroCTO (CASTLE) score depicts a good agreement between the observed (panel B) and the predicted success rates (red line) across all score strata.
The discriminatory performance of the two scoring systems in predicting the technical outcome of CTO PCI was evaluated using the ROC curve analysis. Both scores demonstrated equal overall discriminatory capacity: for the EuroCTO (CASTLE) score, AUC 0.674, 95% CI: 0.625-0.724, p<0.001, for the J-CTO score, AUC 0.694, 95% CI: 0.649-0.739, p<0.001, AUC difference: 0.02, p=NS (Figure 2A). However, for the more complex procedures (EuroCTO [CASTLE] score ≥4 or J-CTO score ≥3), the discriminatory capacity of the EuroCTO (CASTLE) score to predict procedural success appeared superior compared to the J-CTO score (AUC 0.588, 95% CI: 0.509-0.668, p=0.03 for EuroCTO [CASTLE] score vs AUC 0.473, 95% CI: 0.393-0.553, p=NS for J-CTO score, AUC difference: 0.115, p=0.04) (Figure 2B). In the univariate logistic regression analysis, both scores appeared to have better predictive efficacy for the less complex cases with a J-CTO score of <3 and EuroCTO (CASTLE) score <4 (Table 3). We analysed the discriminatory capacity of the two scoring systems across the very early (2012-13) and very late (2017-18) periods of time of our study. The EuroCTO (CASTLE) and J-CTO scores demonstrated a consistent and satisfactory discriminatory capacity over time (AUC 0.740, 95% CI: 0.657-0.882, p<0.001 vs AUC 0.733, 95% CI: 0.579-0.886, p=0.007, and AUC 0.723, 95% CI: 0.641-0.805, p<0.001 vs AUC 0.699, 95% CI: 0.564-0.834, p=0.021, respectively) (Figure 3).
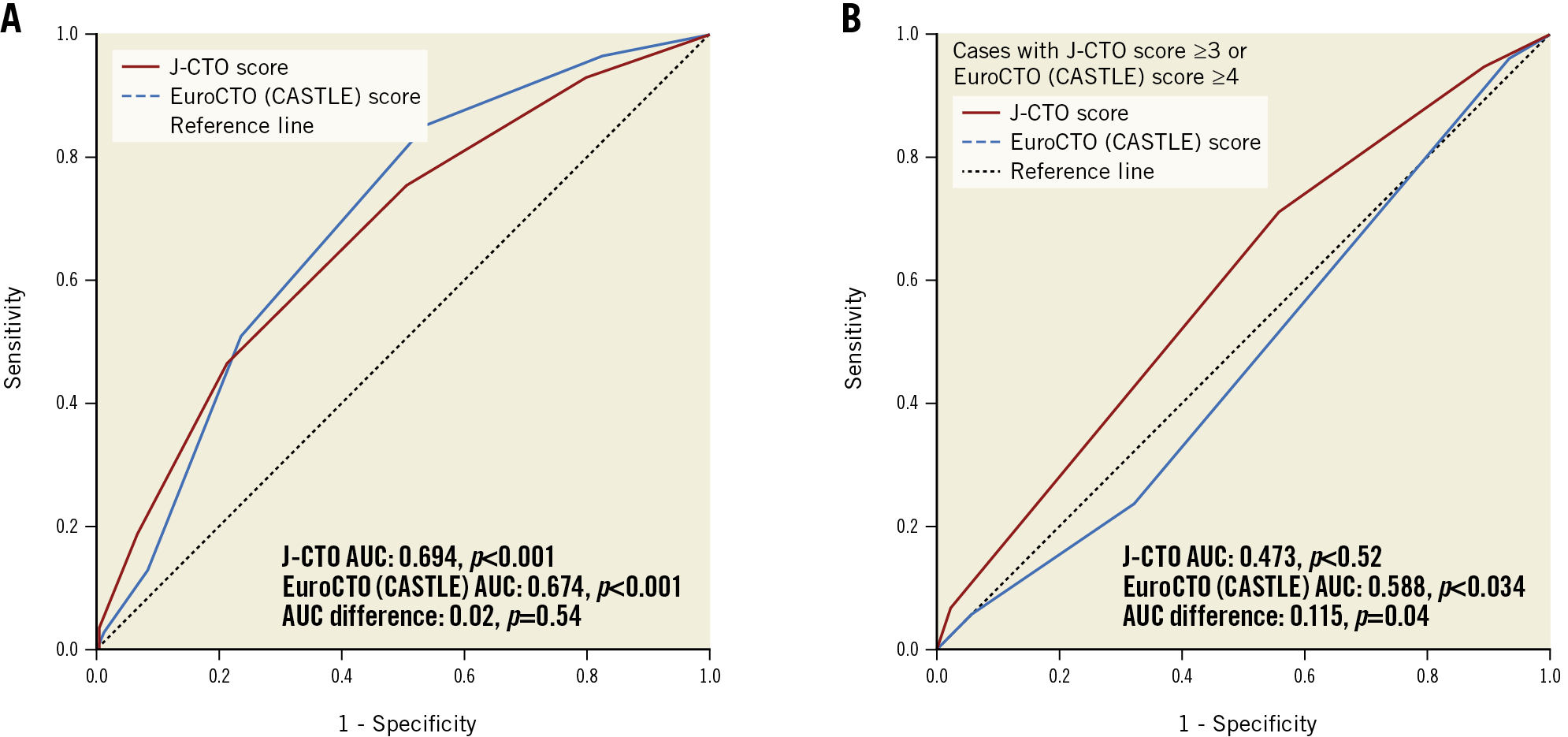
Figure 2. ROC curves for success prediction for the J-CTO and the EuroCTO (CASTLE) scores. A) In the whole study cohort. B) In the more complex cases with J-CTO score ≥3 or EuroCTO (CASTLE) score of ≥4. ROC: receiver operating characteristic
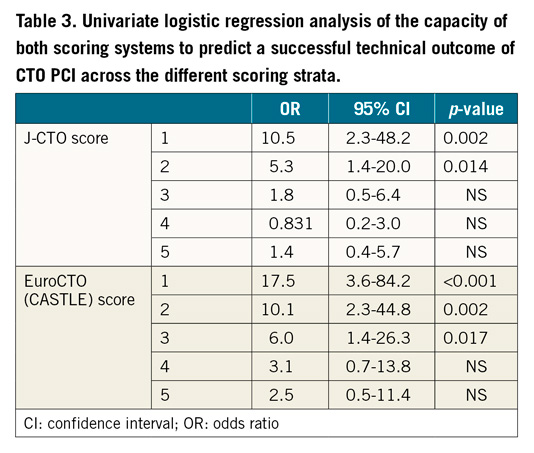
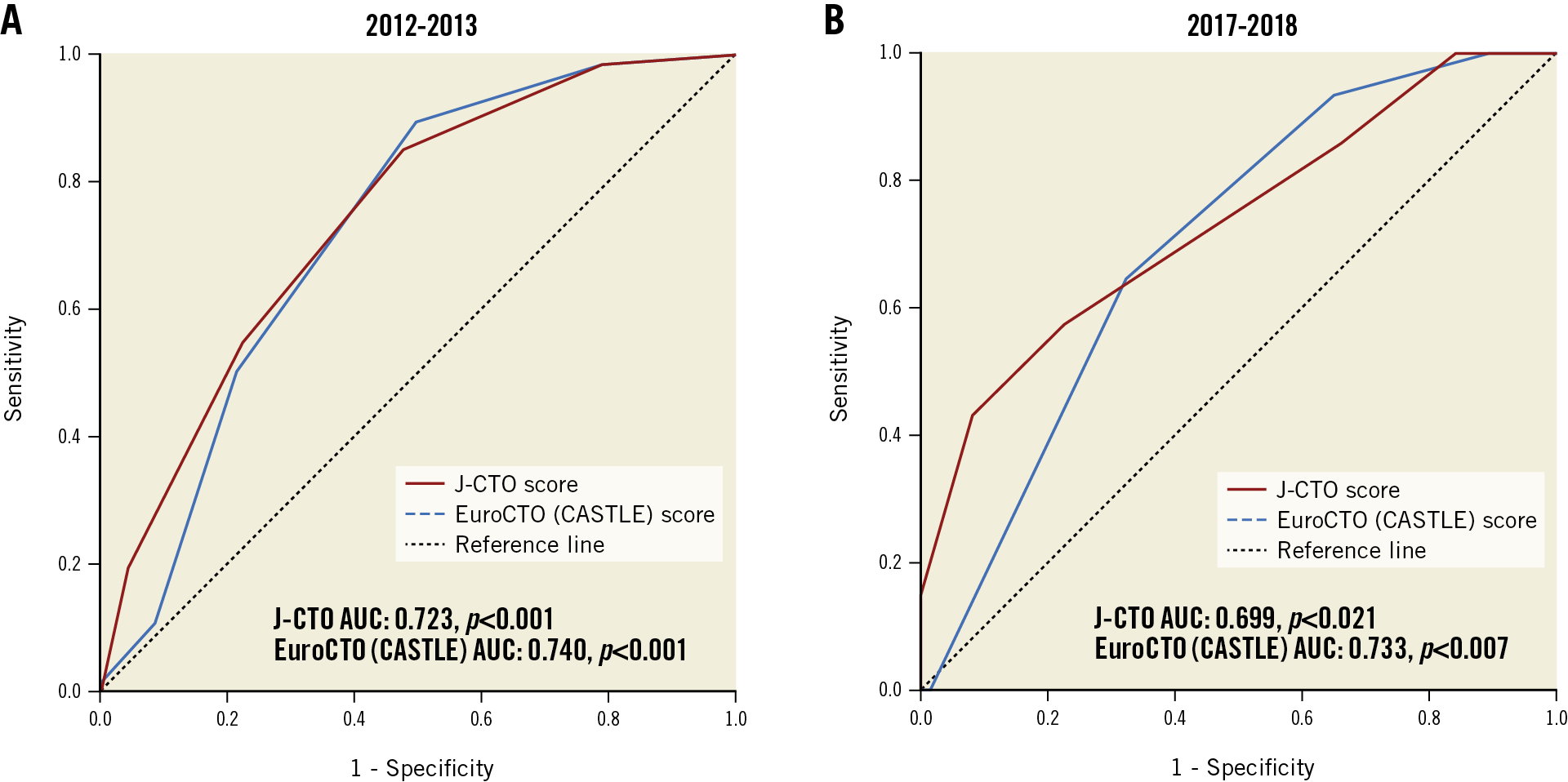
Figure 3. ROC curves for success prediction for the J-CTO and the EuroCTO (CASTLE) scores in the study cohort between the years 2012 and 2013, and 2017 and 2018. A) 2012-2013. B) 2017-2018. ROC: receiver operating characteristic
Successful recanalisation with an AWE approach was predominant in the lower strata of both scores, whereas in more complex cases successful recanalisation through the RA or ADR approach was more frequently observed (Figure 4). Moreover, there was significantly higher radiation dose area product, contrast volume administration, overall procedural time and fluoroscopy time amongst the higher strata of both scores according to the trend analysis (Figure 5).
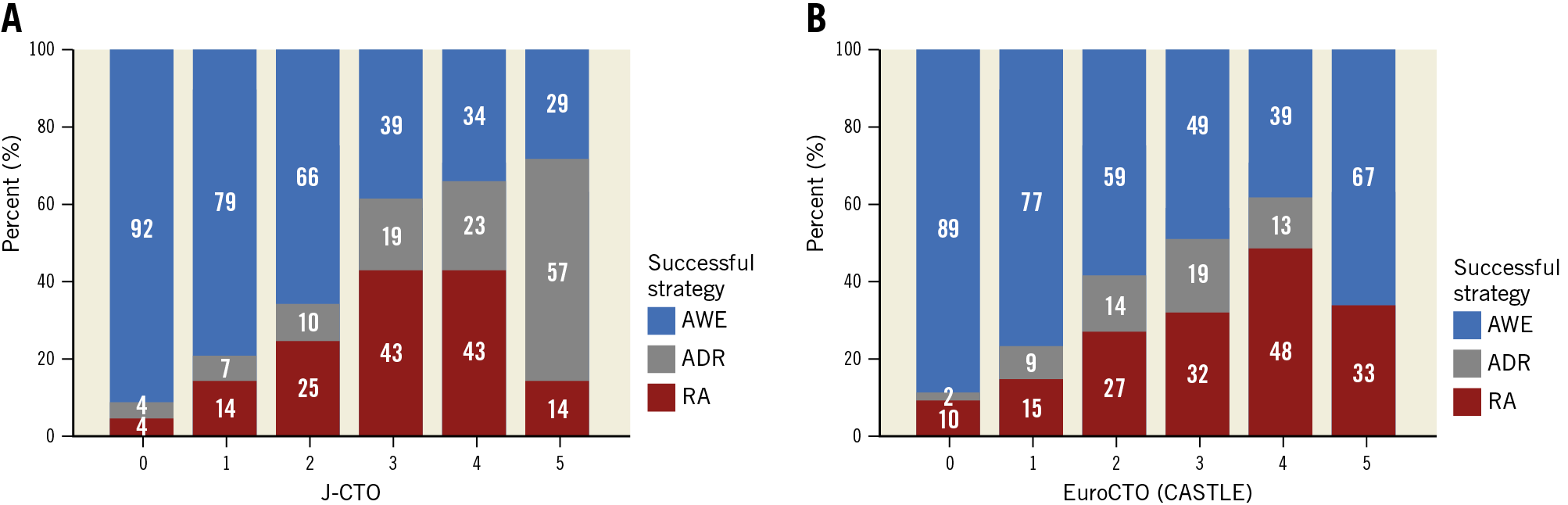
Figure 4. Rates of successful techniques across J-CTO and EuroCTO (CASTLE) score strata. A) J-CTO score strata. B) EuroCTO (CASTLE) score strata.
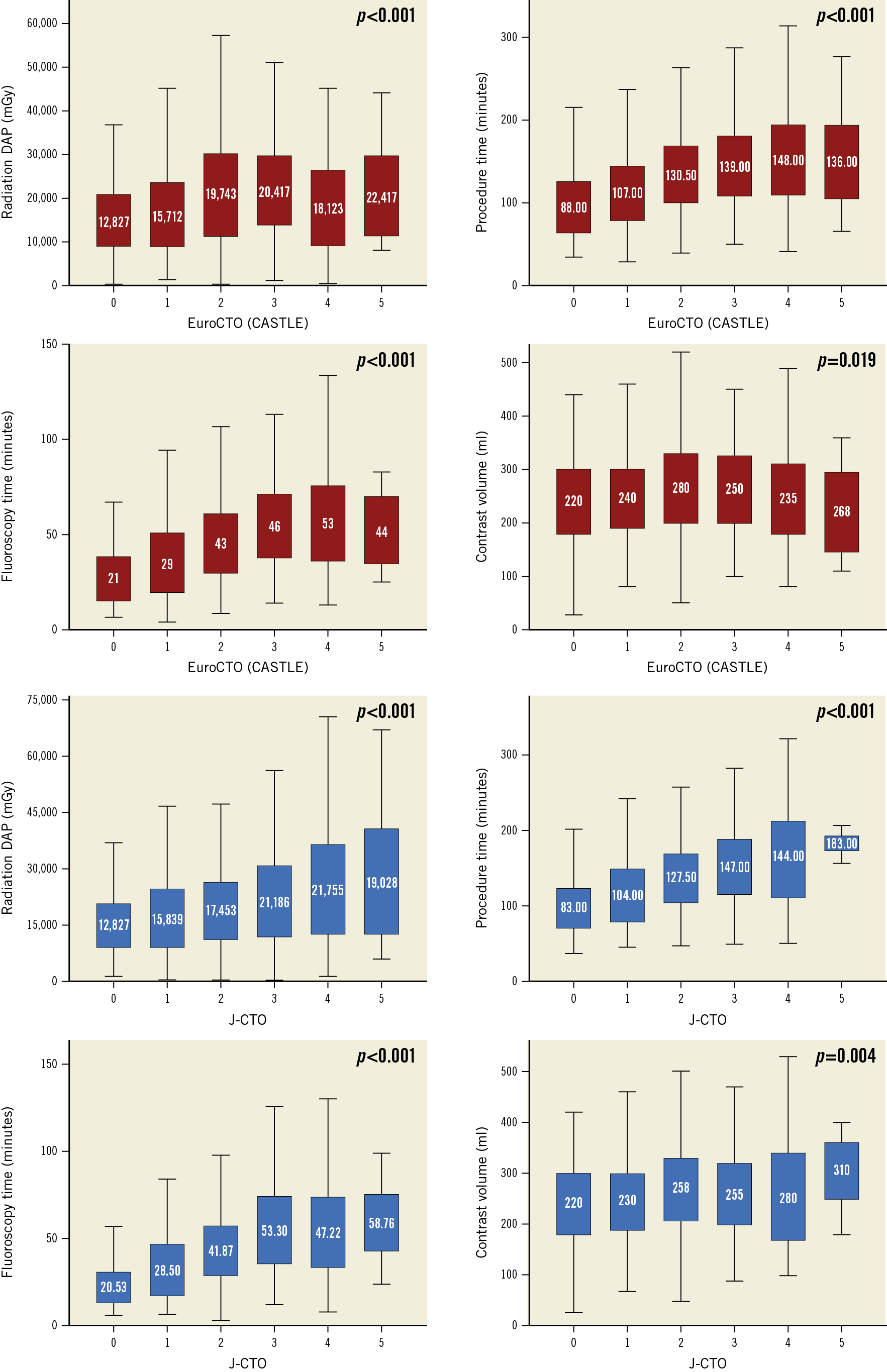
Figure 5. CTO PCI efficiency metrics including contrast volume, radiation dose area product, fluoroscopy and procedural time across the J-CTO score and EuroCTO (CASTLE) score strata.
Discussion
The present study compared the efficiency of the novel EuroCTO (CASTLE) score with the widely adopted J-CTO score to predict the technical outcome of CTO PCIs in an unselected cohort of patients treated with contemporary CTO techniques. Our results showed that the EuroCTO (CASTLE) score demonstrated an overall equal predictive performance with the J-CTO score. However, the EuroCTO (CASTLE) score appeared superior in predicting the technical outcome in the more complex cases.
The ability to appraise case complexity and predict outcomes reliably is a favourable concept that can facilitate CTO PCI in various ways. Firstly, it could ease the process of determining the appropriateness of CTO PCI by evaluating the overall risk-benefit ratio of the procedure12. Secondly, it could help interventional cardiologists during the early stages of their training in CTO PCI to select simpler cases and either refer the more complex cases to more experienced operators or perform these with proctor support. Furthermore, objective quantification of lesion complexity allows careful procedural planning, which is an essential step before attempting CTO recanalisation both for experienced and for non-experienced CTO PCI operators. Finally, determining case complexity, technical outcomes and efficiency metrics could help to evaluate the overall performance of a dedicated CTO programme, identify pitfalls and help to improve performance and quality measures further.
So far, various predicting scoring systems have been developed9,13,14,15,16. These scores have been derived from registries that predominantly included a relatively modest number of patients. Additionally, across the different registries there was great variance regarding the adopted recanalisation techniques, CTO PCI success rates, patients’ clinical characteristics, case complexity and operator skills, making these scores unattractive for more generalised adoption. The most commonly used score – the J-CTO score – was derived from a cohort of 465 patients treated exclusively with the antegrade approach between 2006 and 20079. The endpoint in that study was successful guidewire crossing within 30 minutes, which was achieved in 48% of the cases.
The EuroCTO group recently reported the development and validation of a novel CTO PCI success prediction scoring system, the EuroCTO (CASTLE) score. The potential advantages of this prediction score are the large derivation and validation cohort consisting of an unselected and contemporary population of more than 20,000 cases, the homogeneous distribution of operator experience with the majority of the operators performing >50 CTO PCIs/year and the utilisation of a broad spectrum of contemporary CTO PCI techniques and equipment. In our study, we compared the EuroCTO (CASTLE) score with the J-CTO score, as the latter is the score most commonly used to assess the complexity of CTO PCIs. The EuroCTO (CASTLE) score demonstrated an overall equal discriminatory capacity with the J-CTO score. However, the EuroCTO (CASTLE) score showed superior calibration and had better predictive performance than the J-CTO score in the more complex cases. The noticeably large number of patients who were included in the original derivation cohort of the EuroCTO (CASTLE) score and the inclusion of additional objective clinical features such as prior history of CABG and patients’ age potentially improved the ability of the EuroCTO (CASTLE) score to predict the technical outcome in more complex CTO PCIs. Elderly patients and those with a prior history of CABG are likely to have more comorbidities and diffuse and complex atherosclerotic disease that can increase case complexity and thus result in a higher likelihood of unsuccessful outcomes17,18. In contrast to the J-CTO score, in the EuroCTO (CASTLE) score a previously failed attempt was not incorporated in the final prediction model. This parameter is subject to the operator’s technical expertise. Less experienced operators are more likely to fail, simply because they do not master all recanalisation techniques and thus have limited options to tackle more difficult CTOs, whilst a more experienced operator might have succeeded at the first attempt. Therefore, for an operator with a good level of CTO PCI experience, a previously failed attempt does not necessarily translate into a more complex procedure or increased chances of failure. In addition, the utilisation of the currently expanded armamentarium of dedicated CTO equipment and the implementation of more advanced recanalisation techniques compared to those used in the derivation cohort of the J-CTO score might have blunted the impact of CTO complexity assessed by the J-CTO score and could at least in part explain the inconsistency that we observed in the predictive efficiency in the more complex cases. Finally, although the discriminatory capacity of the EuroCTO (CASTLE) score was superior in the higher complexity subgroup, it was reduced compared to the overall population (AUC 0.588 vs 0.674, respectively).
In our study, the EuroCTO (CASTLE) score demonstrated an almost identical discriminatory capacity with that of the original derivation cohort from the EuroCTO registry (AUC of 0.67 and 0.66, respectively). In our analysis, we included consecutive CTO cases from day 1 of a dedicated CTO PCI programme, thus incorporating all stages of a contemporary CTO PCI learning curve. Therefore, we provide evidence that the EuroCTO (CASTLE) score is generalisable, with excellent reproducibility in different CTO populations and across variable CTO PCI expertise and contemporary CTO PCI modalities.
Higher grades of both scores were associated with significantly higher levels of several procedural efficiency metrics such as radiation exposure, contrast volumes, procedural and fluoroscopy times, in keeping with findings of previous studies19. Beyond the actual predictive ability of technical success, the CTO PCI scoring systems might be advantageous by assisting angiographic review, estimating procedure and lesion complexity and evaluating efficiency metrics, all of which can be valuable components of a comprehensive and universal approach to clinical decision making. Given the higher potential for complications, the decision to proceed with CTO revascularisation must be based on a meticulous risk-benefit assessment and an uncluttered discussion with both the patient and the Heart Team.
Limitations
A few limitations of this study warrant further discussion. The study is limited by its observational design and, even though the population was unselected with enrolment of consecutive patients undergoing CTO PCI, it could be subject to operators’ case selection bias especially during the early stages of the dedicated CTO programme. However, the inclusion of cases from the early stages of the programme, when the operators’ experience was more limited, enhances the capacity of extrapolating the study results to other populations that encompass a broad spectrum of case difficulty and operator technical experience. Angiographic parameters were assessed by the operators without adjudication from a core laboratory, although we think it is unlikely that the major findings would have been any different as all operators were participating in a dedicated CTO programme and have substantial theoretical and practical knowledge regarding all aspects of CTOs. Finally, it is worth mentioning a limitation not of our study, but of any outcome predicting score. Predicting scores are useful for estimating lesion complexity and planning procedural strategy and use of equipment, but it is impossible to generate a flawless model with a perfect predictive capacity. Clinical judgement and operator experience cannot be substituted by any prediction model and are the most important factors for determining a successful and uneventful procedure.
Conclusions
In conclusion, the EuroCTO (CASTLE) score demonstrated similar performance to the J-CTO score in predicting the success of CTO PCI with potentially better discriminatory capacity in more complex cases. Both scores were associated with higher values of procedural efficiency measures and could thus assist with preprocedural planning and risk-benefit assessment.
|
Impact on daily practice Percutaneous revascularisation of chronic total occlusions represents the most challenging procedure in the field of coronary interventions. In this setting, technical outcome prediction scores are useful in preprocedural planning of CTO percutaneous revascularisation. The novel EuroCTO (CASTLE) score, derived from the large EuroCTO registry, could be used as an alternative to the commonly applied J-CTO score, as it shows similar overall capacity in predicting CTO PCI success rates with a superior discriminatory capacity for the more complex cases. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.