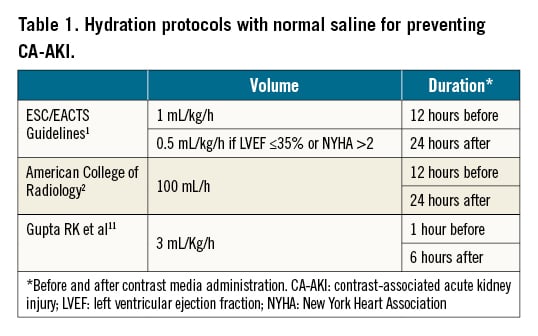
Intravenous hydration is the standard of care for preventing contrast-associated acute kidney injury (CA-AKI) in patients undergoing invasive cardiovascular procedures12. However, the type of solution, the volume and the timing of administration are still a matter of debate. Intravascular volume expansion is usually accomplished by the administration of isotonic saline. Several hydration protocols have been reported and recommended (Table 1).
Sodium bicarbonate has been proposed as an alternative solution to prevent CA-AKI3. One potential mechanism of kidney protection is the alkalinisation of the renal tubular fluid and the scavenging of reactive species generated from nitric oxide. Free radical formation is promoted by an acidic environment typical of tubular urine but is inhibited by the higher pH of normal extracellular fluid. Sodium bicarbonate has been compared with isotonic saline in several randomised trials with conflicting results3456. The most definitive data are from the Prevention of Serious Adverse Events Following Angiography (PRESERVE) randomised trial, which included 4,993 high-risk patients undergoing scheduled angiography and found that both treatments were associated with similar outcomes7.
In the current issue of EuroIntervention, Lombardi et al report on the PrevenTion of contrast-inducEd nephropAThy with urinE alkalinisation (TEATE) prospective, randomised, open-label trial to test the hypothesis that an alkaline urine status with either oral or intravenous (i.v.) bicarbonate on top of hydration alone prevents CA-AKI8. The authors compared 1) saline hydration alone; 2) i.v. bicarbonate; and 3) oral bicarbonate, in patients with chronic kidney disease scheduled for the intra-arterial contrast media (CM) administration. The primary endpoint was the incidence of CA-AKI according to alkaline urine status achieved immediately before angiography. Secondary endpoints were the mean change in urine pH up to the time of angiography and the incidence of CA-AKI in the 3 groups. Patients achieving a pH >6 before angiography had significantly lower incidences of CA-AKI compared with the others (odds ratio 0.48, 95% confidence interval: 0.25-0.90; p=0.023). The proportion of patients achieving a pH >6 was significantly higher in the i.v. and oral bicarbonate groups compared with hydration alone. The incidence of CA-AKI, however, was not significantly different in the 3 treatment arms.
The authors conclude that urinary pH before CM administration is an inverse correlate of CA-AKI incidence, and bicarbonate is superior to hydration alone in achieving urinary alkalinisation. However, bicarbonate did not reduce the incidence of CA-AKI. Although being a confirmatory study, which reaffirms the lack of superiority of sodium bicarbonate solution versus sodium chloride solution in CA-AKI prevention, the TEATE trial emphasises an important new concept in the field of CA-AKI prevention. Sodium bicarbonate solution might be superior to normal saline only in patients with a baseline urine pH <6. The pH of urine ranges from 4.5 to 8, depending upon the systemic acid-base balance. The median pH of human 24-hour urine is ∼69. A low urine pH has been found as a predictor of chronic kidney disease10. In the REMEDIAL trial, baseline urine pH was <6 in approximately 17% of patients5. Further studies that only include patients with a baseline urine pH <6 are needed to clarify this concept.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.