Coronary no-reflow is observed in >20% of patients undergoing primary percutaneous coronary intervention (PCI) for ST-segment elevation myocardial infarction (STEMI) and in <2% of patients undergoing elective PCI1. No-reflow typically occurs in the setting of primary PCI after recanalisation of an occluded coronary artery and may be explained by microvascular obstruction caused by ischaemia and reperfusion-related cell injury, which may be exacerbated by intervention-induced distal embolisation of thrombotic material. Nonetheless, no-reflow may also occur following PCI in non-infarct-related arteries (for example, during elective PCI), primarily due to PCI-related distal embolisation of atherosclerotic/thrombotic material leading to microcirculation clogging1. Irrespective of the underlying mechanism, no-reflow is associated with poor prognosis2. While microvascular obstruction is the principal mechanism of no-reflow, the pathophysiology of this phenomenon is complex and not fully understood3-5. No-reflow is a dynamic condition which seems to resolve spontaneously in 50% of patients by one month6 and in 80% of patients by six months7 after primary PCI. However, the impact of transient no-reflow on long-term clinical outcome remains poorly investigated.
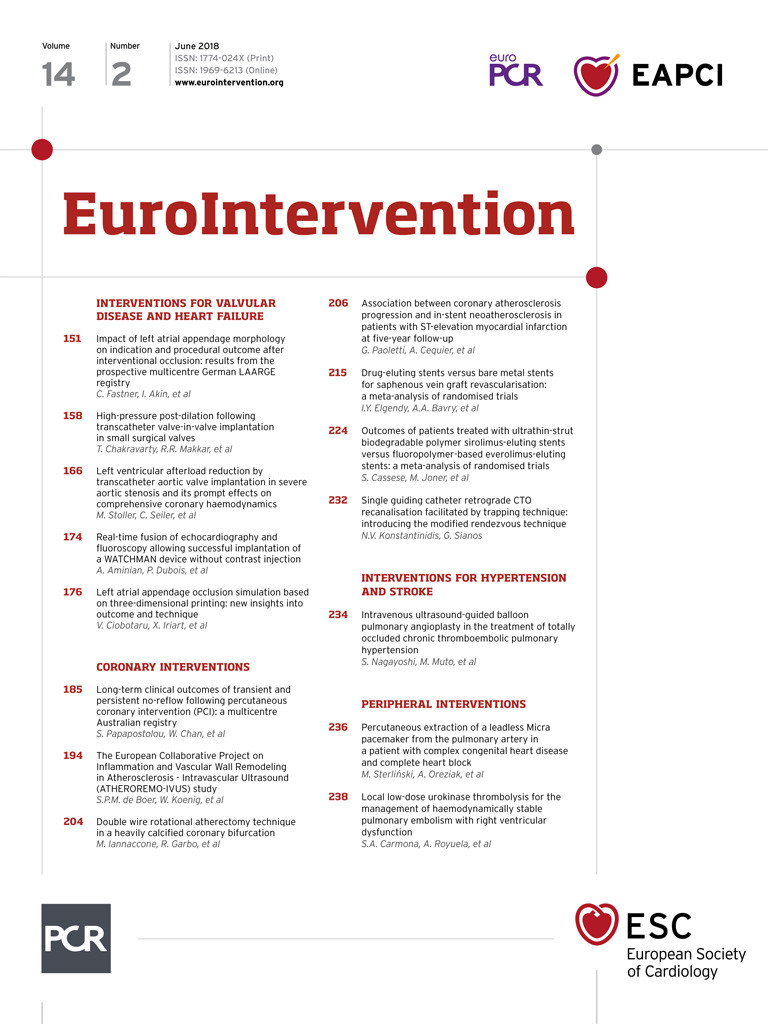
In this issue of EuroIntervention, Papapostolou et al8 assess the association of transient or persistent angiographic no-reflow with long-term outcomes across the whole spectrum of patients with coronary artery disease (CAD) undergoing PCI.
By design, the study was a registry-based retrospective analysis of 18,281 patients who underwent PCI for stable CAD or acute coronary syndrome. Persistent no-reflow was defined as Thrombolysis In Myocardial Infarction (TIMI) flow grade ≤2 in the absence of residual coronary stenosis, dissection or spasm that persisted at the end of the PCI procedure. Transient no-reflow was defined as a temporary reduction in epicardial flow (TIMI flow grade ≤2) at any time following initial restoration of blood flow, which resolved by the end of the procedure. Overall, the frequency of no-reflow was 4% (n=734), comprising transient and persistent no-reflow in 3.2% and 0.8% of patients, respectively. The main finding was that, compared with normal flow, transient and persistent no-reflow were associated with stepwise higher rates of in-hospital and 30-day all-cause mortality, major adverse cardiovascular events (MACE) and heart failure, as well as higher rates of one-year all-cause and cardiovascular mortality, MACE and readmissions for heart failure. Importantly, the higher rate of all-cause mortality in patients with no-reflow persisted at five years - 22% in patients with transient no-reflow and 31% in patients with persistent no-reflow compared with 14% in patients with normal (TIMI grade 3) blood flow. After multivariable adjustment, transient or persistent no-reflow was associated with a 30% and 50% higher adjusted risk for long-term mortality, respectively. Likewise, multivariable models with no-reflow showed a good discriminatory power with respect to prediction of long-term outcomes8.
The authors should be congratulated for conducting this study. The study confirms and extends findings from previous studies, with the strength of assessing the association between no-reflow and adverse outcomes in a large number of patients at several time points after PCI, from the index hospitalisation to multiple years of follow-up. The finding that no-reflow during PCI - even if transient - is associated with poor prognosis expands the limited existing evidence linking no-reflow with adverse events after primary PCI9 and highlights the importance of recognising this phenomenon during PCI procedures.
As the authors emphasise, the study has limitations inherent to its retrospective observational design, somewhat outdated antithrombotic therapy, lack of information on use and/or choice of drugs to treat no-reflow, and the use of insensitive criteria to diagnose no-reflow. Nonetheless, these limitations are unlikely to impact on the main study findings. However, some caveats should be mentioned. First, the study included patients across the whole spectrum of CAD, from stable CAD to STEMI. Depending on their clinical presentation, patients differ with respect to their outcomes after PCI, frequency, and potential mechanisms of no-reflow1. Thus, the overall frequency of no-reflow across such a heterogeneous group of patients may not reflect the true frequency of no-reflow in each patient subgroup. Second, although angiographic (TIMI flow grade) criteria are commonly used to assess no-reflow after PCI, they lack sensitivity to detect no-reflow after PCI, which might explain why the reported frequencies of transient and persistent no-reflow were so low in the current study. It has been shown that, despite grade 3 TIMI flow, a sizeable proportion of patients after PCI have impaired tissue reperfusion due to microvascular obstruction. Indeed, up to 60% of STEMI patients with optimal angiographic reperfusion indices (TIMI flow and blush grade of 3) show no-reflow on magnetic resonance imaging in the 72 hours after the acute event10. Third, fluctuations of coronary blood flow immediately after flow restoration are relatively common and may not necessarily represent no-reflow, per se. Considering the profound alterations at the level of the microcirculation and surrounding myocardium responsible for microvascular obstruction and no-reflow, resolution of true no-reflow at the end of the PCI procedure would seem unlikely. Previous studies have shown that it may take days or even months for no-reflow to resolve spontaneously6,7. Coronary flow fluctuations may reflect vasoconstriction induced by release of vasoconstrictive substances – particularly thromboxane A2 and serotonin – when thrombus is squeezed against the vessel wall during balloon dilatation. Fourth, the end of the PCI procedure may not be the ideal time point to assess no-reflow. Experimental studies have shown that the zone of microvascular obstruction and no-reflow expands progressively over several hours or days11,12 after blood flow restoration, potentially reflecting the time needed to obstruct the microcirculation by platelets, neutrophils, endothelial and cardiomyocyte oedema. Thus, whether fluctuations in the coronary blood flow during PCI herald the development of no-reflow post procedure remains to be explored. If this were the case, it may explain the poor outcomes of patients with transient no-reflow observed in the current study.
In summary, the study by Papapostolou et al clearly shows that no-reflow during PCI – even when transient – is associated with poor short- and long-term outcomes. The study underlines the importance of detecting no-reflow during PCI across the whole spectrum of patients with CAD. Such patients may warrant closer surveillance as well as strict implementation of secondary prevention measures after PCI.
Conflict of interest statement
The authors have no conflicts of interest to declare.