Abstract
Aims: To assess the main predictors and significance of filter no-reflow (FNR) in protected saphenous vein graft (SVG) percutaneous coronary intervention (PCI) and the effect of two different filter-based devices on FNR incidence. The phenomenon of FNR has been described as a transient impairment of blood flow due to debris plugging of a filter-based device used to shield the distal microvasculature during SVG PCI.
Methods and results: Fifty consecutive patients treated with SVG PCI were enrolled, using two different filter-based devices (FilterWire EZ™ [Boston Scientific, Natick, MA, USA] and SpiderRX® [Ev3, Plymouth, MN, USA]). We evaluated: 1) the value of clinical and angiographic variables for predicting FNR including the recently-described “degeneration score” (DS); 2) the predictive value of FNR for post-procedural (type IVa) myocardial infarction (MI); 3) the effect of filter type on incidence of FNR. FNR was observed in 30% of patients and was predicted by a higher DS at baseline (2.1±0.9 vs. 1.4±0.8, p=0.02, respectively) as well as by the type of filter used (54% vs. 23% in SpiderFX and FilterWire EZ, respectively, p=0.04). However, at multivariate analysis DS was the only independent predictor of FNR (OR 2.47, CI 95% 1.06-5.76, p=0.04). Graft age and FNR were found to be independent predictors of type IVa MI (OR 1.28; CI 95% 1.01-1.64, p=0.04 and OR 15.69; CI 95% 2.12-116.39, p=0.007, respectively).
Conclusions: FNR is a common complication of protected SVG stenting. FNR occurs mainly in grafts with a high degeneration score, and the presence of FNR predicts post-procedural myocardial infarction.
Abbreviations
CABG: coronary artery bypass graft
CI 95%: confidence interval 95%
CRP: C-reactive protein
cTFC: corrected TIMI frame count
DS: degeneration score
FNR: filter no-reflow
MACE: major cardiac events
MI: myocardial infarction
MLD: minimal lumen diameter
NSTE-ACS: non-ST-elevation acute coronary syndromes
NSTEMI: non-ST-elevation myocardial infarction
OR: odds ratio
PCI: percutaneous coronary intervention
QCA: quantitative coronary angiography
RVD: reference vessel diameter
SVG: saphenous vein graft
TIMI: Thrombolysis In Myocardial Infarction
TnT: troponin T
Introduction
Within 10 years of coronary artery bypass graft surgery (CABG) approximately one–half of all saphenous vein grafts (SVG) are occluded or re-present with critical lesions1. Redo-CABG is burdened by high complication rates and mortality2,3. Percutaneous coronary intervention (PCI) to SVG is thus frequently performed. SVG PCI, however, represents one of the most hotly-debated topics in interventional cardiology as the safety and efficacy of SVG PCI remains suboptimal in comparison to native vessel PCI4-7. Embolisation of atherothrombotic debris, including friable lipid-rich plaque and platelet clumping, is common in SVG PCI, resulting in periprocedural myocardial infarction in as many as one-third of patients8-10 and leading to increased mortality at both short- and medium-term follow-up11-14. Moreover, it has been recently shown that in SVG patients even minimal elevation of periprocedural troponin may translate into increased mortality when compared with patients with native vessel PCI15. By limiting atheroembolism, the use of embolic protection devices has become standard-of-care during SVG PCI16-19 and multiple randomised trials have confirmed that this strategy is associated with a reduced rate of adverse events20-22. Filter-based baskets, in particular, have gained prominence due to their ease of deployment and limited technical requirements.
When filters are used, however, a transient impairment of epicardial flow after stenting has been observed in up to one-third of cases. This has been characterised as a reversible phenomenon, associated with higher amount of collected debris, and termed “filter no-reflow” (FNR23,24). FNR was first described in association with a single type of filter device (EPI FilterWire EX; Boston Scientific, Santa Clara, CA, USA), no longer available in the market. No data on the functional significance of FNR have been reported. Moreover, quantitative angiographic scoring of the SVG degeneration as a predictor of FNR has not been attempted.
The primary aim of our study was to identify the clinical and angiographic predictors of FNR in patients treated with SVG PCI using distal protection filters. We also tested whether FNR was associated with increased frequency of post-procedural troponin T (TnT) elevation at 24-48 hours, reflecting a type IVa myocardial infarction (MI) under the Universal Definition of Myocardial Infarction25.
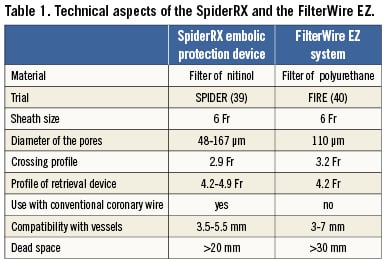
Finally we investigated the differential effect on FNR of the two most commonly used distal protection devices, the EPI FilterWire EZ™ (Boston Scientific, Natick, MA, USA), and the SpiderRX™ distal embolic protection system (Ev3, Plymouth, MN, USA).
Material and methods
Patients
Patients undergoing filter-assisted SVG PCI were retrospectively reviewed. Clinical, procedural and laboratory data were collected for all patents. Exclusion criteria were: cardiogenic shock, multivessel PCI, PCI performed on more than one SVG, vessels anatomically unsuitable for distal protection device, intra-procedural complications. Figure 1 summarises the study flow of patients. A local ethics committee approved the study and all patients enrolled signed informed consent. All procedures were followed in accordance with the ethical standards of the responsible committees on human experimentation and with the Helsinki Declaration.
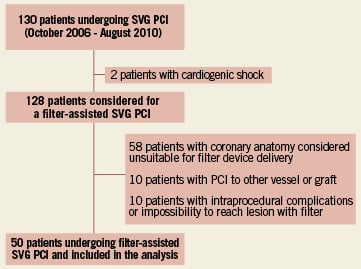
Figure 1. Flow chart of patients included in the study.
Percutaneous coronary intervention
PCI was performed with 6 Fr access via the radial or femoral route. Prior to PCI, all patients received 100 mg of aspirin and oral clopidogrel (with a loading dose of 600 mg if not already on clopidogrel) or ticlopidine 500 mg. Intravenous unfractionated heparin was administered to maintain procedural activated clotting time >300 sec. Use of the glycoprotein IIb/IIIa receptor antagonist abciximab was at the discretion of the operator. No patient had GPIIb/IIIa inhibition as a bailout for intra-procedural no reflow.
Angiographic analysis
Angiograms were blindly analysed by two experienced operators (F.B and I.P.), using quantitative coronary angiography (QCA) (CASS QCA 5.9; Pie Medical Imaging BV, Maastricht, The Netherlands). Measurements were made in a single projection showing the most severe stenosis using standard procedure; reference vessel diameter (RVD), minimal lumen diameter (MLD) and percent diameter stenosis were blindly measured pre- and post-procedure according to previously validated methods26. Thrombolysis In Myocardial Infarction (TIMI) flow grade was measured as previously reported both before and after the procedure27.
FNR was defined as an impaired graft flow during deployment of the filter, followed by a sudden increase of >1 TIMI flow grade immediately after device removal, in absence of pharmacological treatment between the two dye injections (Figure 2). To obtain quantitative data, and for improved standardisation, corrected TIMI frame count (c-TFC) was also measured in the same two cine-loops before and after device removal, and the difference calculated (?c-TFC28). Visual impression of FNR was calibrated to correspond to a ∆c-TFC ≥20. The extent of graft degeneration was analysed by means of “degeneration score” (DS), as previously described29. This is a semi-quantitative visual score ranging from zero to three, determined by estimating the degree of the graft containing luminal irregularities or ectasia, making up >20% of the reference normal segment and <25% (DS0), 26%-50% (DS 1), 51%-75% (DS 2) and >75% (DS 3) of the total SVG length29.
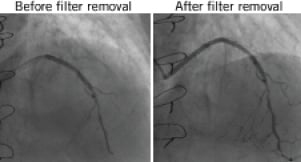
Figure 2. Example of FNR.
Periprocedural MI (type IVa MI) definition and troponin T assay
Troponin T was measured using Roche Diagnostics reagents on an Elecsys® 2010 immunoassay analyser (F. Hoffmann-La Roche Ltd, Basel, Switzerland). The criterion of coefficient of variation ≤10% in our lab was met by a TnT concentration of ≥0.03 ng/ml, although the lower detection limit was 0.01 ng/ml (99th percentile of reference control group). Troponin T was analysed at admission, before PCI and at 12- and 24-hour after PCI. Type IVa MI was defined as a rise of at least 0.03 mg/dl (>3 times the 99th percentile of the upper reference limit) in post-PCI TnT value in stable angina patients who had normal pre-PCI troponin values25. Periprocedural MI was defined as a pre-PCI TnT fall pattern followed by a post-PCI TnT rise of >20% in at least one out of two post-PCI determinations in non ST elevation MI (NSTEMI25).
Statistical analysis
Continuous variables are presented as mean±SD or median and interquartile range (IQR), and discrete variables are reported as counts and percentages. The differences between groups were assessed with a Fisher’s exact test for categorical variables and a Mann-Whitney U test for continuous variables. Correlations were calculated using a Spearman’s rank test. Myonecrosis and FNR predictors were assessed using a multivariate logistic regression model to estimate the odds ratios (OR) and corresponding 95% confidence intervals (CI 95%). First, a univariate analysis was performed including the variables that were predictive of major cardiovascular events after SVG PCI in the literature (MI on admission, graft age, graft DS, stent length, thrombotic burden, pre- and post-dilatation, use of GPIIb/IIIa antagonists5,23,30). Next, the variables with a probability value <0.05 were entered en bloc into the multivariate model, with age and gender as background variables.
Statistical analyses were performed using SPSS 17.0 software (SPSS Inc., Chicago, IL, USA) and statistical significance attributed to p-values <0.05.
Results
After exclusion criteria were applied, we analysed 50 consecutive patients (mean age 66±9.8 years, 47 males) who had SVG PCI at our institution between October 2006 and August 2010. Twenty-seven patients (54%), presented with non-ST elevation acute coronary syndromes (NSTE-ACS), while 23 (46%) presented with stable angina. Average graft age was 10.4±3.9 years. Total lesion length was 30.5±17.5 mm, while mean total stent length was 41.2±28 mm. Average DS of the SVG lesion was 1.6±0.9. During SVG PCI, FNR was present in 15 patients (30% of cases). GP IIb/IIIa antagonists were used from the start of the procedure in 26% of patients.
Distal protection devices used during PCI were: in 39 cases (78%) the FilterWire EZ, while in the remaining 11 patients (22%) the SpiderRX distal embolic protection system. The technical characteristics are illustrated in Table 1. When feasible (42 patients, 85%), the filter was passed directly beyond the lesion. Alternatively, pre-inflation with a small balloon (1.5 or 2 mm in diameter) was permitted in order to facilitate passage of the device.
Of note, despite the use of distal protection, evidence of type IVa post-procedural infarction was present in 18 patients (36%). No other in-hospital clinical major acute cardiac events (MACE) were observed.
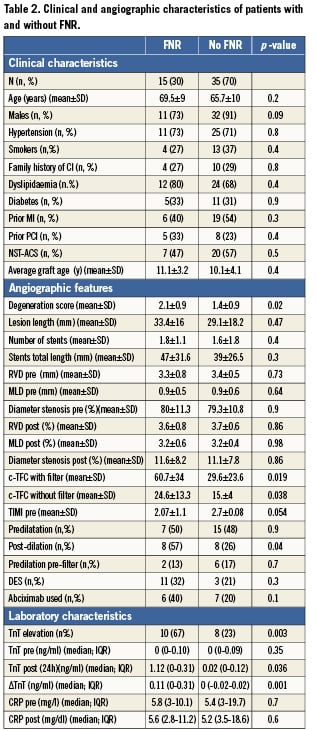
Predictors of FNR
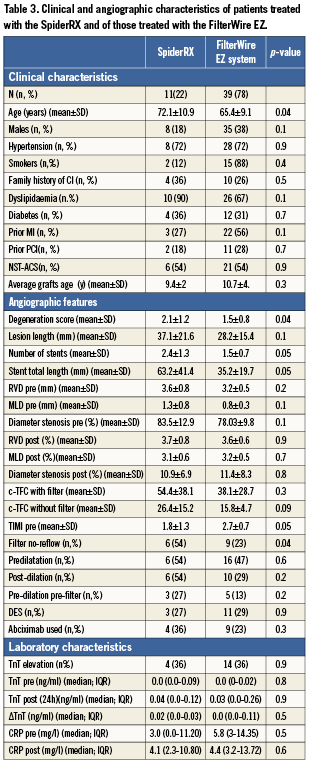
No difference in clinical characteristics was present between those with and without FNR after SVG PCI. Patients with FNR had a higher baseline SVG DS (2.1±0.9 vs. 1.4±0.8, p=0.02), confirming a more diffuse graft disease in this group. No difference was observed between the two groups regarding the number of implanted stents, percentage stenosis, RVD and MLD, both before and after PCI. Patients with FNR more frequently exhibited a type 4a MI after PCI (67% vs. 23%, p=0.003) and had a greater TnT elevation (0.11 ng/ml [CI 95%= 0-0.31] vs. 0.0 ng/ml [CI 95%= 0.02-0.02], p=0.001). Finally, the use of post-dilatation was significantly higher in the group of patients who subsequently developed FNR (57% vs. 26%, p=0.04). Patients’ clinical and angiographic characteristics are reported in details in Tables 2 and 3.
Comparison between filter devices
No difference regarding risk factors, history of past cardiovascular events (PCI or MI) was present, while FNR was observed more frequently in patients treated with the Spider than with the FilterWire EZ device (54% vs. 23%, p=0.04). However, in the group treated with the SpiderRX device, graft atherosclerosis disease was more diffuse (DS 2.1±1.2 vs. 1.5±0.8, p=0.04) and the number (2.4±1.3 vs. 1.5±0.7, p=0.05) and total length of implanted stents were significantly different (63.3±41.4 mm vs. 35.2±19.7 mm, p=0.005). There was no difference in the incidence of periprocedural myonecrosis, or raised C-reactive protein (CRP) between type of filter.
Multivariate analysis
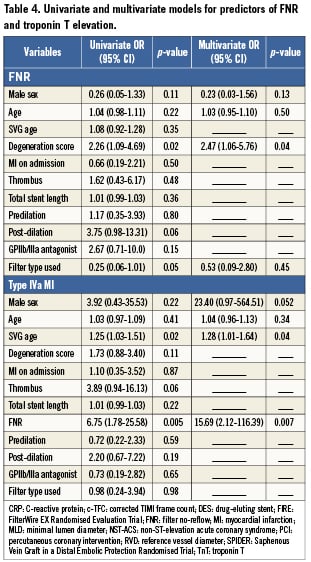
The graft DS was the only independent predictor of FNR at multivariate analysis (OR 2.47 [CI 95%= 1.06-5.76], p=0.04). The independent predictors of post-procedural TnT increase were the presence of FNR (OR 15.69 [CI 95%= 2.12-116.39], p=0.007) and the age of the treated graft (OR 1.28 [CI 95% 1.01-1.64], p=0.04) (Table 4).
Discussion
The main and novel findings of our study are as follows: 1) The temporary slowing down of flow when a filter device is used for embolic protection in SVG PCI, termed FNR, is mainly predicted by the degree of global degeneration of the graft, as expressed by DS; 2) FNR, already known to be a common occurrence in SVG PCI, is an independent predictor of type IVa MI, known to increase the risk of future adverse clinical events31; 3) The type of filter does not appear to independently predict either FNR or type IVa MI.
Regarding FNR prediction, our study reports the ability of DS to predict the occurrence of FNR, thus confirming the hypothesis that intervention to old, degenerated vein grafts, with a high DS, exposes the patient to an increased risk of intra-procedural complications such as FNR.
This finding is in line with our previous report23, where we observed that the presence of FNR was associated with a larger volume of debris “captured” by the older generation FilterWire EX, in a population which included both SVG and native vessel PCI. Mechanical occlusion of the filter pores due to the large quantity of embolised material is suspected to have a key role in the pathogenesis of FNR. In SVG, as opposed to native vessels, the quantity of material present in the filter and the presence of a filling defect within the filter were only modestly related with the presence of FNR22. This suggested that the simultaneous occurrence of macro and micro-embolisation of extremely small plaque fragments, able to pass through the filter pores, is particularly important in the pathogenesis of SVG FNR. Dilatation of degenerated SVG, which are known to contain very friable elements, may cause embolisation of particles with smaller dimensions than the pores of the filter system (100 µm), as well as of the pre-capillary arterioles, leading to coronary microcirculatory occlusion and subsequent myocardial damage. Indeed, analysis of aspirated material after SVG PCI conducted with electron-beam microscopy in the SAFER study showed that 64% of embolic material was smaller than 57 µm and 81% less than 96 µm32.
Another hypothesis formulated to explain the pathogenesis of FNR explores the possible role of humoral molecules released following plaque manipulation. These substances are able to pass freely through the barrier represented by the filter, can modify the vascular tone of the capillary bed, thereby stimulating the expression of adhesion molecules and platelet aggregation, causing alterations of flow and subsequent myocardial damage33. In support of the possible role executed by both these mechanisms in the pathogenesis of FNR, the utility of thrombus aspiration to prevent distal embolisation has been demonstrated in both primary and SVG PCI, in combination with occlusive distal balloons22,34. Combined occlusion-aspiration devices, however, have not been shown to be superior to basket filters35, and a recent report has also shown that additional thrombus aspiration does not decrease the incidence of SVG FNR36. These data point to a different pathogenesis for FNR, perhaps related to coronary and microvascular spasm induced by the filter itself.
There was an apparent difference in the rate of FNR between filter type, however this was explained by the different DS and stent length between the two groups. A multivariate analysis type of device was not an independent predictor of FNR. Any differential effect of the type of filter thus remains to be validated in larger comparative studies.
A recent pooled analysis of five randomised studies and one registry showed that, among clinical and angiographic parameters, the strongest predictor of cardiovascular events at one month after SVG PCI was the extent of degenerative disease in the SVG (corresponding to DS37). By reporting FNR as an independent predictor of type IVa MI, we propose that FNR, an intermediate angiographic endpoint readily recognisable during the procedure, could represent a useful high risk indicator of intra- and periprocedural complications.
The correlation between FNR and type IVa MI has important implications. FNR can be considered a marker of an embolism-prone lesion/patient, or alternatively FNR may be directly responsible for myocardial damage through prolonged ischaemia. FNR occurrence may identify higher risk patients at the time of SVG PCI, who could benefit from more prolonged observation, or from additional medical treatments, such as increased anti-ischaemic therapy or more powerful antiplatelet drugs.
Limitations
We recognise the modest sample size and the retrospective nature of our analysis as limitations of our study. However, few comparisons of filter devices are available in the literature, and, to the best of our knowledge, no study has so far compared the effects of different designs on intra-procedural complications and their significance.
As periprocedural necrosis was defined according to TnT increase, we could not provide data about creatine-kinase MB levels after PCI. However, we believe that TnT elevation is more substantiated as a predictor of adverse prognosis in the field of SVG interventions41.
Conclusions
FNR observed during SVG PCI is a multifactorial phenomenon, the causes of which are only partially understood. It occurs in grafts with a higher degeneration score, and does not seem to be independently linked with the type of filter device used. The mechanisms of FNR require further exploration, as factors other than solely macro-embolisation of particles could be involved in its pathogenesis. The occurrence of FNR is clinically relevant as a strong predictor for subsequent myocardial damage after SVG PCI. Patients with FNR may be identified as being at higher risk of distal embolisation, and requiring a more aggressive therapy in the post-procedural period.
Acknowledgements
The authors would like to thank the Coronary Care Unit and Catheterisation Lab staff of the “Policlinico A. Gemelli”, Catholic University of the Sacred Heart, Rome, Italy, for their invaluable help, support and patience.
Conflict of interest statement
C. Hamilton-Craig is supported by the National Heart Foundation of Australia and the University of Washington Trans-Pacific Fellowship. These funding bodies had no involvement in data analysis or manuscript writing. The authors have no conflicts of interest to declare.

